User login
The Diagnosis: Talon Noir
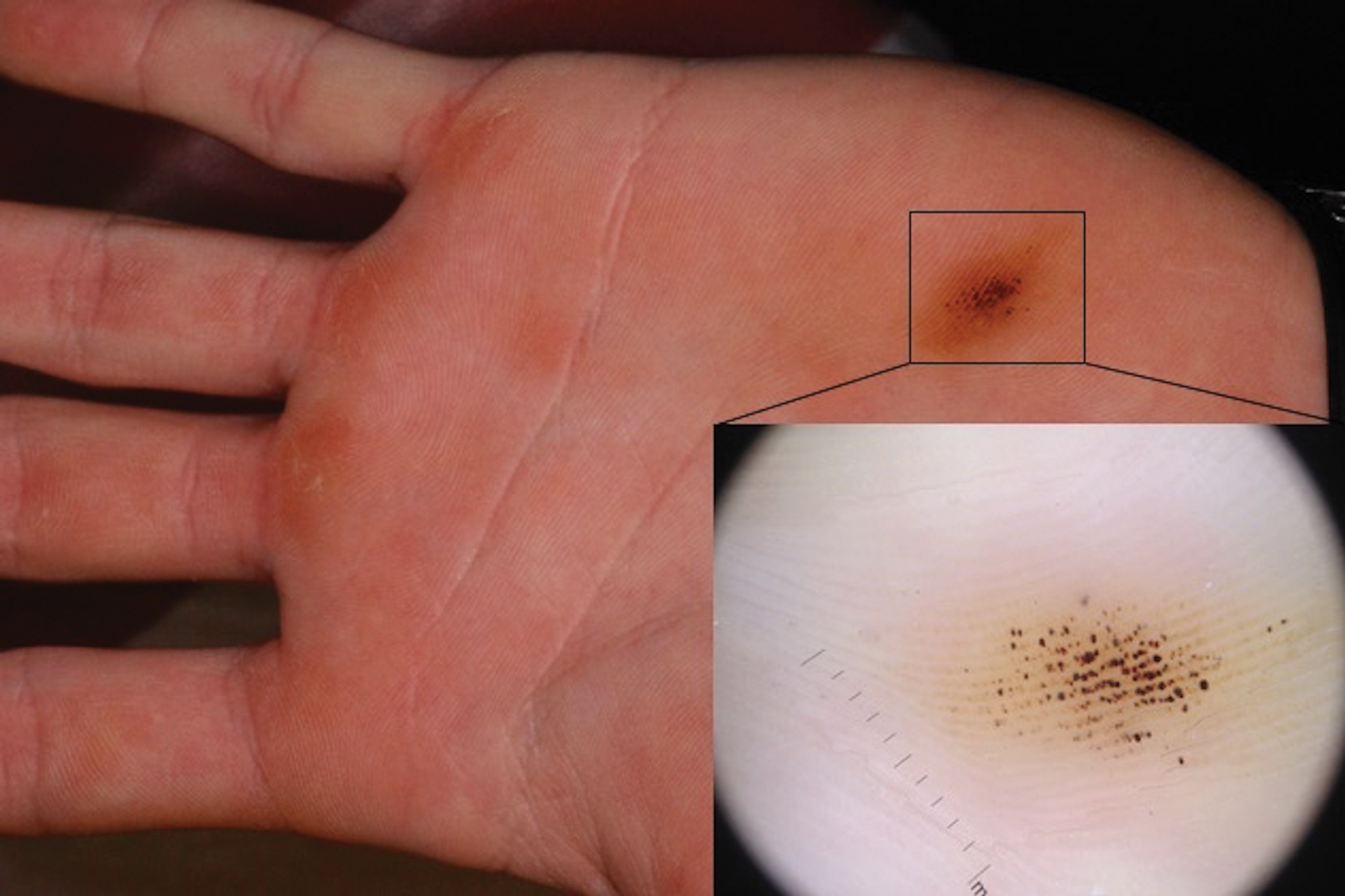
Paring of the stratum corneum overlying the lesion revealed coagulated blood, leading to a diagnosis of talon noir. Talon noir, also known as calcaneal petechiae, is a benign lesion that is typically found on the heel of the foot or palm of the hand.1 To the naked eye, talon noir appears as a brown-black asymmetric macule often with an overlying callus. Dermatoscopic visualization reveals grouped, reddish-colored globules composed of intracorneal hemorrhages, often in a linear pattern without any disruption of the normal skin surface architecture.1,2
Talon noir is the product of shear stress and often is seen in individuals who participate in sports such as baseball, hockey, soccer, and football.1,3 Lateral shearing forces cause tearing of blood vessels within the papillary dermis, which leads to punctate papillary dermal hemorrhages and extravasation of blood into the epidermis, resulting in intracorneal hemorrhage.1,4 Talon noir lesions are completely asymptomatic and typically resolve without intervention within 2 to 3 weeks of discontinuation of the precipitating sport or trauma.4
Recognizing talon noir is important, as it can occasionally be mistaken for acral lentiginous melanoma junctional nevus, tinea nigra, or verruca vulgaris. Paring of a lesion that is suspicious for talon noir is a simple and important step for ruling out a more ominous diagnosis (ie, acral lentiginous melanoma). If paring reveals coagulated blood, then junctional nevus, acral lentiginous melanoma, and tinea nigra can be excluded from the differential diagnosis. To rule out verruca vulgaris, one must prove that there is no disruption of the normal skin architecture, which can be confirmed with dermatoscopic visualization. Verrucae characteristically cause disruption of normal skin architecture, and junctional nevi would reveal a pigment pattern on dermatoscopy. This case illustrates how simple bedside procedures—dermoscopy and paring—can reassure patients and caregivers of the benign nature of talon noir.
