User login
Disclaimer: SHM Members William Atchley, MD, FACP, Ron Greeno, MD, Stacy Goldsholl, MD, and Mark V. Williams, MD, FACP, are quoted in this article. Their opinions do not reflect or represent the opinions of SHM.
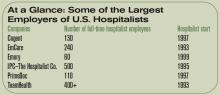
Hospital medicine may be a young field, but several major providers have already been established. Each of these rapidly growing organizations employs dozens—or even hundreds—of hospitalists and is establishing or revamping hospital medicine programs across the United States.
As these organizations grow, they are shaping hospital medicine. “I think that what the large companies really bring to the table is a vision of what hospital medicine is supposed to be about: evidence-based medicine and other things important to the hospital,” says William Atchley, MD, FACP, a practicing hospitalist in Hampton, Va.
This month, we examine just a few of the many large hospital medicine groups in order to set the stage for this growing trend and the issues presented by these groups. That said, here is an overview of some of the largest national players in hospital medicine, their perspective on the industry, their philosophies, and dialogue about their astonishing growth.
The Players
Which organizations have become the nation’s largest employers of hospitalists?
Cogent Healthcare
Based in Irvine, Calif., Cogent employs approximately 130 full-time hospitalists, with an additional 70 who “work with us in other arrangements; some are partnered with us,” says Ron Greeno, MD, FCCP, Cogent chief medical officer.
Cogent was founded by four physician groups in Los Angeles County. “We started in late 1997 and spent the first several years developing the model,” recalls Dr. Greeno. “In the 2000s, we started building programs for hospitals. We’ve seen growth of around 40% a year for the last several years. Frankly, we started too early; the market wasn’t really ready.”
What sets Cogent apart, says Dr. Greeno, is its focus. “We’re not a physician practice management company,” he stresses. “Our competitors’ goal is to build large, successful practices. We built a practice that’s hospital-centric. This helps the hospital satisfy its goals.”
EmCare
Perhaps the first of the national players to actively undertake hospital medicine, EmCare developed its first hospitalist program in 1993 at Baylor University Medical Center (BUMC) in Texas. “[Baylor is] still with us,” says Michael Wagner, MD, CEO, Hospitalists Division, EmCare.
EmCare has more than 30 years of experience with emergency department (ED) staffing, which is how it got its foot in the hospitalist door.
“In the late ’90s, other hospital EDs talked to us” about bringing in a hospitalist program, says Dr. Wagner. “So in each ED region, we worked to sell [the] hospital medicine program. It didn’t really take off until the 2000s, when non-clients started approaching us.”
Today, EmCare employs 350 hospitalists, 240 of whom work full-time. They provide hospital medicine to 47 clients in 60 programs in 37 states.
Emory Healthcare
Emory Healthcare’s Hospital Medicine Unit in Atlanta is the largest academic hospital medicine program in the United States.
“We occupy five hospitals,” says Mark V. Williams, MD, FACP, director of Emory’s Hospital Medicine Unit and editor of the Journal of Hospital Medicine. “Thirty of our hospitalists teach at the two university hospitals, and an additional eight teach at [one of three] community hospital[s]. Others will teach in-service training as well.”
The two university hospitals—Emory University Hospital and Crawford Long Hospital—are “solely staffed by Emory physicians,” explains Dr. Williams. “A third of what we do in these settings is teaching, and the rest is direct care.”
The university’s hospitalist program started in 1999 with eight hospitalists; today, it employs 60. The difference with an academic hospitalist program, explains Dr. Williams, is that “we’re essentially dealing with staffing teaching teams, teaching, and having research components.”
IPC–The Hospitalist Company
Perhaps the best-known hospitalist employer, IPC (North Hollywood, Calif.) currently has approximately 500 full-time employed hospitalists and 150-200 part-timers working in more than 200 facilities across 23 U.S. markets.
“We have every type of practice, including academic and small hospitals,” says Adam D. Singer, MD, chairman, CEO, and chief medical officer of IPC. The company was re-incorporated in 1995. “We started accelerating in ’97, and we’ve been growing 30 to 50% per year—steady growth. We’re acquiring like-minded groups. We’ve had 10 acquisitions in the last 24 months. All our acquisitions have to be high-minded, quality groups.”
PrimeDoc
Based in Asheville, N.C., PrimeDoc is 100% physician-owned and managed. Counting permanent employees as well as independent contractors, the company staffs approximately 110 hospitalists.
“We do things a little differently,” says Robert J. Reynolds, MD, president and CEO, who also co-founded PrimeDoc in 1997. “We started as a freestanding practice serving one hospital, and we use a private practice model today. We’ve grown by establishing private practices in five states along the Atlantic seaboard.”
