User login
A 69-year-old woman with a history of hypertension, hyperlipidemia, diabetes, osteoarthritis, and depression presented to the emergency department (ED) with a 2-day history of blisters on the dorsal aspect of her toes on both feet. She had been wearing sandals so as not to disrupt them. The bullae appeared over the course of one day and progressively grew. The patient had no fever, chills, pain, or itching. She said she’d never had blisters like these before, and she had no history of cellulitis; she also denied trauma to her feet. There were no recent changes to any prescription or nonprescription medications. She also had not had any prolonged exposure to the sun or anything new that would suggest contact dermatitis.
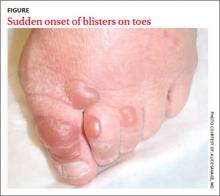
The physical exam revealed an otherwise healthy woman with multiple, clear, fluid-filled bullae of varying sizes on her toes (FIGURE). There was no erythema, warmth, or tenderness. She could walk without difficulty. Her vital signs were normal. A white blood cell count and differential were normal, as well.
Our patient was admitted because of a mistaken concern for cellulitis, despite the absence of any systemic findings or surrounding erythema. She was discharged the next day with no change in status and without treatment. She returned to the ED several days later with the bullae still intact; a biopsy was performed and sent for immunofluorescence.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Bullosis diabeticorum
Direct immunofluorescence was negative. This, along with the patient’s history of diabetes, led us to diagnose bullosis diabeticorum in this patient. This condition, also known as bullous disease of diabetes, is characterized by abrupt development of noninflammatory bullae on acral areas in patients with diabetes. The skin appears normal except for the bullae.1 Bullosis diabeticorum occurs in just .5% of patients with diabetes.2 It is twice as common in men as in women.2
The etiology of bullosis diabeticorum is unknown. The acral location suggests that trauma may be a contributing factor. Although electron microscopy has suggested an abnormality in anchoring fibrils, this cellular change does not fully explain the development of multiple blisters at varying sites. Glycemic control is not thought to play a role.2
A large differential
The distribution of lesions and the presence—or absence—of systemic symptoms go a long way toward narrowing the differential of blistering diseases. The presence of generalized blistering and systemic symptoms would suggest conditions related to medication exposure, such as Stevens-Johnson syndrome or toxic epidermal necrolysis; infectious etiologies (eg, staphylococcal scalded skin syndrome); autoimmune causes; or underlying malignancy.3 Generalized blistering in the absence of systemic symptoms would support diagnoses such as bullous impetigo and pemphigoid.3
Lesion distribution provides important clues, too. Sun exposure-related causes typically leave lesions on the hands and forearms, not just the toes. A dermatomal distribution would suggest herpes zoster. A linear distribution of blisters argues for contact dermatitis. Mucous membrane involvement would suggest etiologies such as herpes simplex virus, erythema multiforme, pemphigus vulgaris, Stevens-Johnson syndrome, or toxic epidermal necrolysis.
Some conditions cannot be excluded from the differential diagnosis upon presentation. Hereditary epidermolysis bullosa (EB) represents a set of inherited diseases in which trauma causes blisters. Localized EB simplex, Weber-Cockayne subtype, can present in adulthood. Blisters can result from trauma on the hands or feet after excessive exercise.4 Although our patient did not give a history of excessive exercise, and this condition is rare, it and similar conditions must be ruled out.
Making the diagnosis
A diagnosis of bullosis diabeticorum can be made when biopsy with immunofluorescence excludes other histologically similar entities such as EB, noninflammatory bullous pemphigoid, and porphyria cutanea tarda. And while immunofluorescence findings are typically negative, elevated levels of immunoglobulin M and C3 have, on occasion, been reported.5,6 Cultures are warranted only if a secondary infection is suspected.
Treatment is usually unnecessary
The bullae of this condition spontaneously resolve over several weeks without treatment, but tend to recur. The lesions typically heal without significant scarring, although they may have a darker pigmentation after the first occurrence.4 Treatment may be warranted if a patient develops a secondary infection.
