User login
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
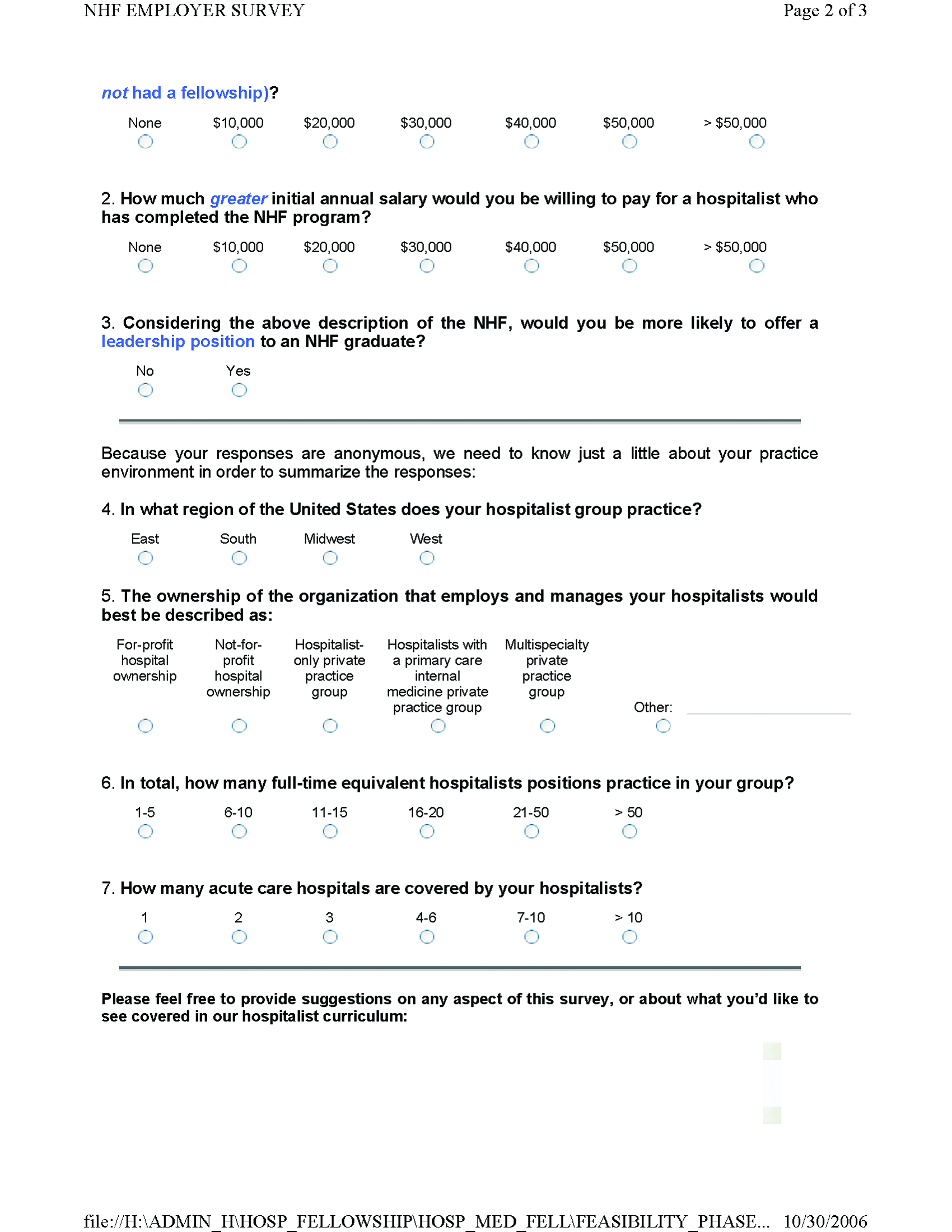
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
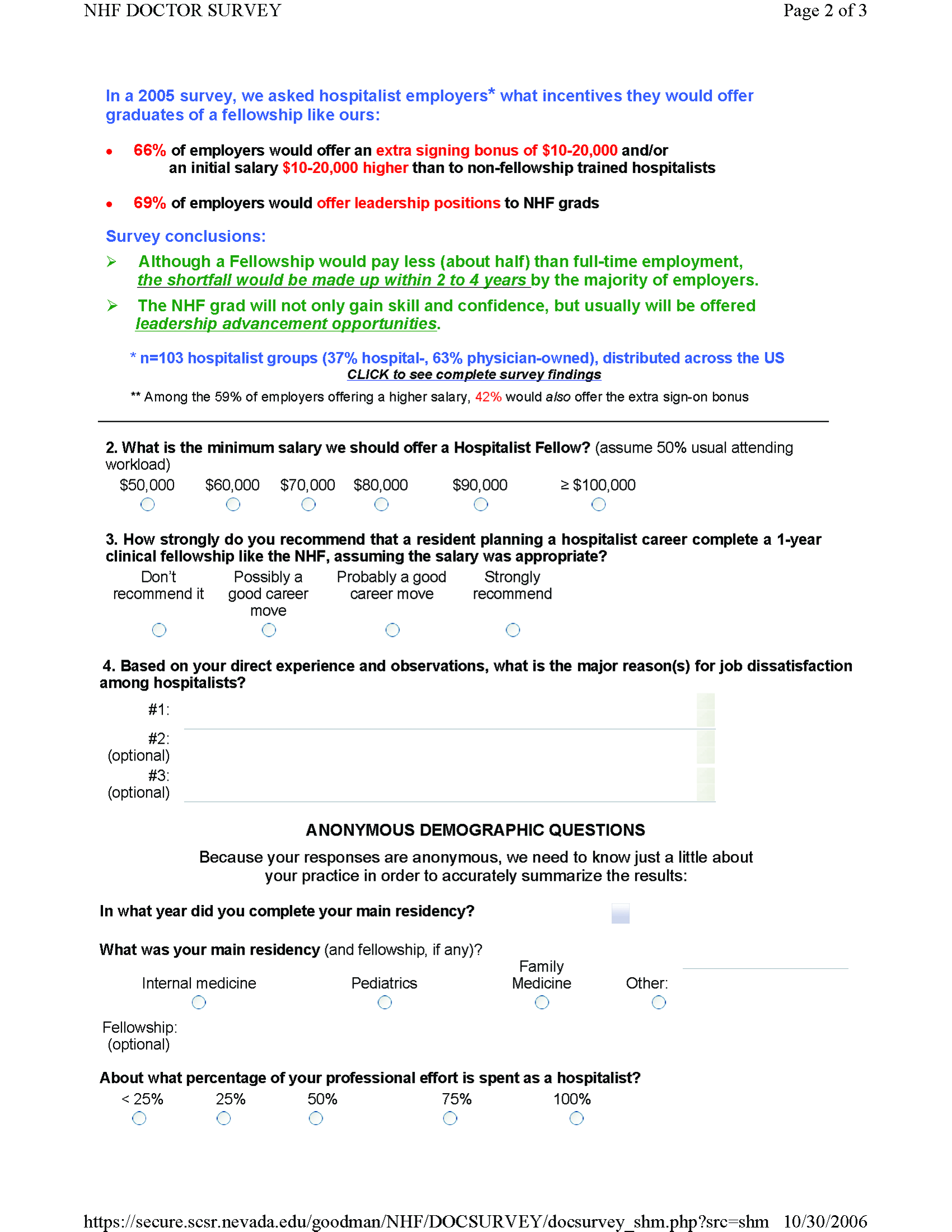
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
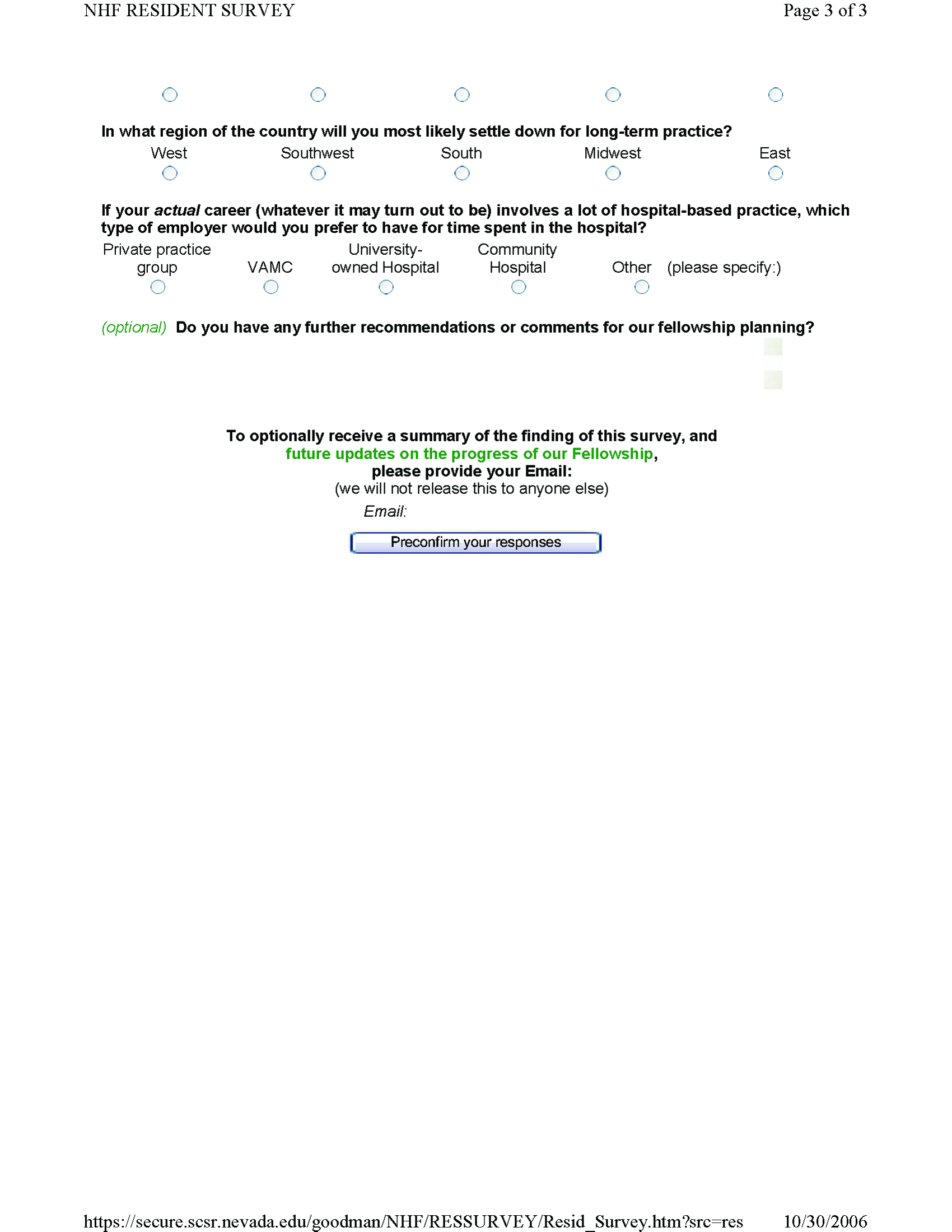
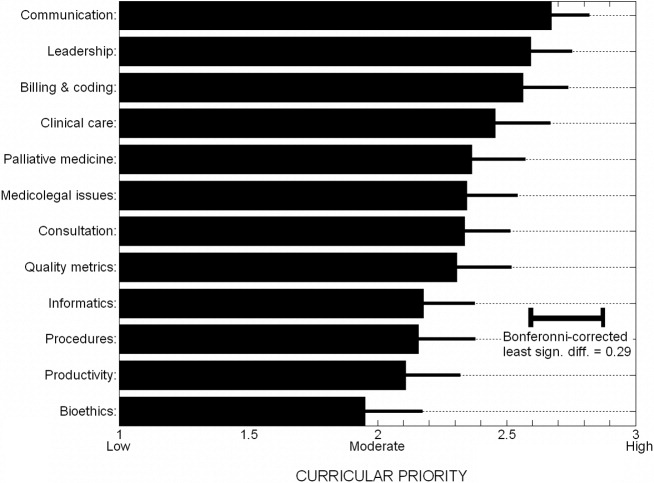
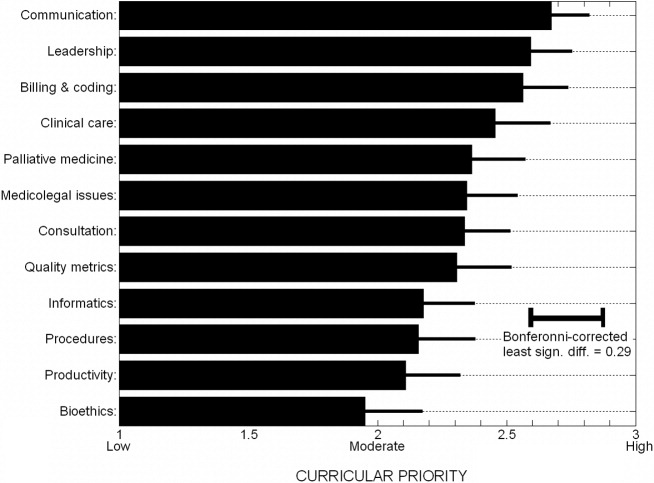
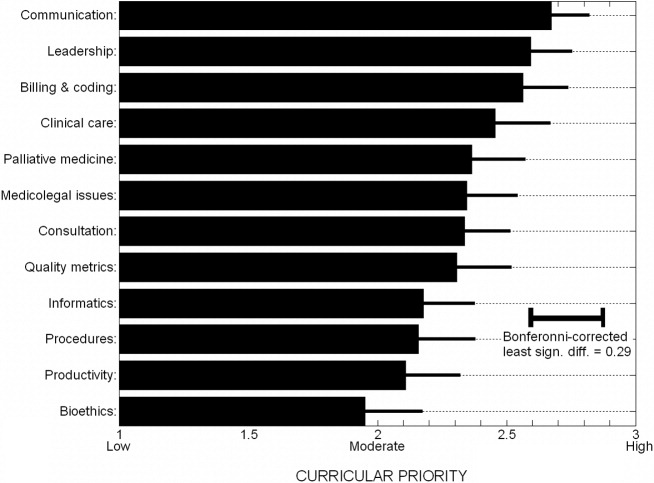
