User login
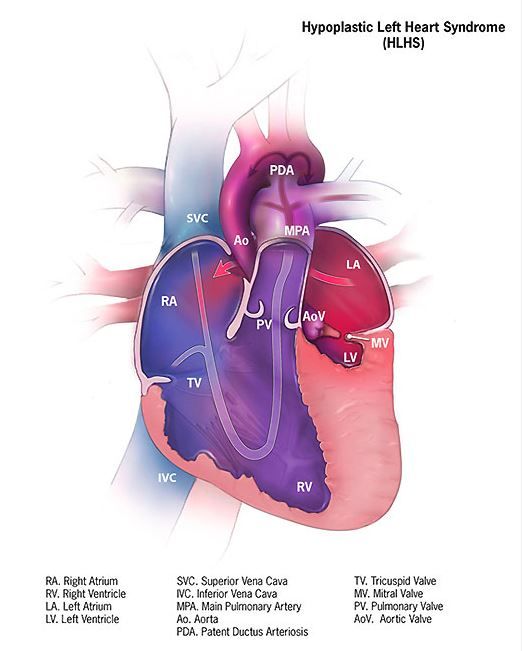
The regional oxygenation index (rSO2) based on near infrared spectroscopy (NIRS) measurement is frequently used to assess the adequacy of oxygen delivery after stage 1 palliation of hypoplastic left heart syndrome (HLHS). However, a recent study showed that cerebral rSO2 has low sensitivity and should not be considered reassuring even at rSO2 of 50 or greater. In addition, values below 30 were not found to be sensitive for detecting compromised oxygen delivery, according to a report published online in the Journal of Thoracic and Cardiovascular Surgery.
Erin Rescoe, MD, of Boston Children’s Hospital, and her colleagues at Harvard Medical School, Boston, performed a retrospective study of 73 neonates assessed with cerebral venous oxyhemoglobin saturation (ScvO2) measured by co-oximetry from the internal jugular vein, which is considered the preferred method for assessing the adequacy of tissue oxygen delivery, compared with cerebral rSO2 after stage 1 palliation of HLHS (doi: 10.1016/j.jtcvs.2017.03.154).
To determine the suggested benefit of NIRS as an effective trend monitor, the researchers used their interpolated data to examine changes in rSO2 and changes in ScvO2 at hourly intervals and compared these values.Of particular concern is the result showing that, in all instances where ScvO2 was less than 30%, rSO2 was greater than 30%. In terms of the sensitivity (the true positive rate) and specificity (the true negative rate) of using NIRS, time-matched pairs of rSO2 and ScvO2 showed that the receiver operating characteristic curves for rSO2 as a diagnostic test to detect ScvO2 less than 30%, less than 40%, and less than 50% were 0.82, 0.84, and 0.87, respectively, showing good specificity, with a value of rSO2 less than 30% indicating that ScvO2 will be less than 30% 99% of the time.
“However, the sensitivity of rSO2 in the range of clinical interest in detecting ScvO2 less than 30% is extremely low,” according to the researchers. Thus, NIRS is likely to produce false negatives, missing patients with clinically low postoperative oxygen saturation.
In fact, rSO2 was less than 30% less than 1% of the time that ScvO2 was less than 30%. Similar results were seen in comparing values at the less than 40% mark (equivalent less than 1% of the time). Better results showed at the less than 50% mark, with equivalence seen 46% of the time.
NIRS measures a composite of arterial and venous blood, according to Dr. Rescoe and her colleagues. Therefore, to do a more direct comparison, they adjusted their NIRS results by calculating an rSO2-based ScvO2 designed to remove arterial contamination from the rSO2 signal: rSO2-based ScvO2 = (rSO2 arterial oxygen saturation x 0.3)/0.7.
This significantly improved the sensitivity of rSO2 to detect ScvO2 at less than 30% to 6.5%, to 29% for rSO2 at less than 40%, and 77.4% for rSO2 less than 50%.
The researchers “were surprised by the extremely low sensitivity of cerebral NIRS to detect even the most severe aberrations in DO2” (i.e., ScvO2 less than 30%, which has been found to be associated with poor outcomes).
