User login
Snow Way to Take Care of Your Heart
ANSWER
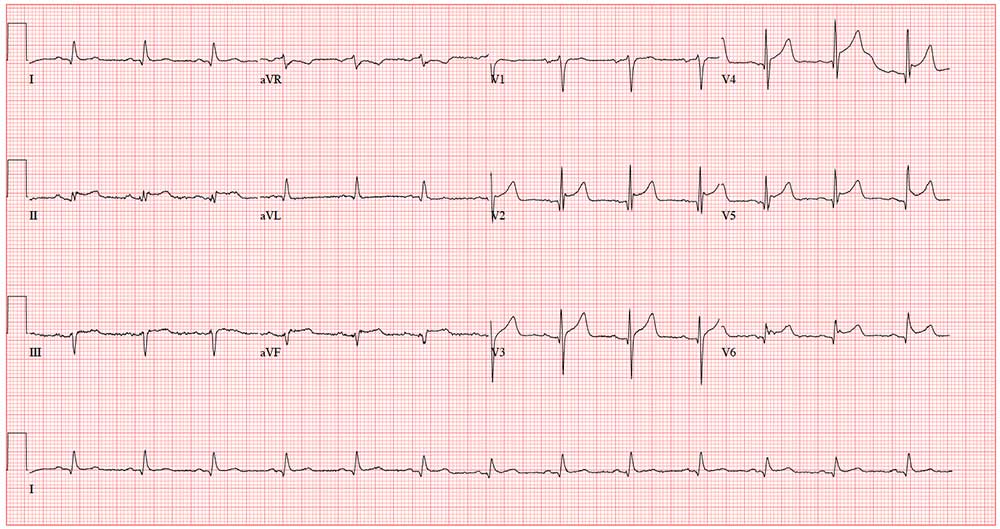
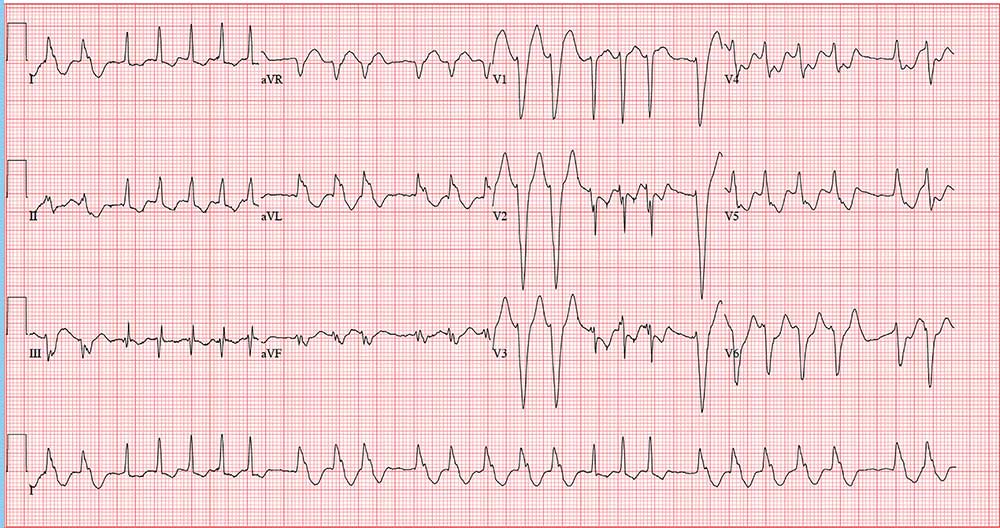
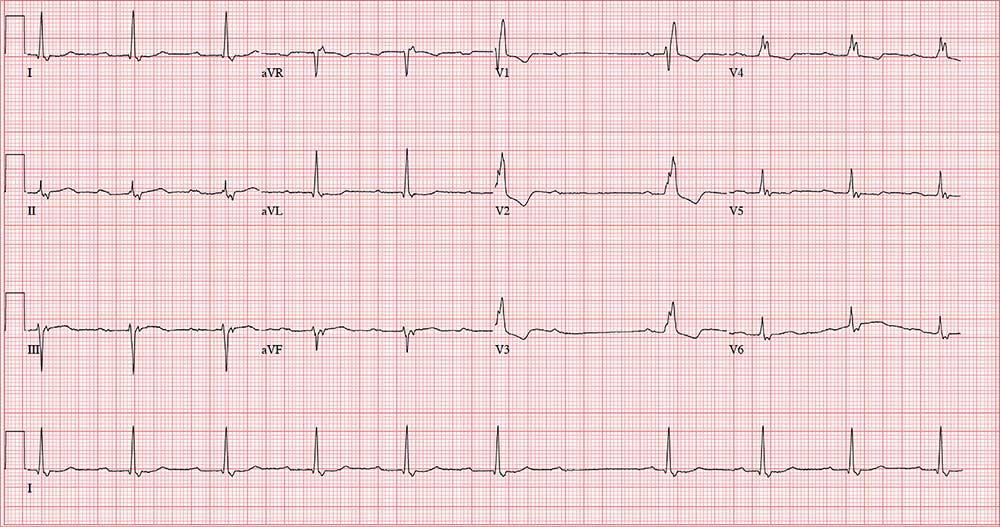
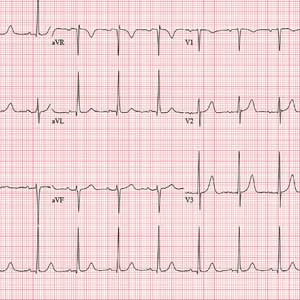
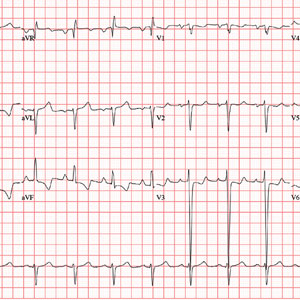
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
ANSWER
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
ANSWER
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
A 58-year-old man is snowmobiling with friends when he develops crushing substernal chest pain. He immediately stops his snowmobile and waves his arms for help—but by the time his friends reach him, he is lying on the ground, clutching his chest.
When asked what happened, he tells his friends that he’s been experiencing chest pain for the past hour but didn’t want to stop or interrupt their fun. He further reveals that he’s had chest “twinges” for the past 2 months, but they were always brief, and he didn’t think they were anything to be concerned about. He acknowledges that the current episode is “far worse” than what he previously experienced.
Because they are in the wilderness, no one in the group is able to establish cellphone service to call 911. The patient is loaded onto the back of another snowmobile for the 30-minute ride to the parking lot, where cellular service is accessible. They call 911, and an ACLS ambulance arrives about 50 minutes later.
An ECG is obtained in the field and transmitted to the receiving hospital, and the catherization lab is notified of an incoming patient. Transport to the hospital takes an hour; during the trip, the patient is administered oxygen, morphine, nitroglycerin, and an aspirin, and he is noted to have several nonsustained episodes of polymorphic ventricular tachycardia. The patient arrives at the hospital about 4 hours after onset of chest pain.
Medical history includes longstanding uncontrolled hypertension, recent onset of type 2 diabetes, and gastric reflux. He has never had shortness of breath, dyspnea on exertion, syncope, or near-syncope.
Current medications include lisinopril and metformin. However, the patient informs you that he hasn’t taken lisinopril in more than 3 months, and although he’s been given a prescription for metformin, he hasn’t filled it. He has no known drug allergies.