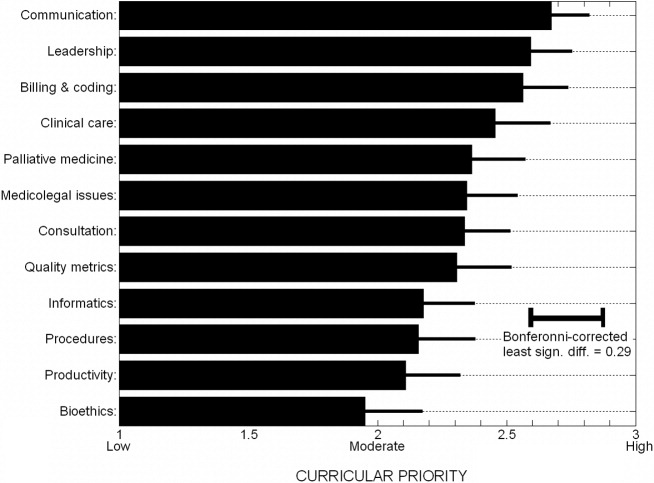
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
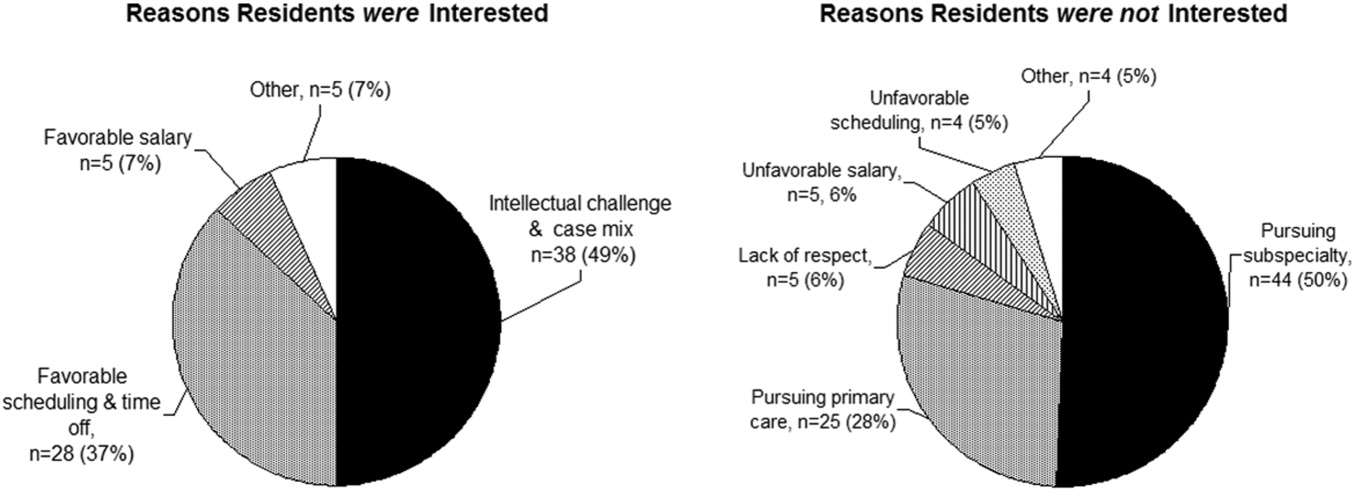
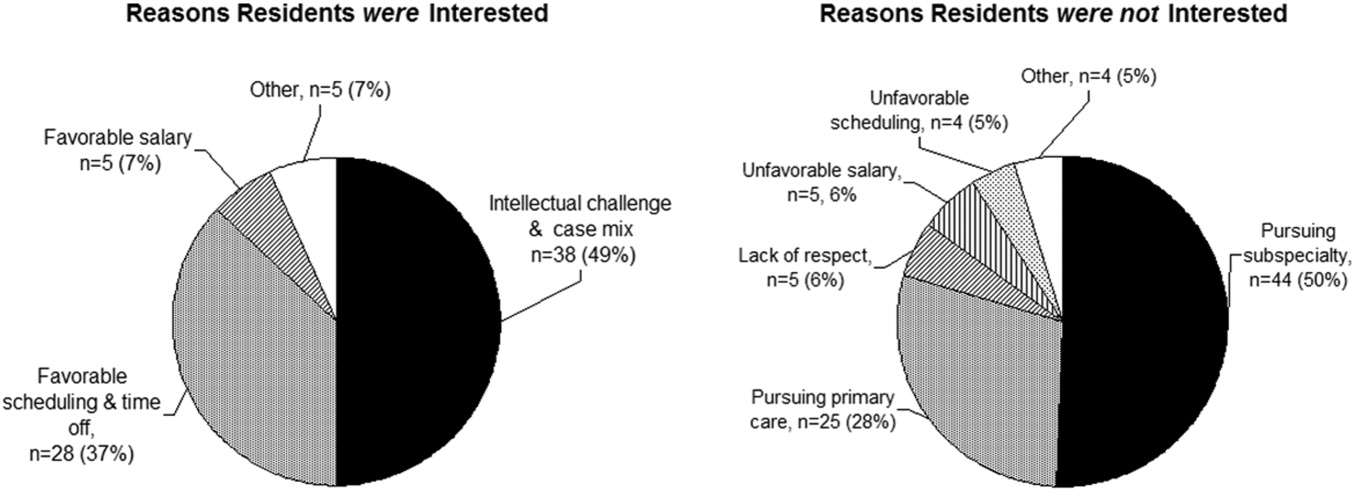
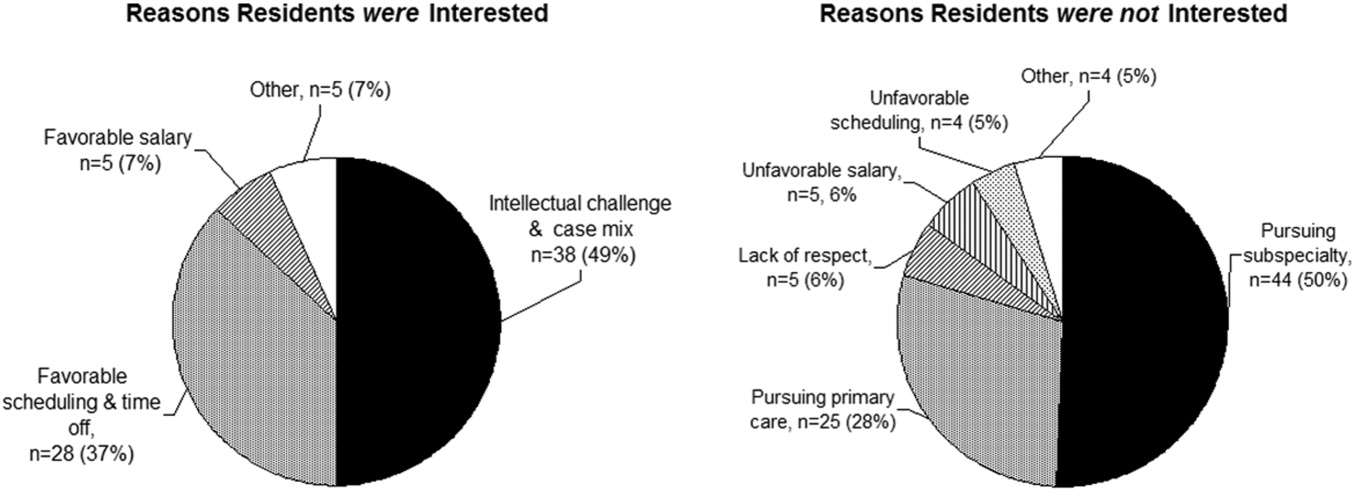
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
The demand for hospital medicine specialists continues to grow at nearly an exponential pace.1 Society of Hospital Medicine (SHM) practice estimates rose from 2000 in 1998 to 15,000 in 2005, with a projection of 30,000 for 2010.2 Most new positions are filled by graduates of internal medicine and pediatric residencies without postgraduate fellowship training. However, as hospital medicine specialists increasingly provide not only direct care but also team leadership and quality improvement, basic residency training alone may not suffice to provide the required skill sets. In addition, the career satisfaction of hospitalists depends in large part on the esteem of colleagues in other specialties. Ready availability for emergency department admissions and inpatient consults, coupled with an absence of postgraduate clinical training and board certification,3 may promote a view of the hospitalist as a perpetual resident‐like workhorse rather than as a professional peer.