Dr. Reynolds admits that the PrimeDoc model is not “terribly unique. We contract with hospitals to provide care to unassigned patients, and we solicit referrals from [primary care physicians] in the community.”
TeamHealth Hospital Medicine
Another company that started out providing ED services—as well as administrative and staffing services—TeamHealth (Wilmington, N.C.) now employees more than 400 hospitalists, most of whom are full-time employees.
“Until this past year, I think we’ve been a little bit of a sleeper in hospital medicine,” says Stacy Goldsholl, MD, president. “That’s all changing now, as we’re aggressively pursuing the number-one place in the market. But we’ve grown as a silent presence through our relational reputations—basically, through word of mouth in the emergency departments. We have more than 400 contracts [in emergency medicine].”
The company continues to add hospital medicine programs through several methods. “We set up new programs from scratch, we restructure existing programs, we acquire large hospital medicine groups,” says Dr. Goldsholl, “and we apply things that work in one model to other models.”
Growth Trends
One feature these organizations have in common: explosive growth. The corporations are acquiring, starting, or partnering with a steady stream of hospital medicine programs.
“We’ve more than doubled in the last year,” says Dr. Goldsholl. “Our pipeline for hospital medicine groups is just exploding. We’re trying to manage the growth we have as well as what’s coming. We hope to double again in the next two years.”
Within that increase in programs comes another growth trend: hospital clients are asking their hospital medicine groups to take on more responsibility. “Our role in the hospital setting is definitely expanding,” says Dr. Goldsholl. “And the hospitalist’s role is only going to increase. We’ll see more hospital-based intensivists, surgicalists, and laborists [OB/GYN physicians]—there’s tremendous growth coming.”
Dr. Reynolds agrees. “In 1997, we basically provided medical care for acute care patients,” he explains. “Now we’re providing care for surgical care patients. We do pre-op eval[uation]s and perioperative management. We’ve also seen more demand for rapid response management, and we’re being asked to do pre-op eval[uation]s for outpatient surgeries.”
More hospitals are proactively seeking out these market leaders to explore adding a new hospital medicine program. “We’re getting calls from smaller and smaller hospitals,” says Dr. Reynolds. “Even the smallest hospitals want to implement a hospital medicine program, and it’s difficult to provide 24-hour coverage and have it make sense financially. But the trend is promising: Every hospital wants this type of service.”
Will these big players gobble up independent programs? That depends on how those programs are doing. “I haven’t heard of any programs being replaced if they’re doing all the right things and their costs are in line,” according to Dr. Atchley. “What you’re seeing is national companies either starting programs or salvaging programs that have failed.”
Industry Trends
Managing a large number of hospital medicine programs provides these companies with a clearer view of what’s happening in the specialty as it grows and changes. One trend that they’re seeing is a sort of second phase, where hospitals that brought in hospitalists several years ago now seek to improve their programs.
“In the past year, we’ve seen [hospitals express] more need, more interest in a hospital medicine management company coming in and restructuring a struggling program or a failed program,” says Dr. Goldsholl.
EmCare observes the same trend. “Hospitals are a lot savvier than they were five or 10 years ago about the setup of a hospital medicine program,” says Dr. Wagner. “Some [hospital administrators] may be on their second or third program, and they know what they want. They ask about recruitment success, retention rates, your data gathering and reporting tools, and what you do specifically to support your physicians in terms of leadership, quality, and satisfaction.”
These expectations are not simply discussed; they become part of the contractual agreement. “Hospitals also want service deliverables written in the contract,” adds Dr. Wagner, “including physician performance in terms of patient satisfaction, primary care physician satisfaction, JCAHO core measures, and medical staff participation.”
Why Big May Be Better
A large group with an established infrastructure that includes standards for quality checks, patient satisfaction, and so on is appealing to hospitals. “Because of economies of scale, we can offer state-of-the-art technologies, billing and collection, and infrastructure,” says Dr. Singer. “We also have the ability to recruit physicians. Small groups cannot compete with that.”
Another attractive feature is the history that these groups have in a relatively new field. “We have a track record of setting up successful programs,” points out Dr. Reynolds. ”We’ve already learned from our mistakes.”
Working for a national corporation has its benefits, including opportunities for education and advancement and an infrastructure support that can take some of the workload off a hospitalist’s shoulders. Dr. Greeno points out that Cogent handles administrative work for the physicians, freeing up their time for patients.
“One guy said, ‘I like working here because it’s the best opportunity to practice pure medicine,’ ” he says. “Our physicians are not case managers; they’re not schedulers.”
And working as part of a large group provides a built-in network of colleagues. “There’s connectivity for the individual hospitalist, as well as the medical director, to learn from other hospitalists all over the country,” says Dr. Goldsholl.