The patient is a mechanic at a local auto dealership. He smokes between 1 and 1.5 packs of cigarettes per day and has attempted to quit several times. He also consumes about 1 case of beer per week.
He is divorced, has no children, and lives alone. Both parents died in an automobile accident. The patient knows his father had several heart attacks beginning in his mid-50s and his mother “had thyroid problems.” His grandparents were known to have coronary artery disease and diabetes.
Review of systems is positive for a longstanding smoker’s cough and a healing burn on his right forearm, attributed to a welding injury.
His pretransport vital signs include a blood pressure of 178/88 mm Hg; pulse, 88 beats/min; respiratory rate, 18 breaths/min-1; and temperature, 97.6ºF. His stated weight is 265 lb and his height, 69 in.
Your findings on the physical exam corroborate those called in by the paramedics: an obese white male in obvious distress but alert and cooperative. His lungs reveal diffuse rales and crackles that clear with vigorous coughing. His cardiac exam reveals a regular rhythm at a rate of 80 beats/min with no murmurs or rubs. The abdomen is obese but otherwise normal. There is no peripheral edema. Pulses are strong and equal bilaterally. The neurologic exam is grossly intact. A bandaged second-degree burn is noted on the lower right forearm.
A repeat ECG shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation?
A New Valve—and a Change of Heart?
ANSWER
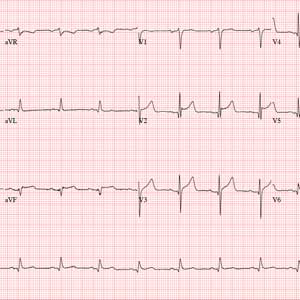
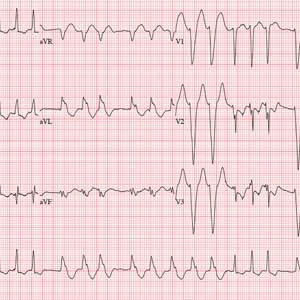
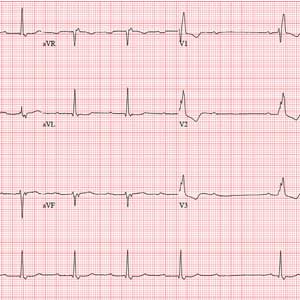
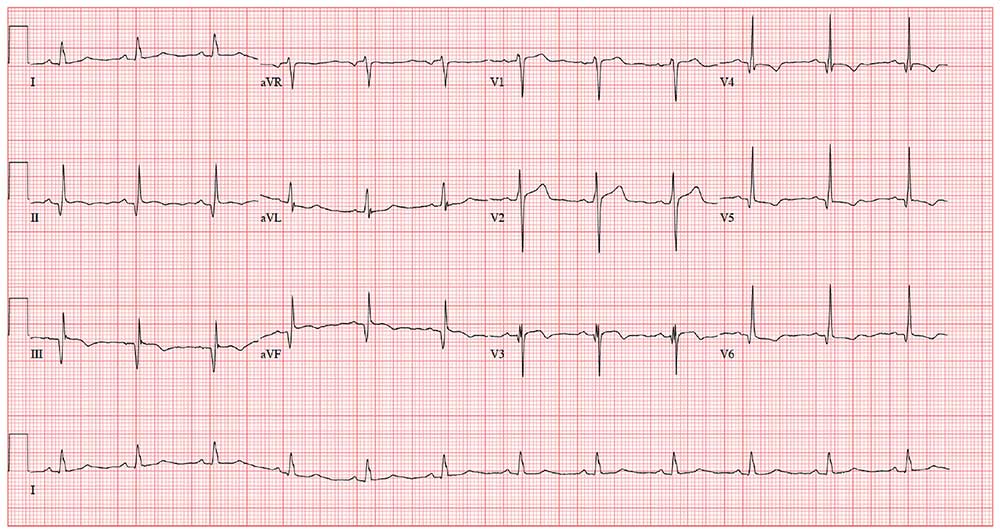
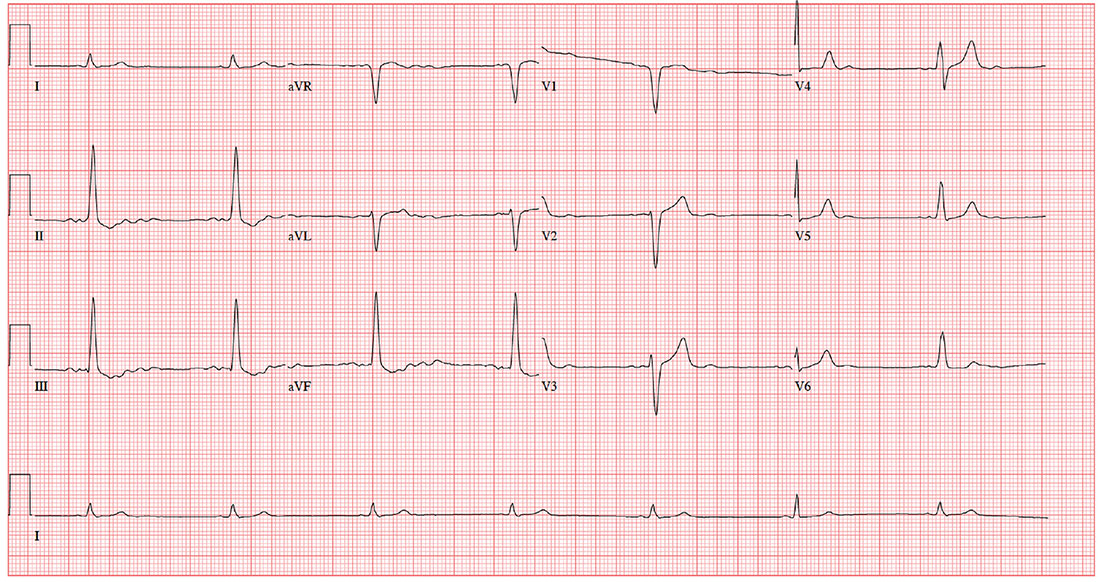
This ECG shows sinus rhythm with complete heart block and a junctional rhythm with a right-axis deviation. Additionally, ventricular depolarization in the precordial leads is suggestive of an anterior myocardial infarction.
Sinus rhythm is evidenced by the regular, steady progression of P waves with a P-P interval of about 90 beats/min. Complete atrioventricular dissociation indicates complete heart block.
A normal QRS duration of 106 ms at a rate of 56 beats/min supports the diagnosis of a junctional escape rhythm. Right-axis deviation is evidenced by an R axis of 120°.
Finally, poor R-wave progression with deep S waves in leads V1 through V5 is suggestive of an anterior myocardial infarction. However, in this case, there is no evidence of ischemia or history of infarction—so these are thought to be early postoperative findings.
ANSWER
This ECG shows sinus rhythm with complete heart block and a junctional rhythm with a right-axis deviation. Additionally, ventricular depolarization in the precordial leads is suggestive of an anterior myocardial infarction.
Sinus rhythm is evidenced by the regular, steady progression of P waves with a P-P interval of about 90 beats/min. Complete atrioventricular dissociation indicates complete heart block.
A normal QRS duration of 106 ms at a rate of 56 beats/min supports the diagnosis of a junctional escape rhythm. Right-axis deviation is evidenced by an R axis of 120°.
Finally, poor R-wave progression with deep S waves in leads V1 through V5 is suggestive of an anterior myocardial infarction. However, in this case, there is no evidence of ischemia or history of infarction—so these are thought to be early postoperative findings.