Clinical hospital medicine fellowships could address the needs both to expand skill sets and to elevate the perceived stature of the profession. To date, only a small number of hospital medicine fellowships have been created,4 and all but a few are intended to train academic educators rather than produce hospitalists for the emerging clinical marketplace.5 Furthermore, a fellowship curriculum would incorporate the advanced training in group dynamics and interpersonal communication needed to lead the increasing number of increasingly diverse hospitalist groups.1
In considering a clinical hospital fellowship for the reasons above, the University of Nevada School of Medicine sought first to address several potential obstacles:
Curriculum. What is the proper balance of mentored clinical service and didactic coursework? How should quality improvement be taught? What emphasis should be placed on business and medicolegal aspects of the profession?
Salary. Would a prospective fellow be willing to defer practice income during the training period? Will future employers compensate for this by rewarding clinical fellowshiptrained hospitalists with bonuses, higher initial salaries, or leadership positions?
Reality check. Do practicing hospitalists regret not having had the opportunity to train in a clinical fellowship environment? Will current residents in training actually apply for such fellowships?
METHODS
Over the course of 7 months in late 2005 and early 2006, we administered a linked sequence of three nation‐wide surveys: Survey I to hospitalist employers, Survey II to practicing hospitalists, and Survey III to internal medicine residents. Although we roughed out the general structure of all surveys in advance, we awaited the main results of the first survey to be incorporated into the second, and the results of the first two into the third (see below). All surveys were created using PHP as the interface language between the user and a MySQL relational database running on our university server, conducted over secure encrypted Web connections. Surveys I‐III were field‐tested and amended based on the responses of focus groups of local employers, hospitalists, and residents, respectively. In addition to required responses targeting the perspectives of the recipient, all surveys requested optional demographic information. Although the surveys were anonymous, an option was provided for respondents to receive a compilation of the results of all 3 surveys by E‐mail. The proposal was screened by our university institutional review board and determined to be exempt from human subjects review.
Survey Methods
Survey I: Employers.
We created an electronic database by extracting employer contact information from all classified advertisements placed between January and June 2005 in the New England Journal of Medicine, JAMA, Today's Hospitalist, Annals of Internal Medicine, and SHM's The Hospitalist. Almost all employers included in their ad or otherwise provided on phone inquiry an E‐mail address to which we sent a request with a link to the Web‐based survey (Supplemental Fig. S1). The remaining employers were faxed a copy of the survey to complete and return by fax or mail. We made up to 3 attempts (including a final phone call attempt) to request a response before considering an employer a nonrespondent. The survey asked employers to indicate how much sign‐on bonus and greater initial salary they would offer a clinical fellowshiptrained graduate and whether such a person would be more likely to be offered a leadership position. Open‐ended comments were sought. Demographic questions related to geographic region, group ownership, number of hospitalists employed, and number of hospitals covered.
Survey II: Hospitalists.
The SHM sent an E‐mail message on our behalf to its roster of practicing hospitalist members. The E‐mail included a link to our Web‐based survey (Supplemental Fig. S2). We asked the hospitalists to suggest a minimum fellowship salary (assuming a 50% clinical workload), to rate the value of a clinical fellowship as a career move, to indicate their perception of causes of dissatisfaction among current hospitalists, and to prioritize each of 12 broad curricular topics as low, medium, or high (open‐ended suggestions were also sought). Demographic questions related to residency and fellowship training, current practice, and perceived likelihood to still be practicing hospital medicine in 5 years.
Survey III: Residents.
We compiled an E‐mail database of internal medicine programs from the Association of Program Directors in Internal Medicine (APDIM) Web site and the ACGME Medical Education Directory (informally known as the green book). Each program director was E‐mailed the rationale for our survey and summary findings from Surveys I and II, with an appended link to our online survey (Supplemental Fig.S3). We made up to 3 E‐mail attempts before considering a program director to be a nonrespondent (confirmation was either by the director or indirectly determined by the E‐mail server domains of responding residents). The survey asked about the resident's likelihood of pursuing a hospitalist career, followed by a hypothetical question: assuming the resident were to become a hospitalist, and knowing the results of Surveys I and II, how likely would the resident be to pursue a clinical hospital medicine fellowship following residency? We also allowed open‐ended responses about the main reasons a resident would or would not consider hospital medicine as a career. Demographic questions concerned current PGY level, geographic region of residency, anticipated future practice, and preferred type of future employer.