Dr. Wagner names compliance as one of EmCare’s top benefits. “We code physician notes professionally, and the result is we have greater than 95% compliance with Medicare. That’s something a national company can bring to the table.”
Some say that a large organization may be more attractive to job candidates. “Our size demonstrates stability to candidates,” says Dr. Williams. “Recruiting is a 100%-a-year job, and this helps.”
He points out that a larger program can appeal to the hospitalists within it: “Another advantage to our size is that we can draw from a pool of physicians to help out if necessary.”
Of course, physicians who work for larger companies may enjoy a larger compensation package, which can benefit the entire specialty. “In my experience, when [large companies] have come into my area, their salary structure is higher,” says Dr. Atchley. “The result is that other groups in the region have to change their salaries to be more competitive.”
The Upside to Independents
One factor that helps hospitals decide between bringing in a national company and using an independent local group is the cost.
“[Local programs] may not be as expensive as the large groups,” says Dr. Atchley. “When my hospital sent out an RFP [request for proposal], we saw that some of our costs were much less than what a national company” has to charge.
One major concern individual hospitalists and smaller groups may have regarding employment in a national corporation is loss of autonomy. Would they be expected to follow rigid rules and regulations set forth by a distant corporation office? The leaders in those offices say no, absolutely not.
“We actually manage down to a small practice,” says Dr. Singer. “Concerns are that there will be a loss of autonomy; that’s not true.”
Regardless of which type of hospital medicine program one prefers, having options is good for both the hospital and the physician. “Competition is good,” maintains Dr. Atchley. “When these companies come in, they’ll definitely provide superior infrastructure and can track outcomes. Homegrown hospital medicine programs should use the same approach.”
A Glimpse of the Future
Will all hospitalists eventually work for a behemoth corporation? Not a chance, say the CEOs and CMOs of the current hospital medicine company leaders. “There are lessons to be learned from the emergency department,” says Dr. Wagner. “Large companies don’t have the majority of ED contracts. There’s only so much [large companies] can manage before it starts to get picked off by smaller, younger practices that are more nimble and quick to respond.
“All the big players won’t be dominant from a market-share point of view,” he adds. “But what they will do is set expectations for good hospital medicine practices.”
However, the employment model for hospitalists will continue to change. “We’re going to see existing [large] companies increase their regional presence,” predicts Dr. Reynolds. “The hospital-owned model will fade away. Physicians make lousy hospital employees—they just don’t fit into the hospital’s view of an employee.”
Dr. Atchley agrees with this point: “We’ll probably see fewer and fewer programs where the physician is employed by the hospital. That’s pretty much what the SHM surveys are showing.”
And when will the booming market for hospitalists start to slow? “I see [the market] growing well beyond my crystal ball,” says Dr. Singer. “I see a soon-to-be emerging trend of hospitals wanting hospitalists rather than internists. More groups are going to step up and add that—make an internist into a subspecialist. It’s a new way of thinking.”
Even without a crystal ball, leaders in hospital medicine forecast that the field will continue to grow and that hospitalists will become better trained, credentialed, and accepted as a specialty—regardless of what type of organization they work for. TH
Jane Jerrard writes “Career Development” and “Public Policy” for The Hospitalist.
Disclaimer: SHM Members William Atchley, MD, FACP, Ron Greeno, MD, Stacy Goldsholl, MD, and Mark V. Williams, MD, FACP, are quoted in this article. Their opinions do not reflect or represent the opinions of SHM.
Hospital medicine may be a young field, but several major providers have already been established. Each of these rapidly growing organizations employs dozens—or even hundreds—of hospitalists and is establishing or revamping hospital medicine programs across the United States.
As these organizations grow, they are shaping hospital medicine. “I think that what the large companies really bring to the table is a vision of what hospital medicine is supposed to be about: evidence-based medicine and other things important to the hospital,” says William Atchley, MD, FACP, a practicing hospitalist in Hampton, Va.
This month, we examine just a few of the many large hospital medicine groups in order to set the stage for this growing trend and the issues presented by these groups. That said, here is an overview of some of the largest national players in hospital medicine, their perspective on the industry, their philosophies, and dialogue about their astonishing growth.
The Players
Which organizations have become the nation’s largest employers of hospitalists?
Cogent Healthcare
Based in Irvine, Calif., Cogent employs approximately 130 full-time hospitalists, with an additional 70 who “work with us in other arrangements; some are partnered with us,” says Ron Greeno, MD, FCCP, Cogent chief medical officer.
Cogent was founded by four physician groups in Los Angeles County. “We started in late 1997 and spent the first several years developing the model,” recalls Dr. Greeno. “In the 2000s, we started building programs for hospitals. We’ve seen growth of around 40% a year for the last several years. Frankly, we started too early; the market wasn’t really ready.”
