User login
The past year has seen the publication of four studies with relevance for clinicians:
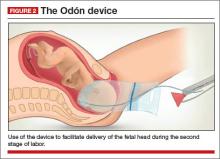
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
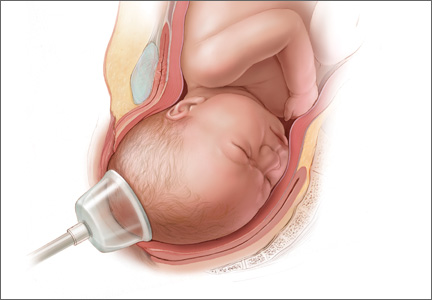
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
The past year has seen the publication of four studies with relevance for clinicians:
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
The past year has seen the publication of four studies with relevance for clinicians:
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
Have you read the June Guest Editorial? Click here to access Dr. John T. Repke's Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”?