Statistical Methods
Central tendencies are expressed or plotted as mean standard deviation or as median with interquartile range, as appropriate to the type of measurement. Because most responses were intended to describe interest and perception rather than to test specific hypotheses, significance testing (SYSTAT, San Jose, CA) was limited to selected responses, using Pearson chi‐square to test for equality of 2 proportions, the Cochran test for linear trend of hospital career interest across the 3 PGY levels, and analysis of variance with Bonferroni correction for least significant differences among prioritized curricular topics.
RESULTS
Survey I (Employers)
Demographics.
Among 241 unique journal classified advertisement sources, we identified 195 representing direct employers of hospitalists, rather than recruitment firms. Of these, 103 (52.8%) completed the survey. Representatives of only 5 employers actively declined to complete the survey, indicating that they were not in positions of authority to provide the information needed.
Table 1 shows that the employers were distributed across the United States, and balanced among hospital‐owned and private group (including academic) ownership (38% vs. 51%, respectively). Although 70% of groups employed at most 15 hospitalists, 20% employed 16‐50, and 10% employed the equivalent of more than 50 full‐time hospitalists. Most groups covered a single hospital, but the remainder distributed their workload over a wide range of facilities.
| Category | n | (%) |
|---|---|---|
| Location | ||
| East | 22 | (21.8) |
| South | 17 | (16.8) |
| Midwest | 32 | (30.7) |
| West | 32 | (30.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 38 | (36.9) |
| For‐profit hospital ownership | 2 | (1.9) |
| Not‐for‐profit hospital ownership | 36 | (35.0) |
| PRACTICE OWNERSHIP | 51 | (49.5) |
| Hospitalist‐only private practice group | 24 | (23.3) |
| Hospitalists within primary care private practice group | 3 | (2.9) |
| Multispecialty private practice group | 24 | (23.3) |
| OTHER | 14 | (13.6) |
| Number of FTE Practicing in the Group | ||
| 1‐5 FTE hospitalists | 28 | (27.2) |
| 6‐10 FTE hospitalists | 31 | (30.1) |
| 11‐15 FTE hospitalists | 13 | (12.6) |
| 16‐50 FTE hospitalists | 21 | (20.4) |
| >50 FTE hospitalists | 10 | (9.7) |
| Number of Hospitals Covered by the Group | ||
| 1 Hospital covered | 54 | (52.4) |
| 2 Hospitals covered | 13 | (12.6) |
| 3 Hospitals covered | 10 | (9.7) |
| 6 Hospitals covered | 10 | (9.7) |
| >6 Hospitals covered | 16 | (15.5) |
Primary Measures.
Two‐thirds of employers would offer either a signing bonus or a starting salary increase of at least $10,000 to those coming out of clinical fellowship training; a quarter would offer a bonus and a higher salary (Table 2). More than 20% of employers would offer an initial salary that was at least $20,000 higher. Leadership positions would be considered by 69% of employers.
| Category | n | (%) |
|---|---|---|
| Signing bonus offer | ||
| No bonus | 70 | (68.6) |
| Bonus $10,000 | 32 | (31.4) |
| Bonus $20,000 | 6 | (5.9) |
| Higher initial salary offer | ||
| No increase | 42 | (41.2) |
| Increase $10,000 | 60 | (58.8) |
| Increase $20,000 | 23 | (22.5) |
| Either signing bonus OR higher salary offer | 67 | (65.7) |
| Both signing bonus AND higher salary offer | 25 | (24.5) |
| Leadership position offer | 71 | (68.9) |
Survey II (Hospitalists)
Demographics.
One hundred and one practicing hospitalists responded to the SHM E‐mail request. The SHM membership office estimates that the survey was sent to deliverable E‐mail addresses of approximately 2300 physicians, of whom approximately 68% (1560) were internists; based on this, our response rate was approximately 6.5%.
Table 3 shows that practicing hospitalists were predominantly internists (88%). They were evenly distributed across the nation and between hospital‐owned groups (46%) and privately owned groups (46%); the latter included medical school practice plans (18% of respondents). Of the respondents, 75% were full‐time hospitalists, and only 1 worked less than 0.25 the equivalent of full‐time. They had graduated a median of 8 years earlier (interquartile range, 6 years; range, 1970‐2005).
| Category | n | (%) |
|---|---|---|
| ||
| Practice region | ||
| East | 32 | (31.7) |
| South | 21 | (20.8) |
| Midwest | 22 | (21.8) |
| West | 26 | (25.7) |
| Ownership of employing organization | ||
| HOSPITAL OWNERSHIP | 46 | (45.5) |
| For‐profit hospital ownership | 4 | (4.0) |
| Not‐for‐profit hospital ownership | 42 | (41.6) |
| PRACTICE OWNERSHIP | 46 | (45.5) |
| Hospitalist‐only private practice group | 7 | (6.9) |
| Hospitalists within primary care private practice group | 9 | (8.9) |
| Multispecialty private practice group | 12 | (11.9) |
| Medical school practice plan | 18 | (17.8) |
| OTHER | 9 | (8.9) |
| Professional effort as hospitalist | ||
| 100% FTE | 76 | (75.3) |
| 75% FTE | 13 | (12.9) |
| 50% FTE | 6 | (5.9) |
| 25% FTE | 5 | (5.0) |
| <25% FTE | 1 | (1.0) |
| Residency Training* | ||
| Internal medicine | 89 | (88.1) |
| Pediatrics | 6 | (5.9) |
| Family medicine | 5 | (5.0) |
| Other | 1 | (1.0) |
Primary Measures.