“Cerebral rSO2 in isolation should not be used to detect low ScvO2, because its sensitivity is low, although correction of rSO2 for arterial contamination significantly improves sensitivity. Cerebral rSO2 of 50 or greater should not be considered reassuring with regard to ScvO2, although values less than 30 are specific for low ScvO2,” the researchers concluded.
The study was sponsored by the Gerber Foundation, the Hess Family Philanthropic Fund, and Boston Children’s Hospital Heart Center Strategic Investment Fund. The authors disclosed that they had no financial conflicts.
The use of postoperative cerebral venous oxygen saturation monitoring (ScvO2) through an internal jugular vein catheter allows better monitoring of circulation, which may lead to better outcomes, but it is invasive and challenging. NIRS, being noninvasive, has proved attractive, but clinical interpretation in terms of both absolute values and trends is difficult, Edward Buratto, MBBS, and his colleagues noted in their invited commentary (doi: 10.1016/j.jtcvs.2017.04.061).
Dr. Rescoe and her colleagues have analyzed the correlation of NIRS-derived data with ScvO2 measured by co-oximetry from the internal jugular vein in 73 neonates after stage 1 palliation for hypoplastic left heart syndrome. They demonstrated that cerebral rSO2 correlated poorly with low ScvO2, and they suggest that cerebral rSO2 not be used in isolation. This problem was somewhat ameliorated by correction of the signal for arterial contamination. NIRS appears to be too valuable a tool to be simply discarded, they said, suggesting that a perioperative risk assessment that would include multisite NIRS and hemodynamic monitoring might still allow early determination of low-cardiac output.
“Two numbers are better than one,” wrote Dr. Buratto and his colleagues. “Whether the NIRS technology will add any useful information to a simple bedside assessment by an astute clinician is yet to be seen.”
Edward Buratto, MBBS, Steve Horton, PhD, and Igor E. Konstantinov, MD, are from the Department of Cardiothoracic Surgery, The Royal Children’s Hospital; the Department of Pediatrics, University of Melbourne; and Murdoch Children’s Research Institute, Melbourne. They reported having no financial conflicts of interest.
The use of postoperative cerebral venous oxygen saturation monitoring (ScvO2) through an internal jugular vein catheter allows better monitoring of circulation, which may lead to better outcomes, but it is invasive and challenging. NIRS, being noninvasive, has proved attractive, but clinical interpretation in terms of both absolute values and trends is difficult, Edward Buratto, MBBS, and his colleagues noted in their invited commentary (doi: 10.1016/j.jtcvs.2017.04.061).
Dr. Rescoe and her colleagues have analyzed the correlation of NIRS-derived data with ScvO2 measured by co-oximetry from the internal jugular vein in 73 neonates after stage 1 palliation for hypoplastic left heart syndrome. They demonstrated that cerebral rSO2 correlated poorly with low ScvO2, and they suggest that cerebral rSO2 not be used in isolation. This problem was somewhat ameliorated by correction of the signal for arterial contamination. NIRS appears to be too valuable a tool to be simply discarded, they said, suggesting that a perioperative risk assessment that would include multisite NIRS and hemodynamic monitoring might still allow early determination of low-cardiac output.
“Two numbers are better than one,” wrote Dr. Buratto and his colleagues. “Whether the NIRS technology will add any useful information to a simple bedside assessment by an astute clinician is yet to be seen.”
Edward Buratto, MBBS, Steve Horton, PhD, and Igor E. Konstantinov, MD, are from the Department of Cardiothoracic Surgery, The Royal Children’s Hospital; the Department of Pediatrics, University of Melbourne; and Murdoch Children’s Research Institute, Melbourne. They reported having no financial conflicts of interest.
The use of postoperative cerebral venous oxygen saturation monitoring (ScvO2) through an internal jugular vein catheter allows better monitoring of circulation, which may lead to better outcomes, but it is invasive and challenging. NIRS, being noninvasive, has proved attractive, but clinical interpretation in terms of both absolute values and trends is difficult, Edward Buratto, MBBS, and his colleagues noted in their invited commentary (doi: 10.1016/j.jtcvs.2017.04.061).
