User login
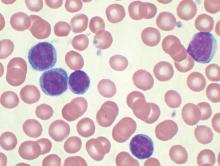
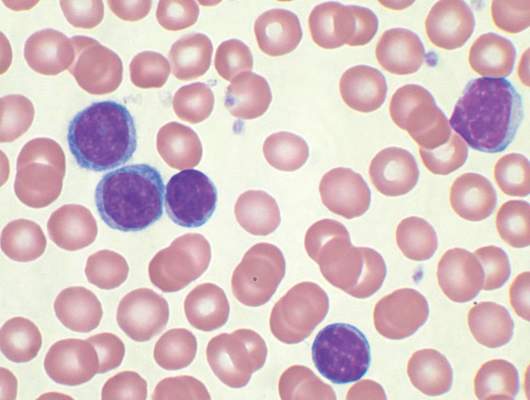
Exosomes released by chronic lymphocytic leukemia (CLL) cells induce stromal cells to adopt a cancer-associated fibroblast phenotype, thereby creating a microenvironment conducive to CLL cell adhesion, survival, and growth.
Although the role of exosomes in other cancers has been well studied, their role in hematologic malignancies has not been well characterized. Also, this study confirmed that exosomes are present in CLL lymph nodes and promote tumor growth in vivo.
“Our in vitro and in vivo data show that CLL exosomes harbor an oncogenic potential by stimulating stromal cells to induce an inflammatory and protumorigenic milieu, including increased angiogenesis, thus supporting the survival and outgrowth of CLL cells,” wrote Jerome Paggetti, Ph.D., of the laboratory of experimental hemato-oncology, Luxembourg Institute of Health (Blood 2015 Aug 27. doi:10.1182/blood-2014-12-618025).
Cells were obtained from 21 CLL patients; all patients had an absolute lymphocyte count of more than 30,000/mcL and were untreated for 3 months. The researchers established 30-day cocultures of bone marrow mesenchymal stem cells with primary CLL cells in culture inserts or they treated bone marrow mesenchymal stem cells weekly with exosomes. Similar experiments were performed with the Burkitt lymphoma cell line Namalwa to investigate whether the impact on stromal cells is CLL specific.
Based on gene expression analysis, CLL exosomes and CLL cells cocultured in inserts induced similar gene expression changes in bone marrow mesenchymal stem cells, highlighting the relevance of exosomes for microenvironment changes. “Importantly, lymphoma cells induced a distinct gene expression pattern in bone marrow mesenchymal stem cells, suggesting a specific response to CLL exosomes,” wrote Dr. Paggetti and coauthors.
The impact of CLL exosomes on tumor growth was studied in vivo by subcutaneously injecting cells with and without CLL exosomes into immunocompromised mice. Cells supplemented with exosomes resulted in an increased tumor size compared with tumor cells injected without additional exosomes. Also, the cells supplemented with exosomes accumulated in mice kidneys, confirming the renal involvement observed in CLL patients. “Our data demonstrate a protumorigenic effect of CLL-derived exosomes in vivo and their importance in the early onset of the disease when tumor cells impact the microenvironment to proliferate and promote angiogenesis,” the researchers concluded.
Chronic lymphocytic leukemia results in clonal expansion and invasive migration of cells that infiltrate the lymph nodes and bone marrow. Understanding the tumor microenvironment and the communication that occurs between malignant cells and their surroundings is imperative to improving cancer therapies.
Alongside well-studied signaling mechanisms involving cytokines, growth factors, and receptors, exosome shedding has emerged recently as a key player in cancer signaling. Paggetti et al. comprehensively analyzed CLL-derived exosomes and provided functional data illustrating the impact of exosomes on the tumor microenvironment by reprogramming healthy stromal cells into cancer-associated fibroblasts.
The RNA and proteins delivered by exosomes to stromal cells induce an inflammatory phenotype characteristic of cancer-associated fibroblasts.