What sets Cogent apart, says Dr. Greeno, is its focus. “We’re not a physician practice management company,” he stresses. “Our competitors’ goal is to build large, successful practices. We built a practice that’s hospital-centric. This helps the hospital satisfy its goals.”
EmCare
Perhaps the first of the national players to actively undertake hospital medicine, EmCare developed its first hospitalist program in 1993 at Baylor University Medical Center (BUMC) in Texas. “[Baylor is] still with us,” says Michael Wagner, MD, CEO, Hospitalists Division, EmCare.
EmCare has more than 30 years of experience with emergency department (ED) staffing, which is how it got its foot in the hospitalist door.
“In the late ’90s, other hospital EDs talked to us” about bringing in a hospitalist program, says Dr. Wagner. “So in each ED region, we worked to sell [the] hospital medicine program. It didn’t really take off until the 2000s, when non-clients started approaching us.”
Today, EmCare employs 350 hospitalists, 240 of whom work full-time. They provide hospital medicine to 47 clients in 60 programs in 37 states.
Emory Healthcare
Emory Healthcare’s Hospital Medicine Unit in Atlanta is the largest academic hospital medicine program in the United States.
“We occupy five hospitals,” says Mark V. Williams, MD, FACP, director of Emory’s Hospital Medicine Unit and editor of the Journal of Hospital Medicine. “Thirty of our hospitalists teach at the two university hospitals, and an additional eight teach at [one of three] community hospital[s]. Others will teach in-service training as well.”
The two university hospitals—Emory University Hospital and Crawford Long Hospital—are “solely staffed by Emory physicians,” explains Dr. Williams. “A third of what we do in these settings is teaching, and the rest is direct care.”
The university’s hospitalist program started in 1999 with eight hospitalists; today, it employs 60. The difference with an academic hospitalist program, explains Dr. Williams, is that “we’re essentially dealing with staffing teaching teams, teaching, and having research components.”
IPC–The Hospitalist Company
Perhaps the best-known hospitalist employer, IPC (North Hollywood, Calif.) currently has approximately 500 full-time employed hospitalists and 150-200 part-timers working in more than 200 facilities across 23 U.S. markets.
“We have every type of practice, including academic and small hospitals,” says Adam D. Singer, MD, chairman, CEO, and chief medical officer of IPC. The company was re-incorporated in 1995. “We started accelerating in ’97, and we’ve been growing 30 to 50% per year—steady growth. We’re acquiring like-minded groups. We’ve had 10 acquisitions in the last 24 months. All our acquisitions have to be high-minded, quality groups.”
PrimeDoc
Based in Asheville, N.C., PrimeDoc is 100% physician-owned and managed. Counting permanent employees as well as independent contractors, the company staffs approximately 110 hospitalists.
“We do things a little differently,” says Robert J. Reynolds, MD, president and CEO, who also co-founded PrimeDoc in 1997. “We started as a freestanding practice serving one hospital, and we use a private practice model today. We’ve grown by establishing private practices in five states along the Atlantic seaboard.”
Dr. Reynolds admits that the PrimeDoc model is not “terribly unique. We contract with hospitals to provide care to unassigned patients, and we solicit referrals from [primary care physicians] in the community.”
TeamHealth Hospital Medicine
Another company that started out providing ED services—as well as administrative and staffing services—TeamHealth (Wilmington, N.C.) now employees more than 400 hospitalists, most of whom are full-time employees.
“Until this past year, I think we’ve been a little bit of a sleeper in hospital medicine,” says Stacy Goldsholl, MD, president. “That’s all changing now, as we’re aggressively pursuing the number-one place in the market. But we’ve grown as a silent presence through our relational reputations—basically, through word of mouth in the emergency departments. We have more than 400 contracts [in emergency medicine].”
The company continues to add hospital medicine programs through several methods. “We set up new programs from scratch, we restructure existing programs, we acquire large hospital medicine groups,” says Dr. Goldsholl, “and we apply things that work in one model to other models.”
Growth Trends
One feature these organizations have in common: explosive growth. The corporations are acquiring, starting, or partnering with a steady stream of hospital medicine programs.
“We’ve more than doubled in the last year,” says Dr. Goldsholl. “Our pipeline for hospital medicine groups is just exploding. We’re trying to manage the growth we have as well as what’s coming. We hope to double again in the next two years.”
Within that increase in programs comes another growth trend: hospital clients are asking their hospital medicine groups to take on more responsibility. “Our role in the hospital setting is definitely expanding,” says Dr. Goldsholl. “And the hospitalist’s role is only going to increase. We’ll see more hospital-based intensivists, surgicalists, and laborists [OB/GYN physicians]—there’s tremendous growth coming.”