ANSWER
This ECG shows sinus rhythm with complete heart block and a junctional rhythm with a right-axis deviation. Additionally, ventricular depolarization in the precordial leads is suggestive of an anterior myocardial infarction.
Sinus rhythm is evidenced by the regular, steady progression of P waves with a P-P interval of about 90 beats/min. Complete atrioventricular dissociation indicates complete heart block.
A normal QRS duration of 106 ms at a rate of 56 beats/min supports the diagnosis of a junctional escape rhythm. Right-axis deviation is evidenced by an R axis of 120°.
Finally, poor R-wave progression with deep S waves in leads V1 through V5 is suggestive of an anterior myocardial infarction. However, in this case, there is no evidence of ischemia or history of infarction—so these are thought to be early postoperative findings.
Three days ago, a 64-year-old man underwent a tricuspid valve replacement for severe tricuspid regurgitation of unknown etiology. The surgical procedure included implantation of a 29-mm porcine valve and 2 epicardial right ventricular epicardial pacing leads.
The patient’s preoperative echocardiogram had shown severe tricuspid regurgitation with anterior leaflet prolapse and severe right atrial and ventricular enlargement. Preoperatively, the peak velocity of the tricuspid valve was 3.4 m/s, and the right ventricular systolic pressure was measured at 55 mm Hg. There was no mitral valvular disease or evidence of ischemia, and the overall left ventricular function was preserved, with a normal ejection fraction.
Preoperative history included 3-year progression of shortness of breath, dyspnea on exertion, and bilateral lower extremity edema. Over the past 2 months, he has had signs of hepatic congestion, including elevated serum transaminase, alkaline phosphatase, and direct bilirubin levels. A physical exam had revealed an enlarged liver that was tender to deep palpation. Social and family histories are noncontributory to the case as presented.
This morning, the patient is in no distress, sitting comfortably in a chair, and is alert and cooperative. Vital signs include a blood pressure of 118/64 mm Hg; pulse, 60 beats/min; respiratory rate, 16 breaths/min; and temperature, 96.4°F.
The surgical incision is clean, dry, and well approximated, and the patient is back to his preoperative weight. Pulmonary exam reveals clear breath sounds, with the exception of the left base, which demonstrates crackles that change with coughing. There are no wheezes. The cardiac exam reveals a regular rhythm at a rate of 60 beats/min, with a soft grade II/VI systolic murmur at the left lower sternal border. A late systolic friction rub is also evident. The abdomen is soft and nontender, with good bowel sounds and no organomegaly. Peripheral pulses are strong bilaterally, and there is trace pitting edema in both lower extremities. Neurologic exam is normal.
This morning’s ECG reveals a ventricular rate of 56 beats/min; PR interval, unmeasurable; QRS duration, 106 ms; QT/QTc interval, 400/386 ms; P axis, 36°; R axis, 120°; and T axis, 7°. What is your interpretation of this ECG?
Enough Fuss; She Wants Lunch!
ANSWER
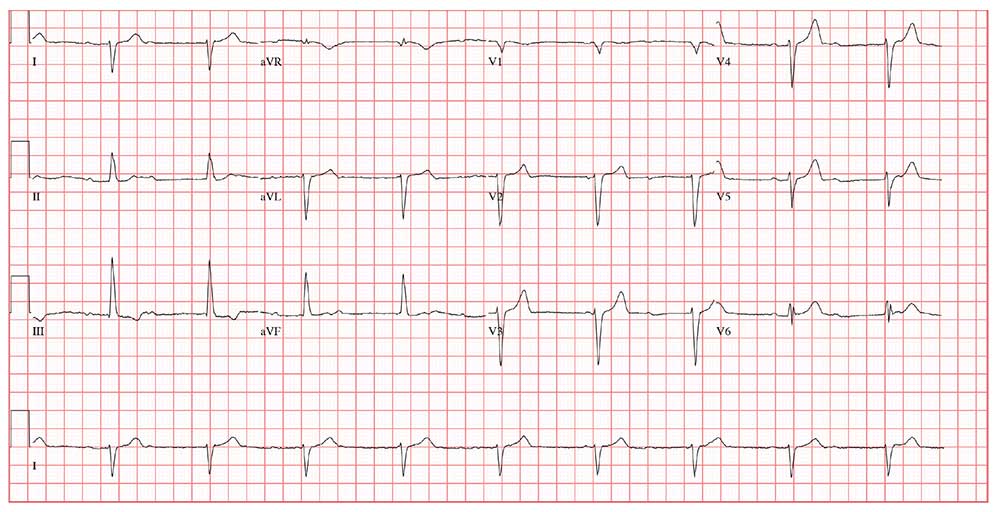
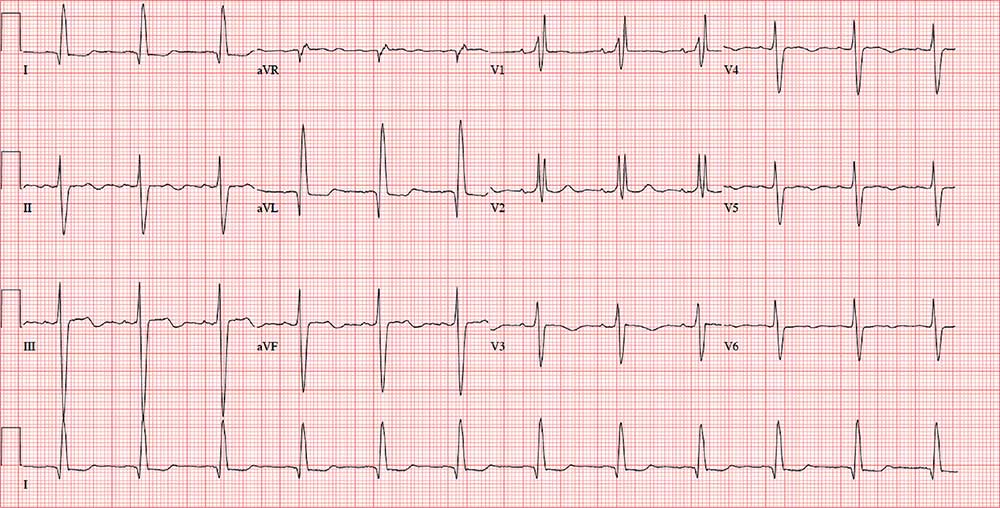
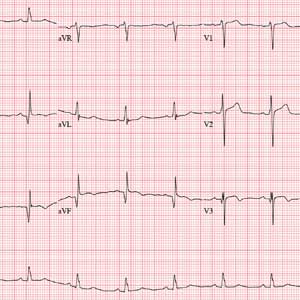
The correct interpretation is atrial fibrillation with aberrantly conducted complexes. The lead I rhythm strip at the bottom of the ECG shows the irregularly irregular rate. There are narrow complexes (see beats 3-7 and 16-18), indicating normal conduction through the atrioventricular node and His-Purkinje system. The remainder of the complexes are wide and aberrantly conducted and are in the same vector as the normally conducted (narrow) complexes.
An important take-away from this case
ANSWER
The correct interpretation is atrial fibrillation with aberrantly conducted complexes. The lead I rhythm strip at the bottom of the ECG shows the irregularly irregular rate. There are narrow complexes (see beats 3-7 and 16-18), indicating normal conduction through the atrioventricular node and His-Purkinje system. The remainder of the complexes are wide and aberrantly conducted and are in the same vector as the normally conducted (narrow) complexes.
