User login
Article Type
Changed
Mon, 11/07/2022 - 14:55
Display Headline
Comorbidities, Racial Disparities, and Geographic Differences in Asthma
References
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
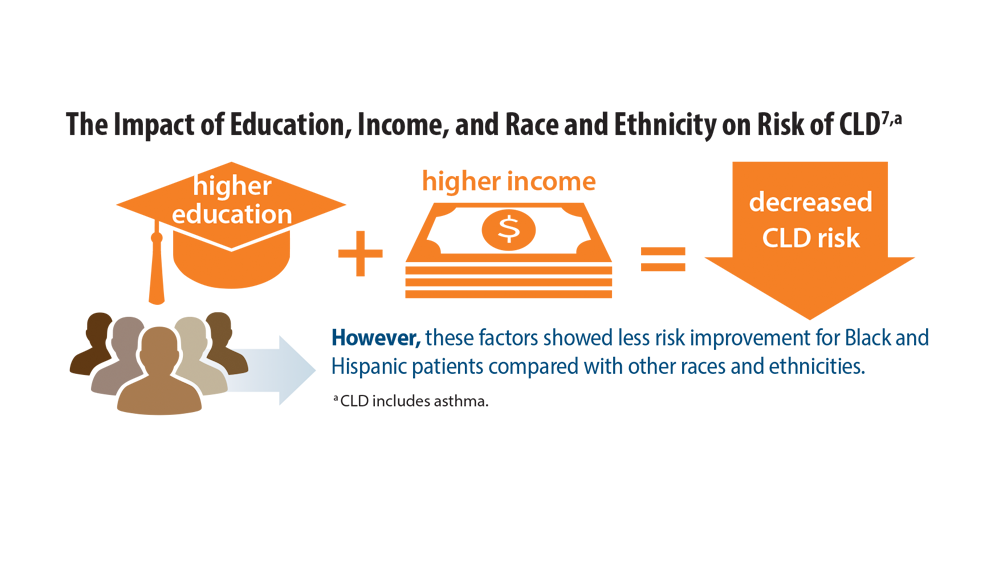
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
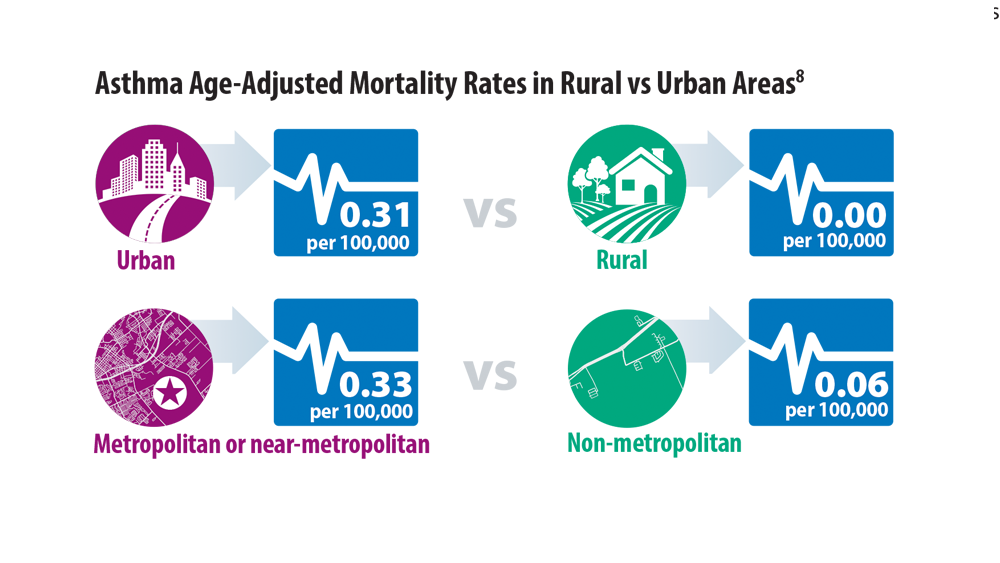
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025
Publications
Topics
References
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025
References
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025
Publications
Publications
Topics
Article Type
Display Headline
Comorbidities, Racial Disparities, and Geographic Differences in Asthma
Display Headline
Comorbidities, Racial Disparities, and Geographic Differences in Asthma
Disallow All Ads
Content Gating
No Gating (article Unlocked/Free)
Alternative CME
Disqus Comments
Default
Consolidated Pubs: Do Not Show Source Publication Logo
Use ProPublica
Conference Recap Checkbox
Not Conference Recap
Clinical Edge
Medscape Article
Display survey writer
Reuters content
Disable Inline Native ads
WebMD Article