Dr. Reynolds agrees. “In 1997, we basically provided medical care for acute care patients,” he explains. “Now we’re providing care for surgical care patients. We do pre-op eval[uation]s and perioperative management. We’ve also seen more demand for rapid response management, and we’re being asked to do pre-op eval[uation]s for outpatient surgeries.”
More hospitals are proactively seeking out these market leaders to explore adding a new hospital medicine program. “We’re getting calls from smaller and smaller hospitals,” says Dr. Reynolds. “Even the smallest hospitals want to implement a hospital medicine program, and it’s difficult to provide 24-hour coverage and have it make sense financially. But the trend is promising: Every hospital wants this type of service.”
Will these big players gobble up independent programs? That depends on how those programs are doing. “I haven’t heard of any programs being replaced if they’re doing all the right things and their costs are in line,” according to Dr. Atchley. “What you’re seeing is national companies either starting programs or salvaging programs that have failed.”
Industry Trends
Managing a large number of hospital medicine programs provides these companies with a clearer view of what’s happening in the specialty as it grows and changes. One trend that they’re seeing is a sort of second phase, where hospitals that brought in hospitalists several years ago now seek to improve their programs.
“In the past year, we’ve seen [hospitals express] more need, more interest in a hospital medicine management company coming in and restructuring a struggling program or a failed program,” says Dr. Goldsholl.
EmCare observes the same trend. “Hospitals are a lot savvier than they were five or 10 years ago about the setup of a hospital medicine program,” says Dr. Wagner. “Some [hospital administrators] may be on their second or third program, and they know what they want. They ask about recruitment success, retention rates, your data gathering and reporting tools, and what you do specifically to support your physicians in terms of leadership, quality, and satisfaction.”
These expectations are not simply discussed; they become part of the contractual agreement. “Hospitals also want service deliverables written in the contract,” adds Dr. Wagner, “including physician performance in terms of patient satisfaction, primary care physician satisfaction, JCAHO core measures, and medical staff participation.”
Why Big May Be Better
A large group with an established infrastructure that includes standards for quality checks, patient satisfaction, and so on is appealing to hospitals. “Because of economies of scale, we can offer state-of-the-art technologies, billing and collection, and infrastructure,” says Dr. Singer. “We also have the ability to recruit physicians. Small groups cannot compete with that.”
Another attractive feature is the history that these groups have in a relatively new field. “We have a track record of setting up successful programs,” points out Dr. Reynolds. ”We’ve already learned from our mistakes.”
Working for a national corporation has its benefits, including opportunities for education and advancement and an infrastructure support that can take some of the workload off a hospitalist’s shoulders. Dr. Greeno points out that Cogent handles administrative work for the physicians, freeing up their time for patients.
“One guy said, ‘I like working here because it’s the best opportunity to practice pure medicine,’ ” he says. “Our physicians are not case managers; they’re not schedulers.”
And working as part of a large group provides a built-in network of colleagues. “There’s connectivity for the individual hospitalist, as well as the medical director, to learn from other hospitalists all over the country,” says Dr. Goldsholl.
Dr. Wagner names compliance as one of EmCare’s top benefits. “We code physician notes professionally, and the result is we have greater than 95% compliance with Medicare. That’s something a national company can bring to the table.”
Some say that a large organization may be more attractive to job candidates. “Our size demonstrates stability to candidates,” says Dr. Williams. “Recruiting is a 100%-a-year job, and this helps.”
He points out that a larger program can appeal to the hospitalists within it: “Another advantage to our size is that we can draw from a pool of physicians to help out if necessary.”
Of course, physicians who work for larger companies may enjoy a larger compensation package, which can benefit the entire specialty. “In my experience, when [large companies] have come into my area, their salary structure is higher,” says Dr. Atchley. “The result is that other groups in the region have to change their salaries to be more competitive.”
The Upside to Independents
One factor that helps hospitals decide between bringing in a national company and using an independent local group is the cost.
“[Local programs] may not be as expensive as the large groups,” says Dr. Atchley. “When my hospital sent out an RFP [request for proposal], we saw that some of our costs were much less than what a national company” has to charge.
One major concern individual hospitalists and smaller groups may have regarding employment in a national corporation is loss of autonomy. Would they be expected to follow rigid rules and regulations set forth by a distant corporation office? The leaders in those offices say no, absolutely not.
“We actually manage down to a small practice,” says Dr. Singer. “Concerns are that there will be a loss of autonomy; that’s not true.”
Regardless of which type of hospital medicine program one prefers, having options is good for both the hospital and the physician. “Competition is good,” maintains Dr. Atchley. “When these companies come in, they’ll definitely provide superior infrastructure and can track outcomes. Homegrown hospital medicine programs should use the same approach.”
