User login
LOS ANGELES – The thickness and functional activation of primary somatosensory cortex mapping to the face differed according to the frequency of migraine in a small study presented at the annual meeting of the American Headache Society.
In the cross-sectional study of 20 patients, investigators conducted anatomic and functional magnetic resonance imaging in 10 patients with a low frequency of migraine attacks (mean age 40 years) and 10 with a high frequency of attacks (mean age 44 years).
Results showed that the area of the postcentral gyrus cortex representing the face was about a quarter thicker in the high-frequency group, compared with the low-frequency group. And activation of this area in response to a painful stimulus was also greater in the former.
"We think that this change that we see in high-frequency migraineurs is probably an adaptive response of the brain in order to accommodate this increased input of painful attacks, to be able to process it more and be able to handle it," commented lead investigator Nasim Maleki, Ph.D., of the Center for Pain and the Brain at Children’s Hospital Boston. Thus, the cortical thickening and increased activation might be a marker of chronification or transformation of migraine due to greater frequency of pain, triptan use, or both, she proposed.
A longitudinal study would be needed to definitively sort out cause versus effect, Dr. Maleki acknowledged. "But it could be a good hypothesis at least if somebody could do a longitudinal study, for example, looking at patients who regress from chronic to episodic migraine and then seeing if that area undergoes changes, both morphometric and functional changes."
Dr. Peter Goadsby of the University of California, San Francisco, asked, "Did you say that the BOLD [blood oxygen level–dependent] effect was being elicited from the dorsum of the hand, and the flow changes were in the face area [of the cortex]?"
"I was surprised by the same thing, too," Dr. Maleki replied. She noted that in results not shown, there was also activation of cortical areas corresponding to the hand. "But I think that maybe because that [face] area is already sensitized and responds to pain in general, the fact that we were seeing it even when we were stimulating the hand ... that’s relevant."
Session attendee Dr. Ronald Andiman of Cedars-Sinai Medical Center in Los Angeles asked, "What is the substance of the increased thickness of the cortex when you see it? Is it cellular? Is it neural fibers?"
It was not possible to tell given that the study used only MRI, Dr. Maleki said. "But ... we are thinking of doing the same thing in rats and seeing if there is the same pattern, and then we will be able to determine if it is density, or if it is just the number of neurons, or what exactly is going on," she said.
In a discussion of research highlights from the meeting and elsewhere, Dr. Stephen D. Silberstein of the Jefferson Headache Center in Philadelphia noted that a previous study of new London cab drivers found that their cortical thickness increased when they learned to navigate the city.
In the migraine study, "the question is, is this [thickening] cause or result?" he said. "I suspect this is like the cab drivers: If you have a lot of headaches, you learn what they are, and it affects your cortex. And I agree that this is probably a marker for migraine, not a cause of it."
Dr. Maleki and her colleagues recruited patients who had had episodic migraine for at least 3 years. On the basis of age, sex, and other migraine characteristics, they matched patients with low-frequency attacks (1-2 per month) to patients with high-frequency attacks (8-12 per month). However, she acknowledged, use of analgesic medications was unavoidably greater in the high-frequency group. The investigators also included a group of age- and sex-matched healthy individuals as controls.
Results from anatomical MRI showed that the thickness of the area of the postcentral gyrus representing the face averaged approximately 2.25 mm in patients with high-frequency migraines, compared with 1.75 mm in patients with low-frequency migraines (P less than .05) and 2.0 mm in the control participants (P less than .05).
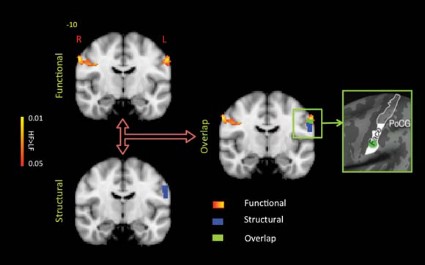
During functional MRI performed while a noxious heat stimulus was applied to the dorsum of the hand on the migraine-dominant side, there were greater increases in BOLD signals bilaterally in the same area in the high- versus low-frequency group. "Comparing what we saw in the morphometric differences between groups and these functional contrasting results, we saw an overlap between the area that shows this structural thickening and the area that shows this functional difference," Dr. Maleki noted.
Additional functional MRI comparing somatosensory cortex connectivity between migraine groups showed that certain other areas of the brain were also more active in the high-frequency group.