In our patient’s case…The bullae resolved within 2 weeks without treatment, although mild hyperpigmentation remained.
CORRESPONDENCE
Lisa Mims, MD, Department of Family Medicine, Medical University of South Carolina, 5 Charleston Center Drive, Suite 263, MSC 192, Charleston, SC 29425; durham@musc.edu
1. Kramer DW. Early or warning signs of impending gangrene in diabetes. Med J Rec. 1930;132:338-342.
2. Poh-Fitzpatrick MB, Junkins-Hopkins JM. Bullous disease of diabetes. Available at: http://emedicine.medscape.com/article/1062235-overview. Accessed March 31, 2014.
3. Hull C, Zone JJ. Approach to the patient with cutaneous blisters. Available at: http://www.uptodate.com/contents/approach-to-the-patient-with-cutaneous-blisters. Accessed March 11, 2014.
4. Rocca FF, Pereyra E. Phlyctenar lesions in the feet of diabetic patients. Diabetes. 1963;12:220-222.
5. James WD, Odom RB, Goette DK. Bullous eruption of diabetes. A case with positive immunofluorescence microscopy findings. Arch Dermatol. 1980;116:1191-1192.
6. Basarab T, Munn SE, McGrath J, et al. Bullous diabeticorum. A case report and literature review. Clin Exp Dermatol. 1995;20:218-220.
A 69-year-old woman with a history of hypertension, hyperlipidemia, diabetes, osteoarthritis, and depression presented to the emergency department (ED) with a 2-day history of blisters on the dorsal aspect of her toes on both feet. She had been wearing sandals so as not to disrupt them. The bullae appeared over the course of one day and progressively grew. The patient had no fever, chills, pain, or itching. She said she’d never had blisters like these before, and she had no history of cellulitis; she also denied trauma to her feet. There were no recent changes to any prescription or nonprescription medications. She also had not had any prolonged exposure to the sun or anything new that would suggest contact dermatitis.
The physical exam revealed an otherwise healthy woman with multiple, clear, fluid-filled bullae of varying sizes on her toes (FIGURE). There was no erythema, warmth, or tenderness. She could walk without difficulty. Her vital signs were normal. A white blood cell count and differential were normal, as well.
Our patient was admitted because of a mistaken concern for cellulitis, despite the absence of any systemic findings or surrounding erythema. She was discharged the next day with no change in status and without treatment. She returned to the ED several days later with the bullae still intact; a biopsy was performed and sent for immunofluorescence.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Bullosis diabeticorum
Direct immunofluorescence was negative. This, along with the patient’s history of diabetes, led us to diagnose bullosis diabeticorum in this patient. This condition, also known as bullous disease of diabetes, is characterized by abrupt development of noninflammatory bullae on acral areas in patients with diabetes. The skin appears normal except for the bullae.1 Bullosis diabeticorum occurs in just .5% of patients with diabetes.2 It is twice as common in men as in women.2
The etiology of bullosis diabeticorum is unknown. The acral location suggests that trauma may be a contributing factor. Although electron microscopy has suggested an abnormality in anchoring fibrils, this cellular change does not fully explain the development of multiple blisters at varying sites. Glycemic control is not thought to play a role.2
A large differential
The distribution of lesions and the presence—or absence—of systemic symptoms go a long way toward narrowing the differential of blistering diseases. The presence of generalized blistering and systemic symptoms would suggest conditions related to medication exposure, such as Stevens-Johnson syndrome or toxic epidermal necrolysis; infectious etiologies (eg, staphylococcal scalded skin syndrome); autoimmune causes; or underlying malignancy.3 Generalized blistering in the absence of systemic symptoms would support diagnoses such as bullous impetigo and pemphigoid.3
Lesion distribution provides important clues, too. Sun exposure-related causes typically leave lesions on the hands and forearms, not just the toes. A dermatomal distribution would suggest herpes zoster. A linear distribution of blisters argues for contact dermatitis. Mucous membrane involvement would suggest etiologies such as herpes simplex virus, erythema multiforme, pemphigus vulgaris, Stevens-Johnson syndrome, or toxic epidermal necrolysis.