Dr. Rescoe and her colleagues have analyzed the correlation of NIRS-derived data with ScvO2 measured by co-oximetry from the internal jugular vein in 73 neonates after stage 1 palliation for hypoplastic left heart syndrome. They demonstrated that cerebral rSO2 correlated poorly with low ScvO2, and they suggest that cerebral rSO2 not be used in isolation. This problem was somewhat ameliorated by correction of the signal for arterial contamination. NIRS appears to be too valuable a tool to be simply discarded, they said, suggesting that a perioperative risk assessment that would include multisite NIRS and hemodynamic monitoring might still allow early determination of low-cardiac output.
“Two numbers are better than one,” wrote Dr. Buratto and his colleagues. “Whether the NIRS technology will add any useful information to a simple bedside assessment by an astute clinician is yet to be seen.”
Edward Buratto, MBBS, Steve Horton, PhD, and Igor E. Konstantinov, MD, are from the Department of Cardiothoracic Surgery, The Royal Children’s Hospital; the Department of Pediatrics, University of Melbourne; and Murdoch Children’s Research Institute, Melbourne. They reported having no financial conflicts of interest.
The regional oxygenation index (rSO2) based on near infrared spectroscopy (NIRS) measurement is frequently used to assess the adequacy of oxygen delivery after stage 1 palliation of hypoplastic left heart syndrome (HLHS). However, a recent study showed that cerebral rSO2 has low sensitivity and should not be considered reassuring even at rSO2 of 50 or greater. In addition, values below 30 were not found to be sensitive for detecting compromised oxygen delivery, according to a report published online in the Journal of Thoracic and Cardiovascular Surgery.
Erin Rescoe, MD, of Boston Children’s Hospital, and her colleagues at Harvard Medical School, Boston, performed a retrospective study of 73 neonates assessed with cerebral venous oxyhemoglobin saturation (ScvO2) measured by co-oximetry from the internal jugular vein, which is considered the preferred method for assessing the adequacy of tissue oxygen delivery, compared with cerebral rSO2 after stage 1 palliation of HLHS (doi: 10.1016/j.jtcvs.2017.03.154).
To determine the suggested benefit of NIRS as an effective trend monitor, the researchers used their interpolated data to examine changes in rSO2 and changes in ScvO2 at hourly intervals and compared these values.Of particular concern is the result showing that, in all instances where ScvO2 was less than 30%, rSO2 was greater than 30%. In terms of the sensitivity (the true positive rate) and specificity (the true negative rate) of using NIRS, time-matched pairs of rSO2 and ScvO2 showed that the receiver operating characteristic curves for rSO2 as a diagnostic test to detect ScvO2 less than 30%, less than 40%, and less than 50% were 0.82, 0.84, and 0.87, respectively, showing good specificity, with a value of rSO2 less than 30% indicating that ScvO2 will be less than 30% 99% of the time.
“However, the sensitivity of rSO2 in the range of clinical interest in detecting ScvO2 less than 30% is extremely low,” according to the researchers. Thus, NIRS is likely to produce false negatives, missing patients with clinically low postoperative oxygen saturation.
In fact, rSO2 was less than 30% less than 1% of the time that ScvO2 was less than 30%. Similar results were seen in comparing values at the less than 40% mark (equivalent less than 1% of the time). Better results showed at the less than 50% mark, with equivalence seen 46% of the time.
NIRS measures a composite of arterial and venous blood, according to Dr. Rescoe and her colleagues. Therefore, to do a more direct comparison, they adjusted their NIRS results by calculating an rSO2-based ScvO2 designed to remove arterial contamination from the rSO2 signal: rSO2-based ScvO2 = (rSO2 arterial oxygen saturation x 0.3)/0.7.
This significantly improved the sensitivity of rSO2 to detect ScvO2 at less than 30% to 6.5%, to 29% for rSO2 at less than 40%, and 77.4% for rSO2 less than 50%.
The researchers “were surprised by the extremely low sensitivity of cerebral NIRS to detect even the most severe aberrations in DO2” (i.e., ScvO2 less than 30%, which has been found to be associated with poor outcomes).
“Cerebral rSO2 in isolation should not be used to detect low ScvO2, because its sensitivity is low, although correction of rSO2 for arterial contamination significantly improves sensitivity. Cerebral rSO2 of 50 or greater should not be considered reassuring with regard to ScvO2, although values less than 30 are specific for low ScvO2,” the researchers concluded.