A Glimpse of the Future
Will all hospitalists eventually work for a behemoth corporation? Not a chance, say the CEOs and CMOs of the current hospital medicine company leaders. “There are lessons to be learned from the emergency department,” says Dr. Wagner. “Large companies don’t have the majority of ED contracts. There’s only so much [large companies] can manage before it starts to get picked off by smaller, younger practices that are more nimble and quick to respond.
“All the big players won’t be dominant from a market-share point of view,” he adds. “But what they will do is set expectations for good hospital medicine practices.”
However, the employment model for hospitalists will continue to change. “We’re going to see existing [large] companies increase their regional presence,” predicts Dr. Reynolds. “The hospital-owned model will fade away. Physicians make lousy hospital employees—they just don’t fit into the hospital’s view of an employee.”
Dr. Atchley agrees with this point: “We’ll probably see fewer and fewer programs where the physician is employed by the hospital. That’s pretty much what the SHM surveys are showing.”
And when will the booming market for hospitalists start to slow? “I see [the market] growing well beyond my crystal ball,” says Dr. Singer. “I see a soon-to-be emerging trend of hospitals wanting hospitalists rather than internists. More groups are going to step up and add that—make an internist into a subspecialist. It’s a new way of thinking.”
Even without a crystal ball, leaders in hospital medicine forecast that the field will continue to grow and that hospitalists will become better trained, credentialed, and accepted as a specialty—regardless of what type of organization they work for. TH
Jane Jerrard writes “Career Development” and “Public Policy” for The Hospitalist.
Disclaimer: SHM Members William Atchley, MD, FACP, Ron Greeno, MD, Stacy Goldsholl, MD, and Mark V. Williams, MD, FACP, are quoted in this article. Their opinions do not reflect or represent the opinions of SHM.
Hospital medicine may be a young field, but several major providers have already been established. Each of these rapidly growing organizations employs dozens—or even hundreds—of hospitalists and is establishing or revamping hospital medicine programs across the United States.
As these organizations grow, they are shaping hospital medicine. “I think that what the large companies really bring to the table is a vision of what hospital medicine is supposed to be about: evidence-based medicine and other things important to the hospital,” says William Atchley, MD, FACP, a practicing hospitalist in Hampton, Va.
This month, we examine just a few of the many large hospital medicine groups in order to set the stage for this growing trend and the issues presented by these groups. That said, here is an overview of some of the largest national players in hospital medicine, their perspective on the industry, their philosophies, and dialogue about their astonishing growth.
The Players
Which organizations have become the nation’s largest employers of hospitalists?
Cogent Healthcare
Based in Irvine, Calif., Cogent employs approximately 130 full-time hospitalists, with an additional 70 who “work with us in other arrangements; some are partnered with us,” says Ron Greeno, MD, FCCP, Cogent chief medical officer.
Cogent was founded by four physician groups in Los Angeles County. “We started in late 1997 and spent the first several years developing the model,” recalls Dr. Greeno. “In the 2000s, we started building programs for hospitals. We’ve seen growth of around 40% a year for the last several years. Frankly, we started too early; the market wasn’t really ready.”
What sets Cogent apart, says Dr. Greeno, is its focus. “We’re not a physician practice management company,” he stresses. “Our competitors’ goal is to build large, successful practices. We built a practice that’s hospital-centric. This helps the hospital satisfy its goals.”
EmCare
Perhaps the first of the national players to actively undertake hospital medicine, EmCare developed its first hospitalist program in 1993 at Baylor University Medical Center (BUMC) in Texas. “[Baylor is] still with us,” says Michael Wagner, MD, CEO, Hospitalists Division, EmCare.
EmCare has more than 30 years of experience with emergency department (ED) staffing, which is how it got its foot in the hospitalist door.
“In the late ’90s, other hospital EDs talked to us” about bringing in a hospitalist program, says Dr. Wagner. “So in each ED region, we worked to sell [the] hospital medicine program. It didn’t really take off until the 2000s, when non-clients started approaching us.”
Today, EmCare employs 350 hospitalists, 240 of whom work full-time. They provide hospital medicine to 47 clients in 60 programs in 37 states.
Emory Healthcare
Emory Healthcare’s Hospital Medicine Unit in Atlanta is the largest academic hospital medicine program in the United States.
“We occupy five hospitals,” says Mark V. Williams, MD, FACP, director of Emory’s Hospital Medicine Unit and editor of the Journal of Hospital Medicine. “Thirty of our hospitalists teach at the two university hospitals, and an additional eight teach at [one of three] community hospital[s]. Others will teach in-service training as well.”