The work supports the theory that tumor cell induction of cancer-associated fibroblasts is a universal feature of progression in both solid and blood cancers. Continued research may identify novel therapies that reconfigure the tumor microenvironment for antitumorigenic effect.
Dr. Benedetta Apollonio is a researcher and Dr. Alan Ramsey is a senior lecturer in lymphoma biology at King’s College, London. Their remarks were part of an editorial accompanying the report (Blood 2015 Aug 27. doi:10.1182/blood-2015-07-655233). The authors had no disclosures to report.
Chronic lymphocytic leukemia results in clonal expansion and invasive migration of cells that infiltrate the lymph nodes and bone marrow. Understanding the tumor microenvironment and the communication that occurs between malignant cells and their surroundings is imperative to improving cancer therapies.
Alongside well-studied signaling mechanisms involving cytokines, growth factors, and receptors, exosome shedding has emerged recently as a key player in cancer signaling. Paggetti et al. comprehensively analyzed CLL-derived exosomes and provided functional data illustrating the impact of exosomes on the tumor microenvironment by reprogramming healthy stromal cells into cancer-associated fibroblasts.
The RNA and proteins delivered by exosomes to stromal cells induce an inflammatory phenotype characteristic of cancer-associated fibroblasts.
The work supports the theory that tumor cell induction of cancer-associated fibroblasts is a universal feature of progression in both solid and blood cancers. Continued research may identify novel therapies that reconfigure the tumor microenvironment for antitumorigenic effect.
Dr. Benedetta Apollonio is a researcher and Dr. Alan Ramsey is a senior lecturer in lymphoma biology at King’s College, London. Their remarks were part of an editorial accompanying the report (Blood 2015 Aug 27. doi:10.1182/blood-2015-07-655233). The authors had no disclosures to report.
Chronic lymphocytic leukemia results in clonal expansion and invasive migration of cells that infiltrate the lymph nodes and bone marrow. Understanding the tumor microenvironment and the communication that occurs between malignant cells and their surroundings is imperative to improving cancer therapies.
Alongside well-studied signaling mechanisms involving cytokines, growth factors, and receptors, exosome shedding has emerged recently as a key player in cancer signaling. Paggetti et al. comprehensively analyzed CLL-derived exosomes and provided functional data illustrating the impact of exosomes on the tumor microenvironment by reprogramming healthy stromal cells into cancer-associated fibroblasts.
The RNA and proteins delivered by exosomes to stromal cells induce an inflammatory phenotype characteristic of cancer-associated fibroblasts.
The work supports the theory that tumor cell induction of cancer-associated fibroblasts is a universal feature of progression in both solid and blood cancers. Continued research may identify novel therapies that reconfigure the tumor microenvironment for antitumorigenic effect.
Dr. Benedetta Apollonio is a researcher and Dr. Alan Ramsey is a senior lecturer in lymphoma biology at King’s College, London. Their remarks were part of an editorial accompanying the report (Blood 2015 Aug 27. doi:10.1182/blood-2015-07-655233). The authors had no disclosures to report.
Exosomes released by chronic lymphocytic leukemia (CLL) cells induce stromal cells to adopt a cancer-associated fibroblast phenotype, thereby creating a microenvironment conducive to CLL cell adhesion, survival, and growth.
Although the role of exosomes in other cancers has been well studied, their role in hematologic malignancies has not been well characterized. Also, this study confirmed that exosomes are present in CLL lymph nodes and promote tumor growth in vivo.
“Our in vitro and in vivo data show that CLL exosomes harbor an oncogenic potential by stimulating stromal cells to induce an inflammatory and protumorigenic milieu, including increased angiogenesis, thus supporting the survival and outgrowth of CLL cells,” wrote Jerome Paggetti, Ph.D., of the laboratory of experimental hemato-oncology, Luxembourg Institute of Health (Blood 2015 Aug 27. doi:10.1182/blood-2014-12-618025).