An important take-away from this case
ANSWER
The correct interpretation is atrial fibrillation with aberrantly conducted complexes. The lead I rhythm strip at the bottom of the ECG shows the irregularly irregular rate. There are narrow complexes (see beats 3-7 and 16-18), indicating normal conduction through the atrioventricular node and His-Purkinje system. The remainder of the complexes are wide and aberrantly conducted and are in the same vector as the normally conducted (narrow) complexes.
An important take-away from this case
During morning rounds at a skilled nursing facility (SNF), a 74-year-old woman is found to have a rapid heart rate. She is placed on telemetry, which reveals a wide complex tachycardia. Concerned about possible ventricular tachycardia, the charge nurse contacts the on-call physician, who recommends calling 911. The patient is transferred via ACLS ambulance to your facility.
When you see her, she seems embarrassed by all the attention she’s receiving and expresses her desire to return to the SNF before she misses lunch. She is in no pain or discomfort, is not particularly short of breath, and does not feel dizzy or lightheaded. According to reports, she was friendly and conversive with both the nursing staff at the SNF and the paramedics during transport.
History is remarkable for several transient ischemic attacks with no residual sequelae, hypertension (under good control), and hypothyroidism (treatedwith medication). Surgical history includes a hyster-ectomy, a cholecystectomy, and an open reduction and metal plate fixation of a high (right) ankle break—all of which were performed more than 10 years ago.
Her medications include warfarin, hydrochlorothiazide, atorvastatin, and levothyroxine. She has no known drug allergies.
The patient is a retired junior high school principal. Her husband died of lung cancer 4 years ago. She has 3 adult children who are all in good health. She has never smoked but does enjoy a daily nightcap. She denies alcohol abuse or illicit drug use.
Family history reveals her parents died in a train accident and her paternal grandparents died of tuberculosis. She does not know her maternal grandparents’ medical history.
Review of systems is positive for chronic constipation and chronic hip and knee discomfort. Vital signs include a blood pressure of 124/88 mm Hg; pulse, 140 beats/min; respiratory rate, 14 breaths/min; and temperature, 97.6°F. Her weight is 158 lb, and her height is not measured.
Physical exam reveals a pleasant elderly woman in no distress. She is dressed appropriately, her hair is styled, and she is wearing makeup as she usually does. The HEENT exam reveals hearing aids and corrective lenses. Her neck has no jugular venous distention, carotid bruits, or thyromegaly.
Her lungs are clear in all fields. Her heart has a rapid and questionably irregular rhythm. There are no appreciable murmurs or rubs. Her abdominal exam is normal, with the exception of well-healed surgical scars. There is no peripheral edema, and all pulses are equal bilaterally in both upper and lower extremities. The neurologic exam is grossly normal with normal affect and mood.
An ECG reveals a ventricular rate of 152 beats/min; PR interval, 128 ms; QRS duration, 88 ms; QT/QTc interval, 280/445 ms; P axis, 27°; R axis, 23°; and T axis, 232°. What is your interpretation?
His Heart’s Awkward Timing
ANSWER
The correct answer is atrial flutter with 2:1 atrioventricular (AV) conduction. The QRS complexes are narrow and regular, indicating the rhythm originates within the atria or AV node, with conduction down the normal His-Purkinje system, and not from the ventricles.
The regular rate of the P waves and QRS complexes rules out atrial fibrillation with a rapid ventricular response. If you look carefully, you’ll see a P wave immediately before each QRS complex, and you’ll also see a P wave at the onset of the T wave (best seen in leads II, V3, and V6) resulting in what looks like a notched T wave. If you measure the duration of the P at the onset of the T wave to the P wave prior to the QRS complex, you’ll see the intervals are regular and march through the QRS complexes.
With 2 P waves for every QRS complex, the atria are contracting at 310 beats/min (193 ms), a rate consistent with atrial flutter in a 2:1 conduction pattern, compared to the ventricular rate of 155 beats/min (387 ms).
ANSWER
The correct answer is atrial flutter with 2:1 atrioventricular (AV) conduction. The QRS complexes are narrow and regular, indicating the rhythm originates within the atria or AV node, with conduction down the normal His-Purkinje system, and not from the ventricles.
The regular rate of the P waves and QRS complexes rules out atrial fibrillation with a rapid ventricular response. If you look carefully, you’ll see a P wave immediately before each QRS complex, and you’ll also see a P wave at the onset of the T wave (best seen in leads II, V3, and V6) resulting in what looks like a notched T wave. If you measure the duration of the P at the onset of the T wave to the P wave prior to the QRS complex, you’ll see the intervals are regular and march through the QRS complexes.
With 2 P waves for every QRS complex, the atria are contracting at 310 beats/min (193 ms), a rate consistent with atrial flutter in a 2:1 conduction pattern, compared to the ventricular rate of 155 beats/min (387 ms).
ANSWER
The correct answer is atrial flutter with 2:1 atrioventricular (AV) conduction. The QRS complexes are narrow and regular, indicating the rhythm originates within the atria or AV node, with conduction down the normal His-Purkinje system, and not from the ventricles.
The regular rate of the P waves and QRS complexes rules out atrial fibrillation with a rapid ventricular response. If you look carefully, you’ll see a P wave immediately before each QRS complex, and you’ll also see a P wave at the onset of the T wave (best seen in leads II, V3, and V6) resulting in what looks like a notched T wave. If you measure the duration of the P at the onset of the T wave to the P wave prior to the QRS complex, you’ll see the intervals are regular and march through the QRS complexes.
With 2 P waves for every QRS complex, the atria are contracting at 310 beats/min (193 ms), a rate consistent with atrial flutter in a 2:1 conduction pattern, compared to the ventricular rate of 155 beats/min (387 ms).
Approximately 5
Feeling fine, he went about his normal workday—but in the afternoon, while sitting at his desk, his rapid heart rate returned. He called over a coworker, who observed that he was “pale” and “sweaty.” His pulse was 130 beats/min. After “a few minutes,” the rapid heart rate spontaneously terminated, and he decided to take off the rest of the day.
This morning, he again awoke with a rapid heart rate and lightheadedness—but he also felt like the room was spinning. At that point, he called 911. By the time the paramedics arrived, his rapid heart rate had spontaneously terminated. Understandably concerned, however, he requested transport to your facility.
The patient says he is in normal health, with no prior cardiac history. He denies any chest pain, dyspnea, shortness of breath, nausea, vomiting, syncope, or near-syncope associated with his recent episodes.
Medical history is remarkable for hypertension, hyperlipidemia, and type 2 diabetes. He has had no surgical procedures. His medications include aspirin, lisinopril, and lovastatin; he says he takes his medications as prescribed and there have been no recent changes to the drugs or dosages. He has no known drug allergies.
Family history includes myocardial infarction in both parents; they are alive and well. The patient’s younger brother has Wolff-Parkinson-White syndrome and underwent an ablation at age 24.
The patient is a practicing attorney for a local firm. He is married with 2 children. He has no history of alcohol, tobacco, or illicit drug use.
Review of systems is positive for a 10-lb weight gain over the past 6 months and new-onset nocturia.
During the physical exam, the patient informs you that his heart is racing again. The exam is suspended, and a 12-lead ECG is quickly performed. It shows a ventricular rate of 155 beats/min; no measurable PR interval; QRS duration, 78 ms; QT/QTc interval, 272/437 ms; P axis, unmeasurable; R axis, 34°; and T axis, –50°.
