User login
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
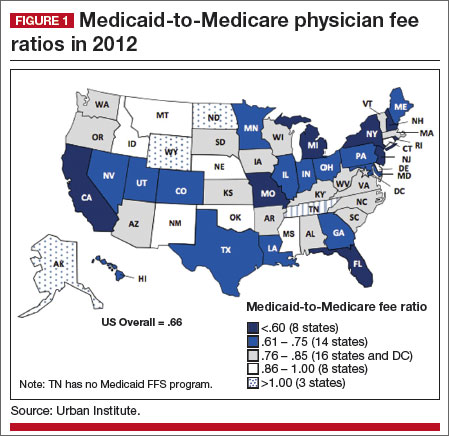
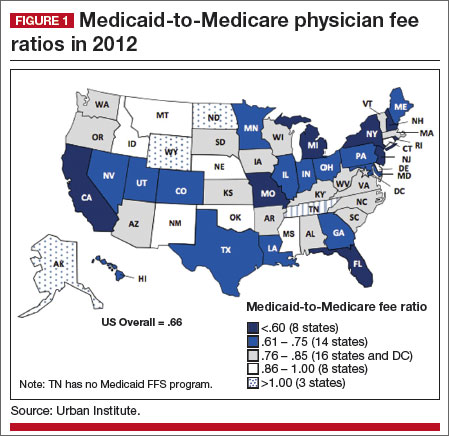
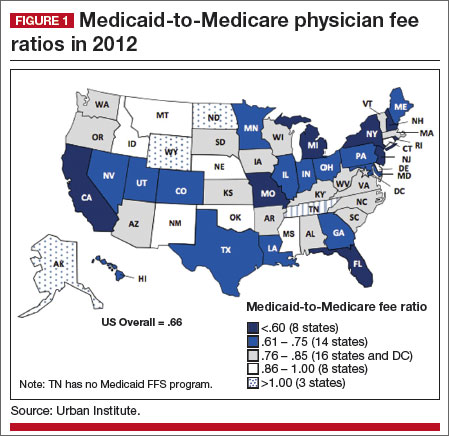
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
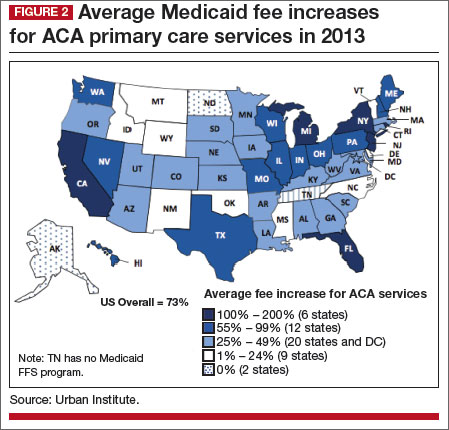
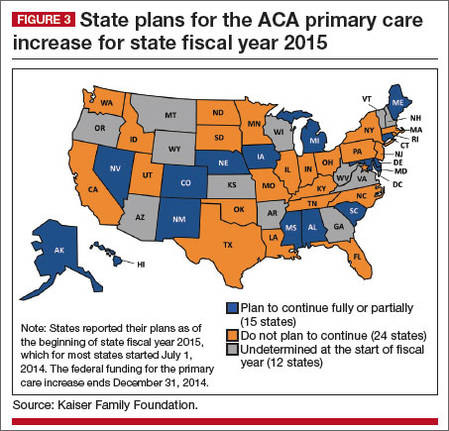
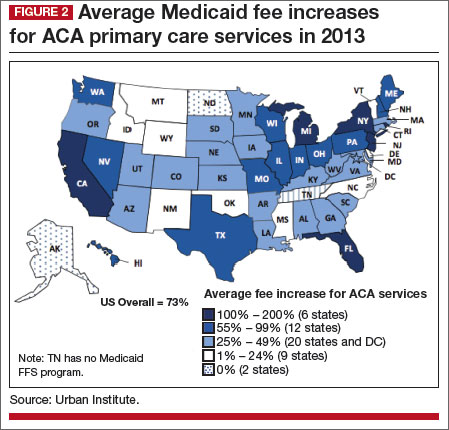
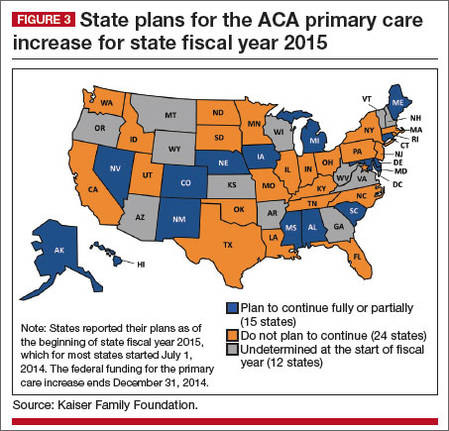
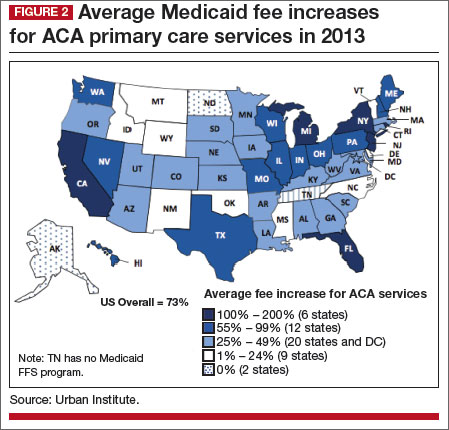
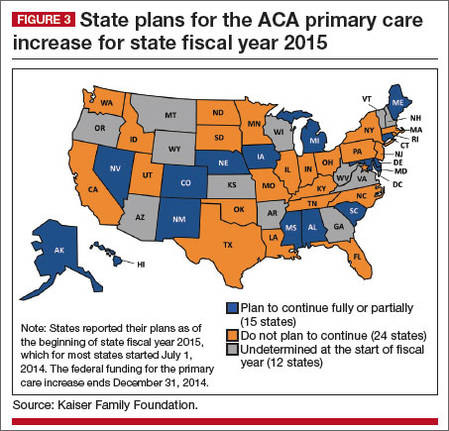
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
   |
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
   |
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
   |
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.