Some conditions cannot be excluded from the differential diagnosis upon presentation. Hereditary epidermolysis bullosa (EB) represents a set of inherited diseases in which trauma causes blisters. Localized EB simplex, Weber-Cockayne subtype, can present in adulthood. Blisters can result from trauma on the hands or feet after excessive exercise.4 Although our patient did not give a history of excessive exercise, and this condition is rare, it and similar conditions must be ruled out.
Making the diagnosis
A diagnosis of bullosis diabeticorum can be made when biopsy with immunofluorescence excludes other histologically similar entities such as EB, noninflammatory bullous pemphigoid, and porphyria cutanea tarda. And while immunofluorescence findings are typically negative, elevated levels of immunoglobulin M and C3 have, on occasion, been reported.5,6 Cultures are warranted only if a secondary infection is suspected.
Treatment is usually unnecessary
The bullae of this condition spontaneously resolve over several weeks without treatment, but tend to recur. The lesions typically heal without significant scarring, although they may have a darker pigmentation after the first occurrence.4 Treatment may be warranted if a patient develops a secondary infection.
In our patient’s case…The bullae resolved within 2 weeks without treatment, although mild hyperpigmentation remained.
CORRESPONDENCE
Lisa Mims, MD, Department of Family Medicine, Medical University of South Carolina, 5 Charleston Center Drive, Suite 263, MSC 192, Charleston, SC 29425; durham@musc.edu
A 69-year-old woman with a history of hypertension, hyperlipidemia, diabetes, osteoarthritis, and depression presented to the emergency department (ED) with a 2-day history of blisters on the dorsal aspect of her toes on both feet. She had been wearing sandals so as not to disrupt them. The bullae appeared over the course of one day and progressively grew. The patient had no fever, chills, pain, or itching. She said she’d never had blisters like these before, and she had no history of cellulitis; she also denied trauma to her feet. There were no recent changes to any prescription or nonprescription medications. She also had not had any prolonged exposure to the sun or anything new that would suggest contact dermatitis.
The physical exam revealed an otherwise healthy woman with multiple, clear, fluid-filled bullae of varying sizes on her toes (FIGURE). There was no erythema, warmth, or tenderness. She could walk without difficulty. Her vital signs were normal. A white blood cell count and differential were normal, as well.
Our patient was admitted because of a mistaken concern for cellulitis, despite the absence of any systemic findings or surrounding erythema. She was discharged the next day with no change in status and without treatment. She returned to the ED several days later with the bullae still intact; a biopsy was performed and sent for immunofluorescence.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Bullosis diabeticorum
Direct immunofluorescence was negative. This, along with the patient’s history of diabetes, led us to diagnose bullosis diabeticorum in this patient. This condition, also known as bullous disease of diabetes, is characterized by abrupt development of noninflammatory bullae on acral areas in patients with diabetes. The skin appears normal except for the bullae.1 Bullosis diabeticorum occurs in just .5% of patients with diabetes.2 It is twice as common in men as in women.2
The etiology of bullosis diabeticorum is unknown. The acral location suggests that trauma may be a contributing factor. Although electron microscopy has suggested an abnormality in anchoring fibrils, this cellular change does not fully explain the development of multiple blisters at varying sites. Glycemic control is not thought to play a role.2
A large differential
The distribution of lesions and the presence—or absence—of systemic symptoms go a long way toward narrowing the differential of blistering diseases. The presence of generalized blistering and systemic symptoms would suggest conditions related to medication exposure, such as Stevens-Johnson syndrome or toxic epidermal necrolysis; infectious etiologies (eg, staphylococcal scalded skin syndrome); autoimmune causes; or underlying malignancy.3 Generalized blistering in the absence of systemic symptoms would support diagnoses such as bullous impetigo and pemphigoid.3
Lesion distribution provides important clues, too. Sun exposure-related causes typically leave lesions on the hands and forearms, not just the toes. A dermatomal distribution would suggest herpes zoster. A linear distribution of blisters argues for contact dermatitis. Mucous membrane involvement would suggest etiologies such as herpes simplex virus, erythema multiforme, pemphigus vulgaris, Stevens-Johnson syndrome, or toxic epidermal necrolysis.