The two university hospitals—Emory University Hospital and Crawford Long Hospital—are “solely staffed by Emory physicians,” explains Dr. Williams. “A third of what we do in these settings is teaching, and the rest is direct care.”
The university’s hospitalist program started in 1999 with eight hospitalists; today, it employs 60. The difference with an academic hospitalist program, explains Dr. Williams, is that “we’re essentially dealing with staffing teaching teams, teaching, and having research components.”
IPC–The Hospitalist Company
Perhaps the best-known hospitalist employer, IPC (North Hollywood, Calif.) currently has approximately 500 full-time employed hospitalists and 150-200 part-timers working in more than 200 facilities across 23 U.S. markets.
“We have every type of practice, including academic and small hospitals,” says Adam D. Singer, MD, chairman, CEO, and chief medical officer of IPC. The company was re-incorporated in 1995. “We started accelerating in ’97, and we’ve been growing 30 to 50% per year—steady growth. We’re acquiring like-minded groups. We’ve had 10 acquisitions in the last 24 months. All our acquisitions have to be high-minded, quality groups.”
PrimeDoc
Based in Asheville, N.C., PrimeDoc is 100% physician-owned and managed. Counting permanent employees as well as independent contractors, the company staffs approximately 110 hospitalists.
“We do things a little differently,” says Robert J. Reynolds, MD, president and CEO, who also co-founded PrimeDoc in 1997. “We started as a freestanding practice serving one hospital, and we use a private practice model today. We’ve grown by establishing private practices in five states along the Atlantic seaboard.”
Dr. Reynolds admits that the PrimeDoc model is not “terribly unique. We contract with hospitals to provide care to unassigned patients, and we solicit referrals from [primary care physicians] in the community.”
TeamHealth Hospital Medicine
Another company that started out providing ED services—as well as administrative and staffing services—TeamHealth (Wilmington, N.C.) now employees more than 400 hospitalists, most of whom are full-time employees.
“Until this past year, I think we’ve been a little bit of a sleeper in hospital medicine,” says Stacy Goldsholl, MD, president. “That’s all changing now, as we’re aggressively pursuing the number-one place in the market. But we’ve grown as a silent presence through our relational reputations—basically, through word of mouth in the emergency departments. We have more than 400 contracts [in emergency medicine].”
The company continues to add hospital medicine programs through several methods. “We set up new programs from scratch, we restructure existing programs, we acquire large hospital medicine groups,” says Dr. Goldsholl, “and we apply things that work in one model to other models.”
Growth Trends
One feature these organizations have in common: explosive growth. The corporations are acquiring, starting, or partnering with a steady stream of hospital medicine programs.
“We’ve more than doubled in the last year,” says Dr. Goldsholl. “Our pipeline for hospital medicine groups is just exploding. We’re trying to manage the growth we have as well as what’s coming. We hope to double again in the next two years.”
Within that increase in programs comes another growth trend: hospital clients are asking their hospital medicine groups to take on more responsibility. “Our role in the hospital setting is definitely expanding,” says Dr. Goldsholl. “And the hospitalist’s role is only going to increase. We’ll see more hospital-based intensivists, surgicalists, and laborists [OB/GYN physicians]—there’s tremendous growth coming.”
Dr. Reynolds agrees. “In 1997, we basically provided medical care for acute care patients,” he explains. “Now we’re providing care for surgical care patients. We do pre-op eval[uation]s and perioperative management. We’ve also seen more demand for rapid response management, and we’re being asked to do pre-op eval[uation]s for outpatient surgeries.”
More hospitals are proactively seeking out these market leaders to explore adding a new hospital medicine program. “We’re getting calls from smaller and smaller hospitals,” says Dr. Reynolds. “Even the smallest hospitals want to implement a hospital medicine program, and it’s difficult to provide 24-hour coverage and have it make sense financially. But the trend is promising: Every hospital wants this type of service.”
Will these big players gobble up independent programs? That depends on how those programs are doing. “I haven’t heard of any programs being replaced if they’re doing all the right things and their costs are in line,” according to Dr. Atchley. “What you’re seeing is national companies either starting programs or salvaging programs that have failed.”
Industry Trends
Managing a large number of hospital medicine programs provides these companies with a clearer view of what’s happening in the specialty as it grows and changes. One trend that they’re seeing is a sort of second phase, where hospitals that brought in hospitalists several years ago now seek to improve their programs.
“In the past year, we’ve seen [hospitals express] more need, more interest in a hospital medicine management company coming in and restructuring a struggling program or a failed program,” says Dr. Goldsholl.
EmCare observes the same trend. “Hospitals are a lot savvier than they were five or 10 years ago about the setup of a hospital medicine program,” says Dr. Wagner. “Some [hospital administrators] may be on their second or third program, and they know what they want. They ask about recruitment success, retention rates, your data gathering and reporting tools, and what you do specifically to support your physicians in terms of leadership, quality, and satisfaction.”