The physical exam is completed after the tachycardia spontaneously terminates. The patient’s blood pressure is 148/88 mm Hg; pulse, 94 beats/min and regular; respiratory rate, 18 breaths/min-1; and temperature, 97.9°F. He appears frightened but otherwise healthy. Pertinent findings of the physical exam include a normal fundoscopic examination with sharp disc margins, clear breath sounds bilaterally, normal heart sounds with no murmur or rub, a soft abdomen with no palpable masses, strong and equal pulses bilaterally in both upper and lower extremities, and a normal neurologic exam with no cognitive deficits.
Now that the physical exam is complete, what is your interpretation of this ECG?
Staying Awake to Evade Death
ANSWER
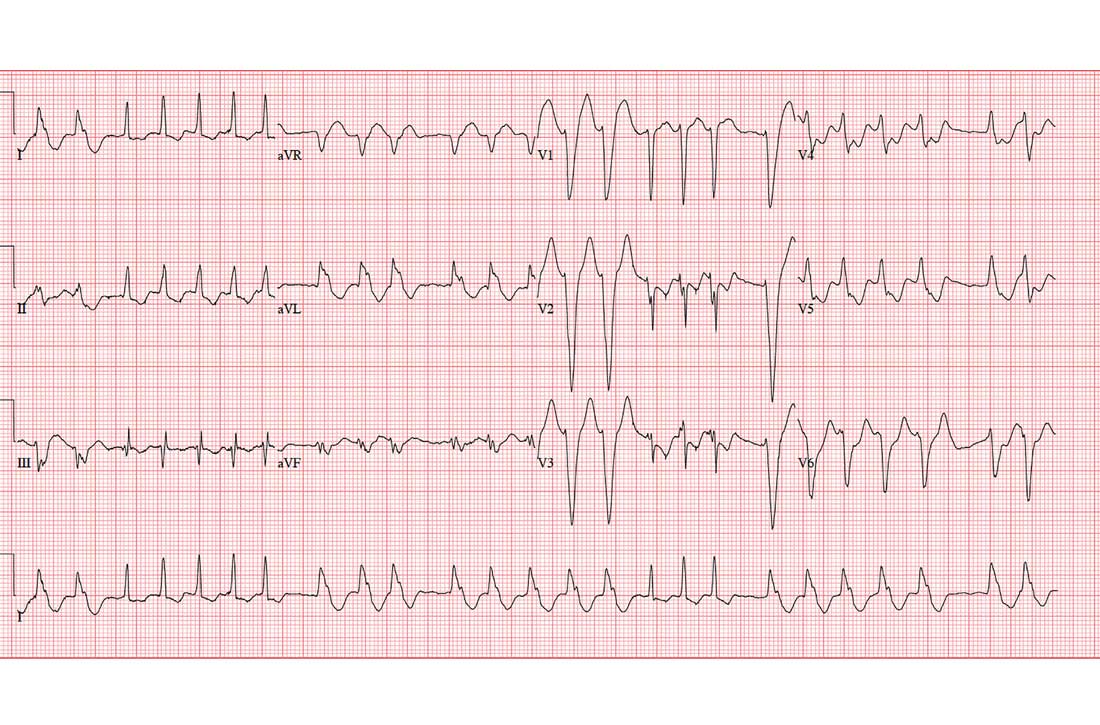
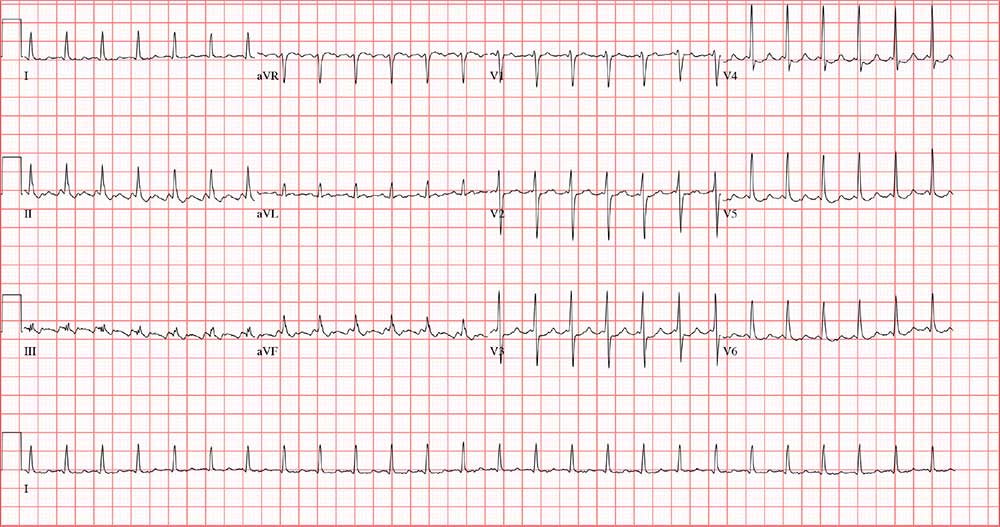
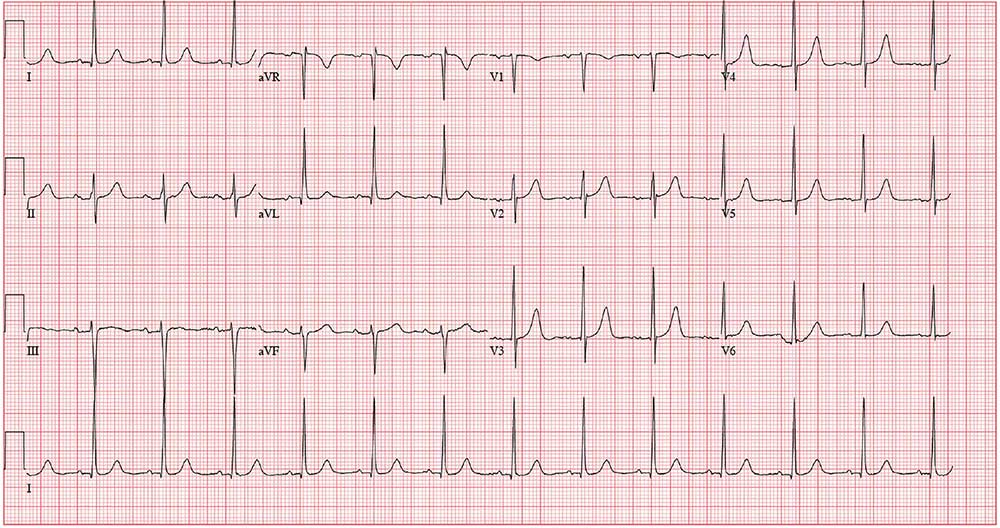
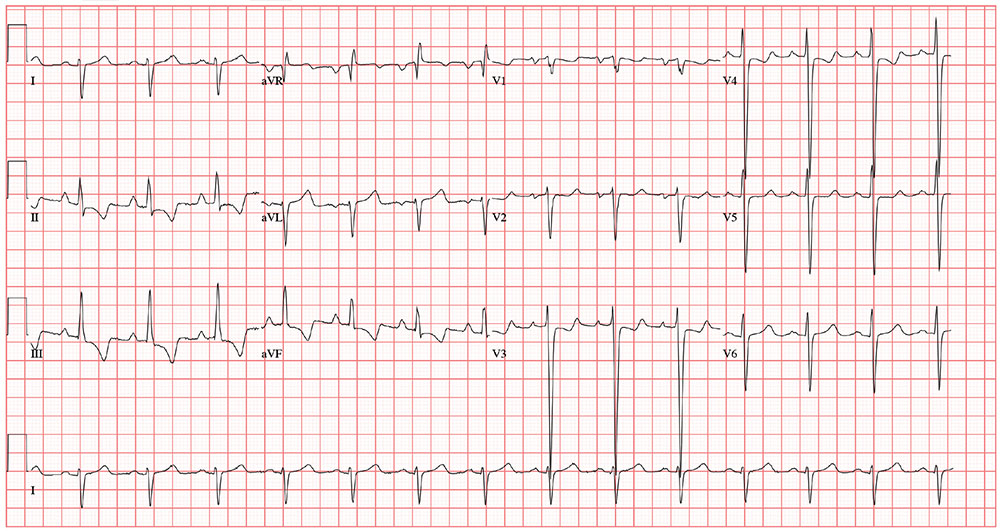
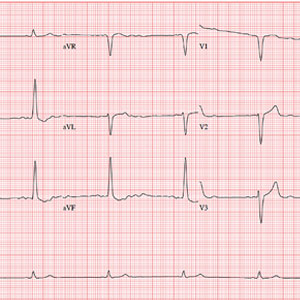
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
ANSWER
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
ANSWER
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
A 64-year-old man presents with a 6-month history of skipped heart beats. He says this occurs most often in the evenings, when he’s resting, and he has been awakened by it. He denies chest pain, dyspnea with exertion, syncope, or near-syncope. He has been otherwise asymptomatic from a cardiac and pulmonary standpoint.