Some conditions cannot be excluded from the differential diagnosis upon presentation. Hereditary epidermolysis bullosa (EB) represents a set of inherited diseases in which trauma causes blisters. Localized EB simplex, Weber-Cockayne subtype, can present in adulthood. Blisters can result from trauma on the hands or feet after excessive exercise.4 Although our patient did not give a history of excessive exercise, and this condition is rare, it and similar conditions must be ruled out.
Making the diagnosis
A diagnosis of bullosis diabeticorum can be made when biopsy with immunofluorescence excludes other histologically similar entities such as EB, noninflammatory bullous pemphigoid, and porphyria cutanea tarda. And while immunofluorescence findings are typically negative, elevated levels of immunoglobulin M and C3 have, on occasion, been reported.5,6 Cultures are warranted only if a secondary infection is suspected.
Treatment is usually unnecessary
The bullae of this condition spontaneously resolve over several weeks without treatment, but tend to recur. The lesions typically heal without significant scarring, although they may have a darker pigmentation after the first occurrence.4 Treatment may be warranted if a patient develops a secondary infection.
In our patient’s case…The bullae resolved within 2 weeks without treatment, although mild hyperpigmentation remained.
CORRESPONDENCE
Lisa Mims, MD, Department of Family Medicine, Medical University of South Carolina, 5 Charleston Center Drive, Suite 263, MSC 192, Charleston, SC 29425; durham@musc.edu
1. Kramer DW. Early or warning signs of impending gangrene in diabetes. Med J Rec. 1930;132:338-342.
2. Poh-Fitzpatrick MB, Junkins-Hopkins JM. Bullous disease of diabetes. Available at: http://emedicine.medscape.com/article/1062235-overview. Accessed March 31, 2014.
3. Hull C, Zone JJ. Approach to the patient with cutaneous blisters. Available at: http://www.uptodate.com/contents/approach-to-the-patient-with-cutaneous-blisters. Accessed March 11, 2014.
4. Rocca FF, Pereyra E. Phlyctenar lesions in the feet of diabetic patients. Diabetes. 1963;12:220-222.
5. James WD, Odom RB, Goette DK. Bullous eruption of diabetes. A case with positive immunofluorescence microscopy findings. Arch Dermatol. 1980;116:1191-1192.
6. Basarab T, Munn SE, McGrath J, et al. Bullous diabeticorum. A case report and literature review. Clin Exp Dermatol. 1995;20:218-220.
1. Kramer DW. Early or warning signs of impending gangrene in diabetes. Med J Rec. 1930;132:338-342.
2. Poh-Fitzpatrick MB, Junkins-Hopkins JM. Bullous disease of diabetes. Available at: http://emedicine.medscape.com/article/1062235-overview. Accessed March 31, 2014.
3. Hull C, Zone JJ. Approach to the patient with cutaneous blisters. Available at: http://www.uptodate.com/contents/approach-to-the-patient-with-cutaneous-blisters. Accessed March 11, 2014.
4. Rocca FF, Pereyra E. Phlyctenar lesions in the feet of diabetic patients. Diabetes. 1963;12:220-222.
5. James WD, Odom RB, Goette DK. Bullous eruption of diabetes. A case with positive immunofluorescence microscopy findings. Arch Dermatol. 1980;116:1191-1192.
6. Basarab T, Munn SE, McGrath J, et al. Bullous diabeticorum. A case report and literature review. Clin Exp Dermatol. 1995;20:218-220.