User login
ANSWER
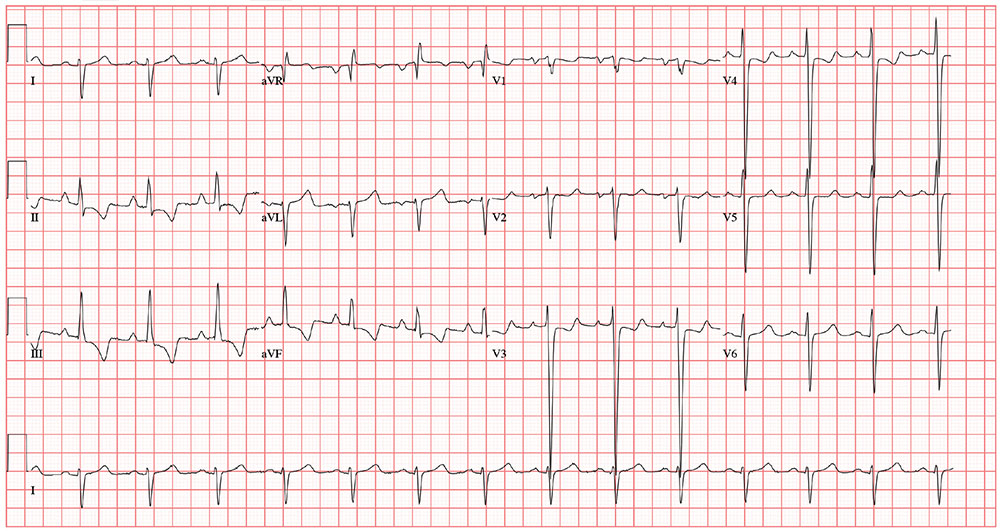
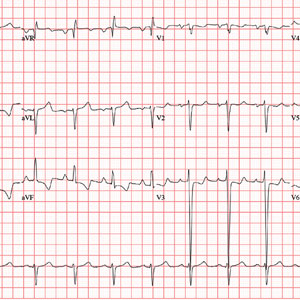
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
ANSWER
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
ANSWER
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
For the past 5 days, a 57-year-old man with “the flu” hasn’t been able to work. This morning, he awoke with chest tightness but denies chest pain. Because work has been busy lately, he just wants an antibiotic to help get him back on the job.
His primary symptom is a persistent, nonproductive cough that prevents him from getting a good night’s sleep. Associated symptoms include rhinorrhea, myalgias and arthralgias, and (for the first 3 days of illness) a low-grade fever. He’s been coughing so hard and for so long that his chest has begun to hurt. His cough is aggravated when lying down and somewhat relieved when sitting upright. He denies wheezing. He presents with specific requests: a chest x-ray to rule out pneumonia and prescriptions for azithromycin and codeine/acetaminophen (the latter for cough suppression).
Past medical history is remarkable for chronic obstructive pulmonary disease (COPD) and chronic bronchitis. Six months ago, a pulmonary function test revealed an FEV1 of 76% and an FEV1/FVC of 60%. He has chronic, mild to moderate shortness of breath with exertion. He has never had pneumonia or any anginal symptoms. Past surgical history is remarkable for an open reduction and internal fixation repair of his right tibia and an appendectomy. Current medications include acetaminophen for fever. He has used an albuterol inhaler in the past but has not had one for more than a year. He has no known drug allergies.
The patient is a crane operator for a large construction business. He is divorced and has an adult son with whom he has no contact. He’s been smoking 1.5 to 2 packs a day since he was 16. He used recreational marijuana until his employer began conducting random drug screenings 3 years ago. He drinks about 2 six-packs of beer a week—most of it on the weekends.
Family history is positive for COPD (mother), acute abdominal aortic dissection (father), and myocardial infarction (paternal grandfather).
The review of systems is positive for myalgias and arthralgias, which have been exacerbated by his recent illness. He denies a productive cough and any changes in heart rhythm and bowel or bladder function. He has no neurologic symptoms.
His vital signs include a blood pressure of 164/96 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 92% on room air; and temperature, 99.8°F.
Physical exam reveals an anxious, tired man in mild distress. His weight is 164 lb and his height, 70 in. The HEENT exam reveals ill-fitting corrective contact lenses, disheveled hair, and a nicotine-stained beard and mustache. His teeth are in poor repair; however, none are loose or missing. The neck is supple, and there is no thyromegaly. There is jugular venous distention, but not to the angle of the jaw. His respirations are shallow, requiring the use of accessory muscles. Deep inhalation causes uncontrollable coughing. Although there is anterior-posterior chest wall enlargement, it is insufficient to consider the patient barrel chested. Auscultation reveals diffuse, coarse rhonchi and end-expiratory wheezing.
The cardiac exam reveals a regular rate and rhythm of 80 beats/min, with a soft diastolic murmur (grade II/VI) that is best heard along the left sternal border. There are no extra heart sounds or rubs. The abdomen is tender to deep palpation in the right upper quadrant, with no evidence of rebound to suggest peritonitis. There are no abdominal or femoral arterial bruits. The extremities demonstrate 2+ pulses bilaterally with 1+ pitting edema in the lower legs. The neurologic exam is grossly intact.
The previously undocumented murmur prompts you to order an ECG. It shows a ventricular rate of 83 beats/min; PR interval, 178 ms; QRS duration, 110 ms; QT/QTc interval, 406/477 ms; P axis, 67°; R axis, 126°; and T axis, –57°. What is your interpretation of this ECG?