However, he is increasingly concerned that his heart may “just stop beating” when he is asleep. When pressed further, he reveals he is afraid to go to sleep at night, knowing “my heart will start skipping beats and I’ll die!” He has discussed his fear of dying in his sleep with a psychologist, who told him that although he experiences fatigue and loss of energy and has recurrent thoughts of death, he does not meet DSM-5 criteria for major depressive disorder. The psychologist obtained an ECG and noticed pauses, which prompted referral of the patient to you.
Past medical history is remarkable for hypertension, cirrhosis, and osteoarthritis. Surgical history includes bilateral knee and left hip replacements. A screening colonoscopy 1 month ago yielded a diagnosis of stage 1 colorectal cancer.
The patient’s medication list includes hydrochlorothiazide and celecoxib. He is allergic to oxycodone (anaphylaxis).
The patient is divorced, which he attributes to his ongoing alcoholism. He drinks half a bottle of whiskey daily to “help with my nerves” and “get drunk enough to sleep.” He reports a lifetime of heavy drinking; he has tried Alcoholics Anonymous but kept dropping out to drink. He also smokes up to 1.5 packs/d of cigarettes. He has no children. He worked as a machinist in a factory but was laid off a year ago when the company downsized.
Family history is positive for alcoholism (father, 2 brothers) and hypothyroidism (mother).
Review of systems is positive for a chronic smoker’s cough, lower abdominal cramping following his colonoscopy, and arthritic pain in his wrists and ankles.
Vital signs include a blood pressure of 174/92 mm Hg; pulse, 74 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 97% on room air. His weight is 247 lb and his height, 69 in. His BMI is 36.5.
Physical exam reveals a somewhat disheveled male in no apparent distress. He wears corrective lenses and has tobacco stains on his mustache. His HEENT exam is surprisingly normal, and there is no evidence of rhinophyma. There is no jugular venous distention, thyromegaly, or lymphadenopathy. There are crackles and late expiratory wheezes in both lower lung fields.
The cardiac exam reveals a regular rate and rhythm of 74 beats/min, with no murmurs, rubs, or extra heart sounds. Peripheral pulses are strong and equal bilaterally. The abdomen is obese but nontender, and there are no palpable masses. There are surgical scars over both knees and the left hip. Arthritic changes are noticeable in the fingers on both hands. There are no neurologic deficits.
Through the electronic medical record, you access the ECG taken in the psychologist’s office. It shows a ventricular rate of 56 beats/min; no measurable PR interval; QRS duration, 144 ms; QT/QTc interval, 438/422 ms; P axis, 47°; R axis, –24°; and T axis, 55°. What is your interpretation of this ECG?
Follow Where She Leads
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
For several years, a 75-year-old woman has been followed for aortic stenosis. Historically, she has done well—but about a year ago, she began experiencing shortness of breath. Within the past 2 months, she has had significantly increasing dyspnea with minimal activity and has experienced 2 episodes of near-syncope. This morning, she complains of chest tightness.
Her medical history is remarkable for hypertension, rheumatoid arthritis, and coronary artery disease. Two years ago, catheterization for chest pain revealed stenoses of her left anterior descending artery (LAD), a diagonal branch of the LAD, and an occluded right coronary artery. A drug-eluding stent was placed, and she has had no symptoms since. She also has a history of paroxysmal atrial fibrillation but has had no episodes in the past year.
An echocardiogram performed 1 week ago revealed severe aortic valve stenosis with a trileaflet valve with heavily calcified leaflets; an aortic valve gradient of 0.4 cm2, with a peak velocity of 5 m/s and a mean gradient of 61 mm Hg; and mild aortic regurgitation. It also showed an enlarged left atrium and mild-to-moderate mitral regurgitation.
Her current medications include senna glycoside, prednisone, metoprolol, atorvastatin, and apixaban. She has a true anaphylactic allergy to penicillin.
The patient, a retired administrative assistant, was widowed 4 years ago, when her husband died as a result of an automobile accident. They had no children. She has never smoked but reports having 1 to 2 glasses of wine each night.
Review of symptoms is positive for joint pain, particularly in her hands, hips, and knees. It is worse in the morning and improves as the day progresses. She tried NSAIDs but experienced bleeding, so she was recently started on prednisone. She also has chronic constipation, for which she takes senna with reasonable results. She denies any significant constitutional, respiratory, urologic, or neurologic symptoms.
Vital signs include a blood pressure of 146/86 mm Hg; pulse, 70 beats/min; respiratory rate, 14 breaths/min-1; temperature, 97.6°F; and O2 saturation, 96% on room air. Her weight is 139 lb and her height, 5 ft 5 in; her BMI is 23.1.
Physical exam reveals corrective lenses and bilateral hearing aids. The patient has multiple bruises of varying stages on both upper extremities. Her teeth are in good repair. There is no significant jugular venous distention or thyromegaly. The lungs are clear in all fields.
The cardiac exam is remarkable for a regular rate and rhythm, with a grade III/VI crescendo-decrescendo systolic murmur best heard at the right upper sternal border. She also has a grade II/VI late systolic murmur at the apex in the left lateral decubitus position. The A2 component of the second heart sound is absent, and there are no gallops or rubs.
The abdominal exam is normal, without palpable masses. Her peripheral pulses are strong and equal bilaterally. She has arthritic changes in her hands bilaterally and has no focal neurologic symptoms.
Her ECG reveals a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation?
Don’t Worry, It’s Just a Valve Problem
ANSWER
The correct interpretation includes normal sinus rhythm, possible left atrial enlargement (LAE), and left ventricular hypertrophy (LVH).
Normal sinus rhythm is defined as a P for every QRS and a QRS for every P, with a normal PR interval and a rate > 60 and < 100 beats/min.
Criteria for LAE include a P wave > 120 ms in lead II and/or a biphasic P wave in lead V1 with a downward deflection > 40 ms in length with a > 1-mm negative deflection. This ECG does not meet criteria for LAE; however, it is suspicious, particularly in the context of mitral regurgitation and LVH.