On average, practicing hospitalists ranked essentially all 12 curricular topics between moderate and high priority. Figure 1 displays the scores sorted by means with standard deviations; any pairwise difference between 2 means greater than 0.286 corresponds to a Bonferroni‐corrected P value < .05. Communication, leadership, and coding skills averaged above 2.5 (ie, closer to high than moderate priority), and bioethics ranked the lowest. There was no overall obvious clustering of topics, with administrative and clinical topics interspersed across the ratings. Respondents offered no separate topics in their open‐ended responses, but recommended subtopics to be included, such as contract negotiation, training for effective committee involvement, dealing with families, consultative medicine, and ICU comanagement. Several respondents also suggested tailoring the weighting of the curricular emphasis according to the needs and experience of individual fellows in each cohort.
Of the practicing hospitalists, 81% believed that clinical fellowship could be a good career move (Table 4), and 59% believed that graduating residents probably or strongly should consider such fellowship training. The median response to the question of minimum salary we should offer a hospitalist fellow was $70,000, with 80% of responses between $50,000 and $90,000.
| Category | n | (%) |
|---|---|---|
| ||
| Strength of recommendation to pursue fellowship | ||
| RECOMMEND | 92 | (91.1) |
| Possibly a good career move | 33 | (32.7) |
| Probably a good career move | 37 | (36.6) |
| Strongly recommend | 22 | (21.8) |
| DON'T RECOMMEND | 9 | (8.9) |
| Fellowship salary* | ||
| $50,000 | 11 | (10.9) |
| $60,000 | 24 | (23.8) |
| $70,000 | 30 | (29.7) |
| $80,000 | 20 | (19.8) |
| $90,000 | 8 | (7.9) |
| $100,000 | 8 | (7.9) |
| Likelihood of practicing hospital medicine in 5 years | ||
| Very likely | 69 | (68.3) |
| Somewhat likely | 17 | (16.8) |
| Somewhat unlikely | 10 | (9.9) |
| Very unlikely | 5 | (5.0) |
| Perceived reasons for job dissatisfaction | ||
| INTERNAL FACTORS | 166 | (71.0) |
| Excess workload | 80 | (34.2) |
| Scheduling frustrations | 32 | (13.7) |
| Organizational leadership and administrative problems | 24 | (10.2) |
| Inadequate salary | 16 | (6.8) |
| Productivity pressures | 14 | (6.0) |
| EXTERNAL FACTORS | 78 | (29.0) |
| Interaction, communication problems within hospital | 29 | (12.4) |
| Mistreatment, lack of professional respect | 28 | (12.0) |
| Other | 11 | (4.7) |
When asked about their future plans, 69% were very likely to be practicing hospital medicine in 5 years (Table 4). Major reasons for career dissatisfaction were aggregated into 5 categories, 3 of which pertained to internal group management (accounting for 71% of concerns) and the others to external interactions in the hospital milieu (Table 4).
Survey III (Residents)
Demographics.
Two hundred and seventy‐nine categorical medicine residents responded to the survey link forwarded by their program director, 43% of whom requested a follow‐up summary of overall survey findings. Based on a total of 385 medicine program directors sent an E‐mail request and the E‐mail domain servers of the respondents, we estimate that about 70 program directors (18%) forwarded surveys to their residents.
Without respect to subspecialty choice, 75% of the 279 categorical residents planned to stay in their region after graduation; among the 25% planning to relocate, most were moving from the East or South to the West or Southwest (Table 5). Interestingly, no residents in the Southwest and the West planned to leave their region of current training. Overall, 40% were academically oriented. About 35% planned to work for a hospital entity, and about 20% planned to work in a private group.
| Category | n | (%) |
|---|---|---|
| ||
| Present residency program location | ||
| East | 129 | (46.2) |
| Midwest | 92 | (33.0) |
| South | 20 | (7.2) |
| Southwest* | 3 | (1.1) |
| West* | 35 | (12.5) |
| Anticipated future practice location | ||
| Eastern | 95 | (34.1) |
| Midwest | 78 | (28.0) |
| South | 36 | (12.9) |
| Southwest* | 14 | (5.0) |
| West* | 56 | (20.1) |
| Probably or definitely will do hospitalist career | ||
| PGY1 (n = 76) | 36 | (47.3) |
| PGY2 (n = 95) | 37 | (38.9) |
| PGY3 (n = 96) | 44 | (45.8) |
| Chiefs (n = 12) | 6 | (50.0) |
| Overall (n = 279) | 123 | (44.1) |
| Probably or definitely will do hospitalist career AND probably or definitely will do fellowship | ||
| PGY1 (n = 76) | 24 | (31.6) |
| PGY2 (n = 95) | 24 | (25.3) |
| PGY3 (n = 96) | 21 | (21.9) |
| Chiefs (n = 12) | 1 | (8.3) |
| Overall (n = 279) | 70 | (25.1) |
Primary Measures.