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731.
2. Lao M, Weissler A, Siegfried E. Talon noir. J Pediatr. 2013;163:919.
3. Ayres S, Mihan R. Calcaneal petechiae. Arch Dermatol. 1972;106:262.
4. Bender TW. Cutaneous manifestations of disease in athletes. Skinmed. 2003;2:34-40
The Diagnosis: Talon Noir
Paring of the stratum corneum overlying the lesion revealed coagulated blood, leading to a diagnosis of talon noir. Talon noir, also known as calcaneal petechiae, is a benign lesion that is typically found on the heel of the foot or palm of the hand.1 To the naked eye, talon noir appears as a brown-black asymmetric macule often with an overlying callus. Dermatoscopic visualization reveals grouped, reddish-colored globules composed of intracorneal hemorrhages, often in a linear pattern without any disruption of the normal skin surface architecture.1,2
Talon noir is the product of shear stress and often is seen in individuals who participate in sports such as baseball, hockey, soccer, and football.1,3 Lateral shearing forces cause tearing of blood vessels within the papillary dermis, which leads to punctate papillary dermal hemorrhages and extravasation of blood into the epidermis, resulting in intracorneal hemorrhage.1,4 Talon noir lesions are completely asymptomatic and typically resolve without intervention within 2 to 3 weeks of discontinuation of the precipitating sport or trauma.4
Recognizing talon noir is important, as it can occasionally be mistaken for acral lentiginous melanoma junctional nevus, tinea nigra, or verruca vulgaris. Paring of a lesion that is suspicious for talon noir is a simple and important step for ruling out a more ominous diagnosis (ie, acral lentiginous melanoma). If paring reveals coagulated blood, then junctional nevus, acral lentiginous melanoma, and tinea nigra can be excluded from the differential diagnosis. To rule out verruca vulgaris, one must prove that there is no disruption of the normal skin architecture, which can be confirmed with dermatoscopic visualization. Verrucae characteristically cause disruption of normal skin architecture, and junctional nevi would reveal a pigment pattern on dermatoscopy. This case illustrates how simple bedside procedures—dermoscopy and paring—can reassure patients and caregivers of the benign nature of talon noir.
The Diagnosis: Talon Noir
Paring of the stratum corneum overlying the lesion revealed coagulated blood, leading to a diagnosis of talon noir. Talon noir, also known as calcaneal petechiae, is a benign lesion that is typically found on the heel of the foot or palm of the hand.1 To the naked eye, talon noir appears as a brown-black asymmetric macule often with an overlying callus. Dermatoscopic visualization reveals grouped, reddish-colored globules composed of intracorneal hemorrhages, often in a linear pattern without any disruption of the normal skin surface architecture.1,2
Talon noir is the product of shear stress and often is seen in individuals who participate in sports such as baseball, hockey, soccer, and football.1,3 Lateral shearing forces cause tearing of blood vessels within the papillary dermis, which leads to punctate papillary dermal hemorrhages and extravasation of blood into the epidermis, resulting in intracorneal hemorrhage.1,4 Talon noir lesions are completely asymptomatic and typically resolve without intervention within 2 to 3 weeks of discontinuation of the precipitating sport or trauma.4
Recognizing talon noir is important, as it can occasionally be mistaken for acral lentiginous melanoma junctional nevus, tinea nigra, or verruca vulgaris. Paring of a lesion that is suspicious for talon noir is a simple and important step for ruling out a more ominous diagnosis (ie, acral lentiginous melanoma). If paring reveals coagulated blood, then junctional nevus, acral lentiginous melanoma, and tinea nigra can be excluded from the differential diagnosis. To rule out verruca vulgaris, one must prove that there is no disruption of the normal skin architecture, which can be confirmed with dermatoscopic visualization. Verrucae characteristically cause disruption of normal skin architecture, and junctional nevi would reveal a pigment pattern on dermatoscopy. This case illustrates how simple bedside procedures—dermoscopy and paring—can reassure patients and caregivers of the benign nature of talon noir.
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731.
2. Lao M, Weissler A, Siegfried E. Talon noir. J Pediatr. 2013;163:919.
3. Ayres S, Mihan R. Calcaneal petechiae. Arch Dermatol. 1972;106:262.
4. Bender TW. Cutaneous manifestations of disease in athletes. Skinmed. 2003;2:34-40
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731.
2. Lao M, Weissler A, Siegfried E. Talon noir. J Pediatr. 2013;163:919.
3. Ayres S, Mihan R. Calcaneal petechiae. Arch Dermatol. 1972;106:262.
4. Bender TW. Cutaneous manifestations of disease in athletes. Skinmed. 2003;2:34-40
A 16-year-old adolescent boy presented to our clinic with a “new brown mole” on the left palm that had appeared within the last few months. The patient did not recall if it had changed in size, shape, or color, and there was no associated pain or itching. He denied any trauma to the hand, but he actively played both hockey and baseball. Physical examination revealed calloused palms bilaterally. One of the calluses was present over the hypothenar eminence, and centrally there were grouped brown-black punctate macules, some that coalesced into larger macules. Dermatoscopic examination (inset) revealed punctate rustcolored macules in a parallel ridge pattern. There was no disruption of the normal skin architecture.