These expectations are not simply discussed; they become part of the contractual agreement. “Hospitals also want service deliverables written in the contract,” adds Dr. Wagner, “including physician performance in terms of patient satisfaction, primary care physician satisfaction, JCAHO core measures, and medical staff participation.”
Why Big May Be Better
A large group with an established infrastructure that includes standards for quality checks, patient satisfaction, and so on is appealing to hospitals. “Because of economies of scale, we can offer state-of-the-art technologies, billing and collection, and infrastructure,” says Dr. Singer. “We also have the ability to recruit physicians. Small groups cannot compete with that.”
Another attractive feature is the history that these groups have in a relatively new field. “We have a track record of setting up successful programs,” points out Dr. Reynolds. ”We’ve already learned from our mistakes.”
Working for a national corporation has its benefits, including opportunities for education and advancement and an infrastructure support that can take some of the workload off a hospitalist’s shoulders. Dr. Greeno points out that Cogent handles administrative work for the physicians, freeing up their time for patients.
“One guy said, ‘I like working here because it’s the best opportunity to practice pure medicine,’ ” he says. “Our physicians are not case managers; they’re not schedulers.”
And working as part of a large group provides a built-in network of colleagues. “There’s connectivity for the individual hospitalist, as well as the medical director, to learn from other hospitalists all over the country,” says Dr. Goldsholl.
Dr. Wagner names compliance as one of EmCare’s top benefits. “We code physician notes professionally, and the result is we have greater than 95% compliance with Medicare. That’s something a national company can bring to the table.”
Some say that a large organization may be more attractive to job candidates. “Our size demonstrates stability to candidates,” says Dr. Williams. “Recruiting is a 100%-a-year job, and this helps.”
He points out that a larger program can appeal to the hospitalists within it: “Another advantage to our size is that we can draw from a pool of physicians to help out if necessary.”
Of course, physicians who work for larger companies may enjoy a larger compensation package, which can benefit the entire specialty. “In my experience, when [large companies] have come into my area, their salary structure is higher,” says Dr. Atchley. “The result is that other groups in the region have to change their salaries to be more competitive.”
The Upside to Independents
One factor that helps hospitals decide between bringing in a national company and using an independent local group is the cost.
“[Local programs] may not be as expensive as the large groups,” says Dr. Atchley. “When my hospital sent out an RFP [request for proposal], we saw that some of our costs were much less than what a national company” has to charge.
One major concern individual hospitalists and smaller groups may have regarding employment in a national corporation is loss of autonomy. Would they be expected to follow rigid rules and regulations set forth by a distant corporation office? The leaders in those offices say no, absolutely not.
“We actually manage down to a small practice,” says Dr. Singer. “Concerns are that there will be a loss of autonomy; that’s not true.”
Regardless of which type of hospital medicine program one prefers, having options is good for both the hospital and the physician. “Competition is good,” maintains Dr. Atchley. “When these companies come in, they’ll definitely provide superior infrastructure and can track outcomes. Homegrown hospital medicine programs should use the same approach.”
A Glimpse of the Future
Will all hospitalists eventually work for a behemoth corporation? Not a chance, say the CEOs and CMOs of the current hospital medicine company leaders. “There are lessons to be learned from the emergency department,” says Dr. Wagner. “Large companies don’t have the majority of ED contracts. There’s only so much [large companies] can manage before it starts to get picked off by smaller, younger practices that are more nimble and quick to respond.
“All the big players won’t be dominant from a market-share point of view,” he adds. “But what they will do is set expectations for good hospital medicine practices.”
However, the employment model for hospitalists will continue to change. “We’re going to see existing [large] companies increase their regional presence,” predicts Dr. Reynolds. “The hospital-owned model will fade away. Physicians make lousy hospital employees—they just don’t fit into the hospital’s view of an employee.”
Dr. Atchley agrees with this point: “We’ll probably see fewer and fewer programs where the physician is employed by the hospital. That’s pretty much what the SHM surveys are showing.”
And when will the booming market for hospitalists start to slow? “I see [the market] growing well beyond my crystal ball,” says Dr. Singer. “I see a soon-to-be emerging trend of hospitals wanting hospitalists rather than internists. More groups are going to step up and add that—make an internist into a subspecialist. It’s a new way of thinking.”
Even without a crystal ball, leaders in hospital medicine forecast that the field will continue to grow and that hospitalists will become better trained, credentialed, and accepted as a specialty—regardless of what type of organization they work for. TH
Jane Jerrard writes “Career Development” and “Public Policy” for The Hospitalist.