One hundred and twenty‐three of the 279 categorical residents (44%) were strongly considering a hospitalist career. There was no significant difference in the proportion of interest across PGY 1‐3 level (P = .48). Seventy of these 123 (57%) would likely pursue a clinical hospital medicine fellowship if it was available to them. Although there was increasing fellowship interest, with interest by PGY1 residents greater than that of PGY2 residents, which was greater than of PGY3 residents, but this trend did not reach statistical significance (Cochrane linear trend, P = .15).
One hundred and forty‐seven of the 279 categorical residents (53%) offered reasons for interest (or lack of interest) in a hospital medicine career (Fig. 2). The predominant attractions (Fig. 2A) were the intellectual challenge and variety of cases encountered in general acute care (49%) and the flexibility in work scheduling and time off (37%). Reasons offered for not pursuing hospital medicine were mainly the intention to purse subspecialty or primary care medicine; remaining factors (from a relatively small number of responders) included perceptions of a lack of professional respect and unfavorable salary or scheduling (Fig. 2B).
DISCUSSION
The increasing demand for hospitalist care has outstripped the supply of physicians available to do the job and as a result of the unmet demand; in our study, two‐thirds of employers were willing to pay more, either through a signing bonus or a starting salary increase of at least $10,000 to fellowship graduates (with more than 20% willing to pay at least $20,000 above the initial salary). The value of enhancing organizational and communication skills was also recognized, as shown by the readiness of about 70% of employers to offer leadership positions to clinical fellowshiptrained hospitalists.
Residents drawn to hospital medicine were mainly attracted by the flexible scheduling and intellectual challenge (Fig. 2). Lack of interest mainly reflected plans to enter other subspecialties or primary care, rather than apprehension about professional frustrations. Practicing hospitalists, however, related substantial professional concerns arising from both internal factors (predominantly excessive workload) and external sources (respect from other physicians and interdisciplinary hospital communication issues). An alarming 31% were not very likely to remain in the practice of hospital medicine beyond the next 5 years. Fellowship training could indirectly address workload issues by creating leaders skilled in scheduling and team building and could directly enhance communication and team‐building skills and generate esteem among professional peers.
Would residents forgo a year of greater salary to pursue a fellowship? Based on the SHM estimate of a median salary of $169,000 and a leadership salary gradient of $12,0006 and Survey III median recommendation for a fellowship salary of $70,000, a 1‐year fellow would face a potential loss of income of about $100,000. Using the Survey I findings above and the leadership gradient, this could be recouped within about 5 years. Of course, it is difficult to assign a dollar value to the additional intangible benefits attributable to enhanced career satisfaction and greater effectiveness in affecting hospital care dynamics. The $70,000 salary proposed (higher than most traditional fellowships offer) corresponds to revenue collected from the proposed clinical workload of 50% that of a full‐time hospitalist; programs would thus need to identify other sources to cover supervisory and teaching overhead. Residents considering a hospital medicine career apparently did appreciate the deferred value of an investment in hospital fellowship: having been provided the results of the employer and hospitalist surveys, 57% would likely pursue a clinical fellowship if available. Extrapolating to the national pool of about 6600 annual graduates of internal medicine residencies, a 44% overall rate of hospital medicine career interest, with 57% fellowship interest, would yield about 550 fellowship candidates annually (this is an upper bound overestimate, given the relatively large proportion of our respondents with interest in an academic career).
The validity of the 12 proposed curricular topics is supported by the rating of all topics as moderate to high priority by practicing hospitalists (Fig. 1) and is consistent with the recently published SHM Core Competencies.7 Significant differences were found for topics rated in the lower versus upper half of the response range, without obvious clustering of clinical or administrative topics. Communication, leadership, and billing and coding were rated as top priorities, training in quality metrics and consultation were intermediate, and bioethics was given the lowest relative priority (although still considered moderately important). Although no novel additional topics were generated in open‐ended responses, several suggested tailoring the curricular emphasis according to the needs and prior experience of individual fellows in a cohort.
Generalization of our findings is limited by the low response rates of both hospitalist and resident physicians. It is likely that responding hospitalists were more interested than nonresponders in the concept of clinical hospital medicine fellowships. The strength of recommendation of fellowship training should therefore be considered an upper bound. The other main questions, pertaining to salary and curriculum, would presume a sufficient interest among responders and thus be less susceptible to sampling bias. Regarding resident response, we do not know the number of questionnaires actually forwarded by program directors to their residents. However, given that most responding residents were not planning to be hospitalists, we have at least a relatively representative sample of the attitudes of both uninterested and interested residents.
In summary, the results of our national surveys of hospitalist employers, practicing hospitalists, and current internal medicine residents reveals a potentially unmet demand for the provision of clinical hospital medicine fellowships. Curricular development under the leadership of organizations such as the Society of Hospital Medicine could hasten this development.
Acknowledgements
We thank Beverly Parker, MD, UNSOM Reno internal medicine program director, for her suggestions on the resident survey, and the SHM for e‐mail distribution of the survey of practicing hospitalists.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- Society of Hospital Medicine. Growth of Hospital Medicine in North America. 2006 projection. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/ Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm.
- .Come together: key leaders in internal medicine call for a revision in residency training.Hospitalist.2006:5.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- Society of Hospital Medicine fellowship tracking link. Updated January,2006. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/HospitalMedicinePrograms/Hospital_Medicine_Pr.htm.
- Society of Hospital Medicine. Authoritative source on the state of hospital medicine: executive summary. SHM2006. Available at: http://www.hospitalmedicine.org.
- Pistoria JM, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1 (suppl 1).
Copyright © 2008 Society of Hospital Medicine