The study was sponsored by the Gerber Foundation, the Hess Family Philanthropic Fund, and Boston Children’s Hospital Heart Center Strategic Investment Fund. The authors disclosed that they had no financial conflicts.
The regional oxygenation index (rSO2) based on near infrared spectroscopy (NIRS) measurement is frequently used to assess the adequacy of oxygen delivery after stage 1 palliation of hypoplastic left heart syndrome (HLHS). However, a recent study showed that cerebral rSO2 has low sensitivity and should not be considered reassuring even at rSO2 of 50 or greater. In addition, values below 30 were not found to be sensitive for detecting compromised oxygen delivery, according to a report published online in the Journal of Thoracic and Cardiovascular Surgery.
Erin Rescoe, MD, of Boston Children’s Hospital, and her colleagues at Harvard Medical School, Boston, performed a retrospective study of 73 neonates assessed with cerebral venous oxyhemoglobin saturation (ScvO2) measured by co-oximetry from the internal jugular vein, which is considered the preferred method for assessing the adequacy of tissue oxygen delivery, compared with cerebral rSO2 after stage 1 palliation of HLHS (doi: 10.1016/j.jtcvs.2017.03.154).
To determine the suggested benefit of NIRS as an effective trend monitor, the researchers used their interpolated data to examine changes in rSO2 and changes in ScvO2 at hourly intervals and compared these values.Of particular concern is the result showing that, in all instances where ScvO2 was less than 30%, rSO2 was greater than 30%. In terms of the sensitivity (the true positive rate) and specificity (the true negative rate) of using NIRS, time-matched pairs of rSO2 and ScvO2 showed that the receiver operating characteristic curves for rSO2 as a diagnostic test to detect ScvO2 less than 30%, less than 40%, and less than 50% were 0.82, 0.84, and 0.87, respectively, showing good specificity, with a value of rSO2 less than 30% indicating that ScvO2 will be less than 30% 99% of the time.
“However, the sensitivity of rSO2 in the range of clinical interest in detecting ScvO2 less than 30% is extremely low,” according to the researchers. Thus, NIRS is likely to produce false negatives, missing patients with clinically low postoperative oxygen saturation.
In fact, rSO2 was less than 30% less than 1% of the time that ScvO2 was less than 30%. Similar results were seen in comparing values at the less than 40% mark (equivalent less than 1% of the time). Better results showed at the less than 50% mark, with equivalence seen 46% of the time.
NIRS measures a composite of arterial and venous blood, according to Dr. Rescoe and her colleagues. Therefore, to do a more direct comparison, they adjusted their NIRS results by calculating an rSO2-based ScvO2 designed to remove arterial contamination from the rSO2 signal: rSO2-based ScvO2 = (rSO2 arterial oxygen saturation x 0.3)/0.7.
This significantly improved the sensitivity of rSO2 to detect ScvO2 at less than 30% to 6.5%, to 29% for rSO2 at less than 40%, and 77.4% for rSO2 less than 50%.
The researchers “were surprised by the extremely low sensitivity of cerebral NIRS to detect even the most severe aberrations in DO2” (i.e., ScvO2 less than 30%, which has been found to be associated with poor outcomes).
“Cerebral rSO2 in isolation should not be used to detect low ScvO2, because its sensitivity is low, although correction of rSO2 for arterial contamination significantly improves sensitivity. Cerebral rSO2 of 50 or greater should not be considered reassuring with regard to ScvO2, although values less than 30 are specific for low ScvO2,” the researchers concluded.
The study was sponsored by the Gerber Foundation, the Hess Family Philanthropic Fund, and Boston Children’s Hospital Heart Center Strategic Investment Fund. The authors disclosed that they had no financial conflicts.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:
Major finding: In terms of sensitivity, rSO2 was less than 30% less than 1% of the time that ScvO2 was less than 30%.
Data source: A retrospective single institution study of 73 neonates assessed after stage 1 palliation
Disclosures: The study was sponsored by the Gerber Foundation, the Hess Family Philanthropic Fund, and Boston Children’s Hospital Heart Center Strategic Investment Fund. The authors disclosed that they had no financial conflicts.