"Interestingly, all of these areas ... are known areas involved in pain processing," she noted. "So again, this confirms that this thicker cortical area in high-frequency migraineurs also has stronger communication with these other areas of the brain that are also involved in pain processing."
Dr. Maleki disclosed no relevant conflicts of interest. Data analysis was supported in part by a grant from Merck.
LOS ANGELES – The thickness and functional activation of primary somatosensory cortex mapping to the face differed according to the frequency of migraine in a small study presented at the annual meeting of the American Headache Society.
In the cross-sectional study of 20 patients, investigators conducted anatomic and functional magnetic resonance imaging in 10 patients with a low frequency of migraine attacks (mean age 40 years) and 10 with a high frequency of attacks (mean age 44 years).
Results showed that the area of the postcentral gyrus cortex representing the face was about a quarter thicker in the high-frequency group, compared with the low-frequency group. And activation of this area in response to a painful stimulus was also greater in the former.
"We think that this change that we see in high-frequency migraineurs is probably an adaptive response of the brain in order to accommodate this increased input of painful attacks, to be able to process it more and be able to handle it," commented lead investigator Nasim Maleki, Ph.D., of the Center for Pain and the Brain at Children’s Hospital Boston. Thus, the cortical thickening and increased activation might be a marker of chronification or transformation of migraine due to greater frequency of pain, triptan use, or both, she proposed.
A longitudinal study would be needed to definitively sort out cause versus effect, Dr. Maleki acknowledged. "But it could be a good hypothesis at least if somebody could do a longitudinal study, for example, looking at patients who regress from chronic to episodic migraine and then seeing if that area undergoes changes, both morphometric and functional changes."
Dr. Peter Goadsby of the University of California, San Francisco, asked, "Did you say that the BOLD [blood oxygen level–dependent] effect was being elicited from the dorsum of the hand, and the flow changes were in the face area [of the cortex]?"
"I was surprised by the same thing, too," Dr. Maleki replied. She noted that in results not shown, there was also activation of cortical areas corresponding to the hand. "But I think that maybe because that [face] area is already sensitized and responds to pain in general, the fact that we were seeing it even when we were stimulating the hand ... that’s relevant."
Session attendee Dr. Ronald Andiman of Cedars-Sinai Medical Center in Los Angeles asked, "What is the substance of the increased thickness of the cortex when you see it? Is it cellular? Is it neural fibers?"
It was not possible to tell given that the study used only MRI, Dr. Maleki said. "But ... we are thinking of doing the same thing in rats and seeing if there is the same pattern, and then we will be able to determine if it is density, or if it is just the number of neurons, or what exactly is going on," she said.
In a discussion of research highlights from the meeting and elsewhere, Dr. Stephen D. Silberstein of the Jefferson Headache Center in Philadelphia noted that a previous study of new London cab drivers found that their cortical thickness increased when they learned to navigate the city.
In the migraine study, "the question is, is this [thickening] cause or result?" he said. "I suspect this is like the cab drivers: If you have a lot of headaches, you learn what they are, and it affects your cortex. And I agree that this is probably a marker for migraine, not a cause of it."
Dr. Maleki and her colleagues recruited patients who had had episodic migraine for at least 3 years. On the basis of age, sex, and other migraine characteristics, they matched patients with low-frequency attacks (1-2 per month) to patients with high-frequency attacks (8-12 per month). However, she acknowledged, use of analgesic medications was unavoidably greater in the high-frequency group. The investigators also included a group of age- and sex-matched healthy individuals as controls.
Results from anatomical MRI showed that the thickness of the area of the postcentral gyrus representing the face averaged approximately 2.25 mm in patients with high-frequency migraines, compared with 1.75 mm in patients with low-frequency migraines (P less than .05) and 2.0 mm in the control participants (P less than .05).
During functional MRI performed while a noxious heat stimulus was applied to the dorsum of the hand on the migraine-dominant side, there were greater increases in BOLD signals bilaterally in the same area in the high- versus low-frequency group. "Comparing what we saw in the morphometric differences between groups and these functional contrasting results, we saw an overlap between the area that shows this structural thickening and the area that shows this functional difference," Dr. Maleki noted.
Additional functional MRI comparing somatosensory cortex connectivity between migraine groups showed that certain other areas of the brain were also more active in the high-frequency group.
"Interestingly, all of these areas ... are known areas involved in pain processing," she noted. "So again, this confirms that this thicker cortical area in high-frequency migraineurs also has stronger communication with these other areas of the brain that are also involved in pain processing."