LVH is diagnosed using either the Sokolow-Lyon criteria (the sum of the S wave in V1 and the R wave in V5 or V6 ≥ 35 mm) or the Cornell voltage criteria (the S in V3 plus the R in aVL > 20 mm for women [> 28 mm for men]).
LVH is usually not a target of therapy. Management is typically directed at treating the underlying pathology. For this patient, it is important to manage her hypertension and provide follow-up—including periodic echocardiography of her left atrium, mitral valve, and left ventricle—to determine response to hypertensive therapy.
ANSWER
The correct interpretation includes normal sinus rhythm, possible left atrial enlargement (LAE), and left ventricular hypertrophy (LVH).
Normal sinus rhythm is defined as a P for every QRS and a QRS for every P, with a normal PR interval and a rate > 60 and < 100 beats/min.
Criteria for LAE include a P wave > 120 ms in lead II and/or a biphasic P wave in lead V1 with a downward deflection > 40 ms in length with a > 1-mm negative deflection. This ECG does not meet criteria for LAE; however, it is suspicious, particularly in the context of mitral regurgitation and LVH.
LVH is diagnosed using either the Sokolow-Lyon criteria (the sum of the S wave in V1 and the R wave in V5 or V6 ≥ 35 mm) or the Cornell voltage criteria (the S in V3 plus the R in aVL > 20 mm for women [> 28 mm for men]).
LVH is usually not a target of therapy. Management is typically directed at treating the underlying pathology. For this patient, it is important to manage her hypertension and provide follow-up—including periodic echocardiography of her left atrium, mitral valve, and left ventricle—to determine response to hypertensive therapy.
ANSWER
The correct interpretation includes normal sinus rhythm, possible left atrial enlargement (LAE), and left ventricular hypertrophy (LVH).
Normal sinus rhythm is defined as a P for every QRS and a QRS for every P, with a normal PR interval and a rate > 60 and < 100 beats/min.
Criteria for LAE include a P wave > 120 ms in lead II and/or a biphasic P wave in lead V1 with a downward deflection > 40 ms in length with a > 1-mm negative deflection. This ECG does not meet criteria for LAE; however, it is suspicious, particularly in the context of mitral regurgitation and LVH.
LVH is diagnosed using either the Sokolow-Lyon criteria (the sum of the S wave in V1 and the R wave in V5 or V6 ≥ 35 mm) or the Cornell voltage criteria (the S in V3 plus the R in aVL > 20 mm for women [> 28 mm for men]).
LVH is usually not a target of therapy. Management is typically directed at treating the underlying pathology. For this patient, it is important to manage her hypertension and provide follow-up—including periodic echocardiography of her left atrium, mitral valve, and left ventricle—to determine response to hypertensive therapy.
A 49-year-old woman establishes care at your clinic after moving to the area. When asked about previous health care provision, she reports being followed for a “valve problem” and high blood pressure—although she admits she hasn’t kept many of her scheduled appointments. Two past echocardiograms documented valvular heart disease, although she can’t remember which valve. She was told it was nothing to worry about but that she should have follow-up. She also says she’s been prescribed medication to help with her hypertension but in the past 6 months hasn’t taken any because she’s been “too busy” to get the script filled.
She denies a history of chest pain or dyspn
Medical history is remarkable for resection of 2 lipomas on her left arm and leg. She has had 2 uncomplicated pregnancies and 1 in which she had preeclampsia. All 3 deliveries were Cesarean. She is currently taking no medications and has no known drug allergies.
Family history is remarkable for hypothyroidism and type 2 diabetes (in her mother). When the patient was 4, her mother remarried, so she does not know her biological father’s health history. She has 2 sons and 1 daughter who are in good health.
Divorced for 7 years, the patient is not currently in a relationship. She is a project manager for a start-up software company where she works long, stressful hours and drinks “a lot” of coffee. She does not drink alcohol or smoke.
The review of systems is consistent with premenopausal symptoms including hot flashes, night sweats, and irregular menses. She has no gastrointestinal or urinary symptoms. She has had no recent weight loss or gain.
Vital signs include a blood pressure of 168/98 mm Hg; pulse, 80 beats/min; respiratory rate, 12 breaths/min-1; O2 saturation, 96% on room air; and temperature, 98.2°F. Her height is 64 in and her weight, 164 lb.
Physical exam reveals a pleasant, well-kept woman in no distress. She wears contact lenses and has no oropharyngeal lesions. Her teeth are capped with porcelain. There is no thyromegaly, jugular venous distention, or carotid bruits. The lungs are clear in all lung fields. The cardiac exam is remarkable for a regular rate and rhythm of 80 beats/min, with a mid-to-late systolic murmur best heard when the patient is in the left lateral decubitus position. She has no extra heart sounds or rubs.
The abdomen is soft and nontender, with a well-healed Pfannenstiel surgical scar. The extremities have full range of motion with no peripheral edema. She has a recent full-sleeve tattoo on her right arm, which is well healed with no erythema. The neurologic exam is grossly intact.
As part of her workup, you order an ECG. It reveals a ventricular rate of 79 beats/min; PR interval, 184 ms; QRS duration, 76 ms; QT/QTc interval, 382/438 ms; P axis, 48°; R axis, –29°; and T axis, 33°. What is your interpretation of this ECG?
Hanging by a Thread
ANSWER
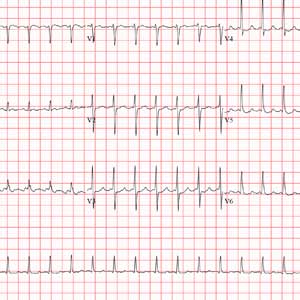
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
ANSWER
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
ANSWER
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
A 54-year-old man presents for preoperative workup for surgical repair of a partial tear of his right rotator cuff. He sustained the injury about 8 months ago, while rock climbing. His clinical work-up included MRI, magnetic resonance arthrogram, and dynamic musculoskeletal ultrasound. Initial treatment included physical therapy and 2 corticosteroid injections, without relief. A repeat arthrogram showed no resolution of the tear and revealed tendon retraction and muscular atrophy. The patient declined further physical therapy and opted for surgical intervention instead, because the injury is in his dominant shoulder and the pain continues to interfere with his job as a general contractor.
His medical history is positive for hypertension and hypercholesterolemia, which have been managed with medications. There is also a history of myocardial infarction (MI), which occurred 3 years ago when he was lifting a heavy truss at a job site; it manifested as acute chest pain, shortness of breath, and diaphoresis. He waited 3 days before seeking medical care because he “needed to get that project done.” He has had no further chest pain, but he‘s felt “a twinge” now and again in the past 2 months. He denies shortness of breath, dyspnea on exertion, or exertional chest pain. He has had no palpitations, syncope, or near-syncope.
His current medications include diltiazem, atorvastatin, and isosorbide. He tried metoprolol but did not like how he felt when taking it. He has no known drug allergies.
Family history is positive for familial hyperlipidemia on his father’s side. His father died of a heart attack at age 51. His mother has type 2 diabetes mellitus. His 2 older brothers have had MIs; his younger sister has no known health issues.
The patient is a self-employed general contractor. He has been married for 20 years and has a 21-year-old son who works for him. He smokes 1 to 1.5 packs a day and takes a shot of bourbon every night before dinner.
A review of systems reveals an 8-lb weight gain over the past 6 months. He denies fever, chills, and gastrointestinal and urologic symptoms. He believes he is depressed because his rotator cuff injury prevents him from doing what he would like.