Cells were obtained from 21 CLL patients; all patients had an absolute lymphocyte count of more than 30,000/mcL and were untreated for 3 months. The researchers established 30-day cocultures of bone marrow mesenchymal stem cells with primary CLL cells in culture inserts or they treated bone marrow mesenchymal stem cells weekly with exosomes. Similar experiments were performed with the Burkitt lymphoma cell line Namalwa to investigate whether the impact on stromal cells is CLL specific.
Based on gene expression analysis, CLL exosomes and CLL cells cocultured in inserts induced similar gene expression changes in bone marrow mesenchymal stem cells, highlighting the relevance of exosomes for microenvironment changes. “Importantly, lymphoma cells induced a distinct gene expression pattern in bone marrow mesenchymal stem cells, suggesting a specific response to CLL exosomes,” wrote Dr. Paggetti and coauthors.
The impact of CLL exosomes on tumor growth was studied in vivo by subcutaneously injecting cells with and without CLL exosomes into immunocompromised mice. Cells supplemented with exosomes resulted in an increased tumor size compared with tumor cells injected without additional exosomes. Also, the cells supplemented with exosomes accumulated in mice kidneys, confirming the renal involvement observed in CLL patients. “Our data demonstrate a protumorigenic effect of CLL-derived exosomes in vivo and their importance in the early onset of the disease when tumor cells impact the microenvironment to proliferate and promote angiogenesis,” the researchers concluded.
Exosomes released by chronic lymphocytic leukemia (CLL) cells induce stromal cells to adopt a cancer-associated fibroblast phenotype, thereby creating a microenvironment conducive to CLL cell adhesion, survival, and growth.
Although the role of exosomes in other cancers has been well studied, their role in hematologic malignancies has not been well characterized. Also, this study confirmed that exosomes are present in CLL lymph nodes and promote tumor growth in vivo.
“Our in vitro and in vivo data show that CLL exosomes harbor an oncogenic potential by stimulating stromal cells to induce an inflammatory and protumorigenic milieu, including increased angiogenesis, thus supporting the survival and outgrowth of CLL cells,” wrote Jerome Paggetti, Ph.D., of the laboratory of experimental hemato-oncology, Luxembourg Institute of Health (Blood 2015 Aug 27. doi:10.1182/blood-2014-12-618025).
Cells were obtained from 21 CLL patients; all patients had an absolute lymphocyte count of more than 30,000/mcL and were untreated for 3 months. The researchers established 30-day cocultures of bone marrow mesenchymal stem cells with primary CLL cells in culture inserts or they treated bone marrow mesenchymal stem cells weekly with exosomes. Similar experiments were performed with the Burkitt lymphoma cell line Namalwa to investigate whether the impact on stromal cells is CLL specific.
Based on gene expression analysis, CLL exosomes and CLL cells cocultured in inserts induced similar gene expression changes in bone marrow mesenchymal stem cells, highlighting the relevance of exosomes for microenvironment changes. “Importantly, lymphoma cells induced a distinct gene expression pattern in bone marrow mesenchymal stem cells, suggesting a specific response to CLL exosomes,” wrote Dr. Paggetti and coauthors.
The impact of CLL exosomes on tumor growth was studied in vivo by subcutaneously injecting cells with and without CLL exosomes into immunocompromised mice. Cells supplemented with exosomes resulted in an increased tumor size compared with tumor cells injected without additional exosomes. Also, the cells supplemented with exosomes accumulated in mice kidneys, confirming the renal involvement observed in CLL patients. “Our data demonstrate a protumorigenic effect of CLL-derived exosomes in vivo and their importance in the early onset of the disease when tumor cells impact the microenvironment to proliferate and promote angiogenesis,” the researchers concluded.
FROM BLOOD
Key clinical point: Exosomes derived from chronic lymphocytic leukemia (CLL) cells induce stromal cell transition to cancer-associated fibroblasts.
Major finding: CLL exosomes and CLL cells cocultured in inserts induced similar gene expression changes in bone marrow mesenchymal stem cells.
Data source: In vitro and in vivo studies that used cells obtained from 21 CLL patients.
Disclosures: Jerome Paggetti, Ph.D., and coauthors reported having no disclosures.