Dr. Maleki disclosed no relevant conflicts of interest. Data analysis was supported in part by a grant from Merck.
LOS ANGELES – The thickness and functional activation of primary somatosensory cortex mapping to the face differed according to the frequency of migraine in a small study presented at the annual meeting of the American Headache Society.
In the cross-sectional study of 20 patients, investigators conducted anatomic and functional magnetic resonance imaging in 10 patients with a low frequency of migraine attacks (mean age 40 years) and 10 with a high frequency of attacks (mean age 44 years).
Results showed that the area of the postcentral gyrus cortex representing the face was about a quarter thicker in the high-frequency group, compared with the low-frequency group. And activation of this area in response to a painful stimulus was also greater in the former.
"We think that this change that we see in high-frequency migraineurs is probably an adaptive response of the brain in order to accommodate this increased input of painful attacks, to be able to process it more and be able to handle it," commented lead investigator Nasim Maleki, Ph.D., of the Center for Pain and the Brain at Children’s Hospital Boston. Thus, the cortical thickening and increased activation might be a marker of chronification or transformation of migraine due to greater frequency of pain, triptan use, or both, she proposed.
A longitudinal study would be needed to definitively sort out cause versus effect, Dr. Maleki acknowledged. "But it could be a good hypothesis at least if somebody could do a longitudinal study, for example, looking at patients who regress from chronic to episodic migraine and then seeing if that area undergoes changes, both morphometric and functional changes."
Dr. Peter Goadsby of the University of California, San Francisco, asked, "Did you say that the BOLD [blood oxygen level–dependent] effect was being elicited from the dorsum of the hand, and the flow changes were in the face area [of the cortex]?"
"I was surprised by the same thing, too," Dr. Maleki replied. She noted that in results not shown, there was also activation of cortical areas corresponding to the hand. "But I think that maybe because that [face] area is already sensitized and responds to pain in general, the fact that we were seeing it even when we were stimulating the hand ... that’s relevant."
Session attendee Dr. Ronald Andiman of Cedars-Sinai Medical Center in Los Angeles asked, "What is the substance of the increased thickness of the cortex when you see it? Is it cellular? Is it neural fibers?"
It was not possible to tell given that the study used only MRI, Dr. Maleki said. "But ... we are thinking of doing the same thing in rats and seeing if there is the same pattern, and then we will be able to determine if it is density, or if it is just the number of neurons, or what exactly is going on," she said.
In a discussion of research highlights from the meeting and elsewhere, Dr. Stephen D. Silberstein of the Jefferson Headache Center in Philadelphia noted that a previous study of new London cab drivers found that their cortical thickness increased when they learned to navigate the city.
In the migraine study, "the question is, is this [thickening] cause or result?" he said. "I suspect this is like the cab drivers: If you have a lot of headaches, you learn what they are, and it affects your cortex. And I agree that this is probably a marker for migraine, not a cause of it."
Dr. Maleki and her colleagues recruited patients who had had episodic migraine for at least 3 years. On the basis of age, sex, and other migraine characteristics, they matched patients with low-frequency attacks (1-2 per month) to patients with high-frequency attacks (8-12 per month). However, she acknowledged, use of analgesic medications was unavoidably greater in the high-frequency group. The investigators also included a group of age- and sex-matched healthy individuals as controls.
Results from anatomical MRI showed that the thickness of the area of the postcentral gyrus representing the face averaged approximately 2.25 mm in patients with high-frequency migraines, compared with 1.75 mm in patients with low-frequency migraines (P less than .05) and 2.0 mm in the control participants (P less than .05).
During functional MRI performed while a noxious heat stimulus was applied to the dorsum of the hand on the migraine-dominant side, there were greater increases in BOLD signals bilaterally in the same area in the high- versus low-frequency group. "Comparing what we saw in the morphometric differences between groups and these functional contrasting results, we saw an overlap between the area that shows this structural thickening and the area that shows this functional difference," Dr. Maleki noted.
Additional functional MRI comparing somatosensory cortex connectivity between migraine groups showed that certain other areas of the brain were also more active in the high-frequency group.
"Interestingly, all of these areas ... are known areas involved in pain processing," she noted. "So again, this confirms that this thicker cortical area in high-frequency migraineurs also has stronger communication with these other areas of the brain that are also involved in pain processing."
Dr. Maleki disclosed no relevant conflicts of interest. Data analysis was supported in part by a grant from Merck.
AT THE ANNUAL MEETING OF THE AMERICAN HEADACHE SOCIETY