Vital signs include a blood pressure of 138/88 mm Hg; pulse, 72 beats/min; respiratory rate, 14 breaths/min; O2 saturation, 98% on room air; and temperature, 97.4°F. His height is 70 in and his weight, 208 lb.
Physical exam reveals an anxious male in no distress wearing a sling on his right upper extremity. The HEENT exam is remarkable for corrective lenses. There are no lesions in the oropharynx, and his tobacco-stained teeth are in otherwise good repair. The neck is supple, and there are no carotid bruits, jugular venous distention, or thyromegaly. The pulmonary exam reveals coarse, scattered crackles with end-expiratory wheezing that clears with coughing.
Cardiac exam reveals a regular rate and rhythm of 72 beats/min. There are no murmurs, extra heart sounds, or rubs.
The abdomen is soft and nontender without palpable organomegaly or pulsatile masses. The lower extremities reveal no edema. The right upper extremity exam is deferred because the patient is very apprehensive about any movement of his shoulder. Peripheral pulses are strong and equal bilaterally. The neurologic exam is grossly intact.
As part of the preoperative workup, an ECG is ordered. It shows a ventricular rate of 72 beats/min; PR interval, 158 ms; QRS duration, 106 ms; QT/QTc interval, 400/438 ms; P axis, 33°; R axis, 38°; and T axis, –15°. What is your interpretation of this ECG?
Coughing Won’t Pay the Bills
ANSWER
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
ANSWER
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
ANSWER
The correct interpretation includes normal sinus rhythm, biatrial enlargement, and right-axis deviation. Other findings include a prolonged QT interval and ST-T wave abnormalities in inferior and anterior distributions.
A P wave
A normal QTc interval is generally 350 to 440 ms; the patient’s QTc interval (477 ms) meets the criteria for prolonged QT. There are ST- and T-wave inversions in leads II, III, and aVF, consistent with inferior ischemia, with ST depressions in leads V3 and V4, which could suggest anterior ischemia. Such findings are also seen in a pulmonary disease pattern.
Further workup included a chest x-ray, laboratory testing, and an echocardiogram. The last revealed right lower lobe consolidation and a diffuse, dilated cardiomyopathy with mild mitral and tricuspid regurgitation.
For the past 5 days, a 57-year-old man with “the flu” hasn’t been able to work. This morning, he awoke with chest tightness but denies chest pain. Because work has been busy lately, he just wants an antibiotic to help get him back on the job.
His primary symptom is a persistent, nonproductive cough that prevents him from getting a good night’s sleep. Associated symptoms include rhinorrhea, myalgias and arthralgias, and (for the first 3 days of illness) a low-grade fever. He’s been coughing so hard and for so long that his chest has begun to hurt. His cough is aggravated when lying down and somewhat relieved when sitting upright. He denies wheezing. He presents with specific requests: a chest x-ray to rule out pneumonia and prescriptions for azithromycin and codeine/acetaminophen (the latter for cough suppression).
Past medical history is remarkable for chronic obstructive pulmonary disease (COPD) and chronic bronchitis. Six months ago, a pulmonary function test revealed an FEV1 of 76% and an FEV1/FVC of 60%. He has chronic, mild to moderate shortness of breath with exertion. He has never had pneumonia or any anginal symptoms. Past surgical history is remarkable for an open reduction and internal fixation repair of his right tibia and an appendectomy. Current medications include acetaminophen for fever. He has used an albuterol inhaler in the past but has not had one for more than a year. He has no known drug allergies.
The patient is a crane operator for a large construction business. He is divorced and has an adult son with whom he has no contact. He’s been smoking 1.5 to 2 packs a day since he was 16. He used recreational marijuana until his employer began conducting random drug screenings 3 years ago. He drinks about 2 six-packs of beer a week—most of it on the weekends.
Family history is positive for COPD (mother), acute abdominal aortic dissection (father), and myocardial infarction (paternal grandfather).
The review of systems is positive for myalgias and arthralgias, which have been exacerbated by his recent illness. He denies a productive cough and any changes in heart rhythm and bowel or bladder function. He has no neurologic symptoms.
His vital signs include a blood pressure of 164/96 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 92% on room air; and temperature, 99.8°F.
Physical exam reveals an anxious, tired man in mild distress. His weight is 164 lb and his height, 70 in. The HEENT exam reveals ill-fitting corrective contact lenses, disheveled hair, and a nicotine-stained beard and mustache. His teeth are in poor repair; however, none are loose or missing. The neck is supple, and there is no thyromegaly. There is jugular venous distention, but not to the angle of the jaw. His respirations are shallow, requiring the use of accessory muscles. Deep inhalation causes uncontrollable coughing. Although there is anterior-posterior chest wall enlargement, it is insufficient to consider the patient barrel chested. Auscultation reveals diffuse, coarse rhonchi and end-expiratory wheezing.
The cardiac exam reveals a regular rate and rhythm of 80 beats/min, with a soft diastolic murmur (grade II/VI) that is best heard along the left sternal border. There are no extra heart sounds or rubs. The abdomen is tender to deep palpation in the right upper quadrant, with no evidence of rebound to suggest peritonitis. There are no abdominal or femoral arterial bruits. The extremities demonstrate 2+ pulses bilaterally with 1+ pitting edema in the lower legs. The neurologic exam is grossly intact.
The previously undocumented murmur prompts you to order an ECG. It shows a ventricular rate of 83 beats/min; PR interval, 178 ms; QRS duration, 110 ms; QT/QTc interval, 406/477 ms; P axis, 67°; R axis, 126°; and T axis, –57°. What is your interpretation of this ECG?
A Vital Clue to the Problem
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
Two days ago, a 76-year-old man underwent surgical repair of a left femoral fracture sustained in an automobile accident. Last night, his vital signs were concerning for asymptomatic bradycardia, prompting an order for ECG prior to morning rounds. His postoperative surgical course has been otherwise uneventful, and he is using minimal narcotic analgesia.
The patient has a long history of mild hypertension, which is well controlled with hydrochlorothiazide (50 mg/d). Otherwise, his medical history shows no angina, dyspnea, shortness of breath, or palpitations. There is no history of thyroid dysfunction or renal disease.
A pack-a-day smoker since age 15, the patient has been using a nicotine patch during his hospital stay. In the past 36 hours, he has taken 4 acetaminophen/oxycodone tablets (325/5 mg).
The patient works on a 400-acre ranch with about 100 head of cattle. His alcohol consumption was heavy until about 12 years ago, when he “blacked out” and gave up drinking altogether. He attends Alcoholics Anonymous meetings and leads sessions at his church. He denies recreational or illicit drug use.
Family history is positive for prostate cancer in his father and lung cancer in two brothers. His mother died of a hemorrhagic stroke at age 84.
The review of systems is remarkable only for discomfort due to an indwelling Foley catheter placed at the time of the surgery. He has no other specific complaints.
This morning, his vital signs include a blood pressure of 108/60 mm Hg; pulse, 42 beats/min; and O2 saturation, 100% on 2L of oxygen via nasal prongs.
When you arrive at the patient’s room, the ECG is in progress. The technician expresses concern about the tracing and shows you that the electrodes are placed properly. Looking at the ECG, you see a ventricular rate of 42 beats/min; PR interval, unmeasured; QRS duration, 130 ms; QT/QTc interval, 514/429 ms; P axis, +83°; R axis, +84°; and T axis, –43°. What is your interpretation?