News
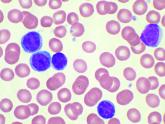
Patients with CLL have significantly reduced response to COVID-19 vaccine
- Author:
- Mark S. Lesney
- Phd
Less than half of CLL patients had an antibody-mediated response to the Pfizer vaccine in a study.
News
Combo drug improves survival in older patients with high-risk/secondary AML
- Author:
- Mark S. Lesney
CPX-351 therapy was tied to long-term remission and survival in older patients with newly diagnosed high-risk or...
News

FDA approves twice-daily formulation of key thalassemia drug
- Author:
- Mark S. Lesney
The new formulation of twice-a-day Ferriprox 1,000 mg oral tablets eliminates the midday dose.
News
Vaccination regimen effective in preventing pneumonia in MM patients
- Author:
- Mark S. Lesney
Vaccination was effective despite the expected decrease in immunological response during target and...
News
Race and location appear to play a role in the incidence of CLL and DLBCL
- Author:
- Mark S. Lesney
Urban non Hispanic blacks and Hispanics have an increased incidence of CLL, DLBCL, respectively vs. rural....
News
Secondary acute lymphoblastic leukemia more lethal than de novo
- Author:
- Mark S. Lesney
Adult patients with secondary ALL had poorer overall survival than de novo ALL patients.
News
Protective levels of vitamin D achievable in SCD with oral supplementation
- Author:
- Mark S. Lesney
Vitamin D3 prophylaxis is a safe practice in sickle cell disease, and it is important to start this prophylactic treatment when the child is an...
News
DLBCL patients at academic centers had significantly better survival
- Author:
- Mark S. Lesney
Researchers suggested that academic centers might provide increased access to clinical trials, improved physician expertise, improved treatment...
News
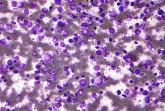
Interleukin-27 increased cytotoxic effects of bone marrow NK cells in CLL
- Author:
- Mark S. Lesney
Interleukin-27 was able to increase cytotoxic effects of bone marrow natural killer cells in chronic lymphocytic leukemia (CLL).
News
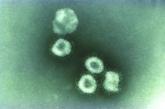
SARS-CoV-2 present significantly longer in stool than in respiratory, serum samples
- Author:
- Mark S. Lesney
SARS-CoV-2 is present significantly longer in samples from severe COVID-19 patients than from patients with mild...
News
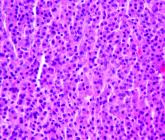
Combo therapy with melflufen promising in small r/r multiple myeloma study
- Author:
- Mark S. Lesney
Melflufen plus dexamethasone showed activity in patients with relapsed/refractory multiple myeloma.
News
REACH2: Ruxolitinib outperformed control treatment for refractory acute GVHD
- Author:
- Mark S. Lesney
Ruxolitinib was significantly more effective against acute graft-versus-host disease but produced more thrombocytopenia than did control treatment...
News
Five prognostic indexes come up short for planning early CLL treatment
- Author:
- Mark S. Lesney
None of the indexes was able to predict with total precision the clinical evolution of Binet A chronic...
News
EHA and TIF explore how COVID-19 is affecting thalassemia and SCD patients
- Author:
- Mark S. Lesney
Thalassemia patients appeared to fare relatively well after COVID-19 diagnosis in anecdotal series reports from...
News
CLAM trial regimen shown safe, effective for r/r AML
- Author:
- Mark S. Lesney
High response rates and effective bridge to transplant shown.
