User login
ANSWER
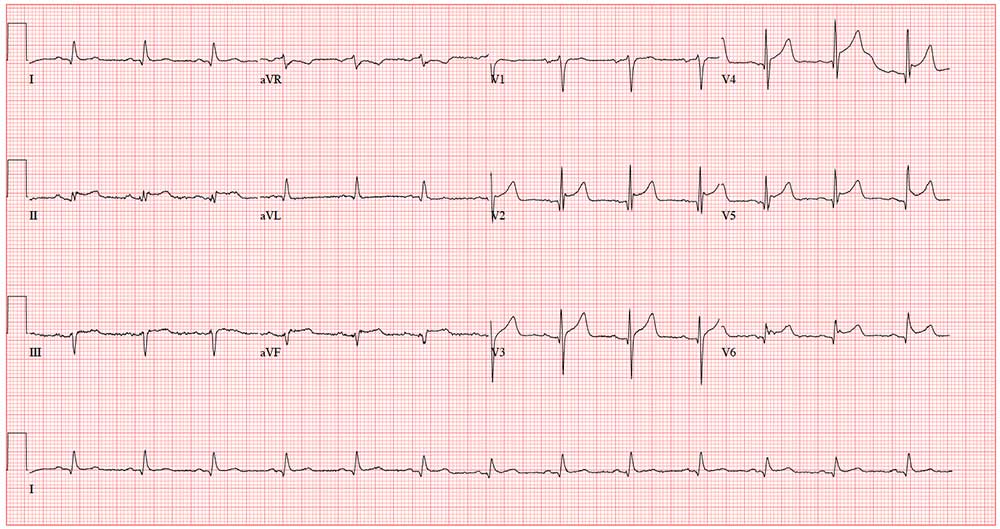
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
ANSWER
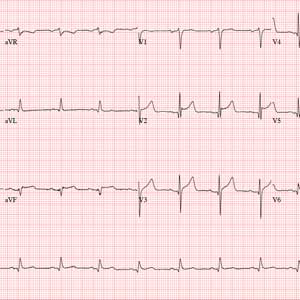
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
ANSWER
This ECG shows normal sinus rhythm, an anterior myocardial infarction, and inferolateral injury consistent with an acute ST-elevation myocardial infarction (STEMI).
A P wave for every QRS complex and a QRS complex with every P wave, with a consistent PR interval and a rate > 60 and < 100 beats/min, signifies sinus rhythm.
Criteria for an anterior STEMI include new ST elevation (≥ 2 mm [0.2 mV]) at the J point in leads V3 and V4. Inferolateral injury is indicated inferiorly by ST changes in leads II, III, and aVL and laterally by the ST elevation in leads V5 and V6.
Subsequent cardiac catheterization showed an occluded proximal left anterior descending artery and significant diagonal and obtuse marginal disease.
A 58-year-old man is snowmobiling with friends when he develops crushing substernal chest pain. He immediately stops his snowmobile and waves his arms for help—but by the time his friends reach him, he is lying on the ground, clutching his chest.
When asked what happened, he tells his friends that he’s been experiencing chest pain for the past hour but didn’t want to stop or interrupt their fun. He further reveals that he’s had chest “twinges” for the past 2 months, but they were always brief, and he didn’t think they were anything to be concerned about. He acknowledges that the current episode is “far worse” than what he previously experienced.
Because they are in the wilderness, no one in the group is able to establish cellphone service to call 911. The patient is loaded onto the back of another snowmobile for the 30-minute ride to the parking lot, where cellular service is accessible. They call 911, and an ACLS ambulance arrives about 50 minutes later.
An ECG is obtained in the field and transmitted to the receiving hospital, and the catherization lab is notified of an incoming patient. Transport to the hospital takes an hour; during the trip, the patient is administered oxygen, morphine, nitroglycerin, and an aspirin, and he is noted to have several nonsustained episodes of polymorphic ventricular tachycardia. The patient arrives at the hospital about 4 hours after onset of chest pain.
Medical history includes longstanding uncontrolled hypertension, recent onset of type 2 diabetes, and gastric reflux. He has never had shortness of breath, dyspnea on exertion, syncope, or near-syncope.
Current medications include lisinopril and metformin. However, the patient informs you that he hasn’t taken lisinopril in more than 3 months, and although he’s been given a prescription for metformin, he hasn’t filled it. He has no known drug allergies.
The patient is a mechanic at a local auto dealership. He smokes between 1 and 1.5 packs of cigarettes per day and has attempted to quit several times. He also consumes about 1 case of beer per week.
He is divorced, has no children, and lives alone. Both parents died in an automobile accident. The patient knows his father had several heart attacks beginning in his mid-50s and his mother “had thyroid problems.” His grandparents were known to have coronary artery disease and diabetes.
Review of systems is positive for a longstanding smoker’s cough and a healing burn on his right forearm, attributed to a welding injury.
His pretransport vital signs include a blood pressure of 178/88 mm Hg; pulse, 88 beats/min; respiratory rate, 18 breaths/min-1; and temperature, 97.6ºF. His stated weight is 265 lb and his height, 69 in.
Your findings on the physical exam corroborate those called in by the paramedics: an obese white male in obvious distress but alert and cooperative. His lungs reveal diffuse rales and crackles that clear with vigorous coughing. His cardiac exam reveals a regular rhythm at a rate of 80 beats/min with no murmurs or rubs. The abdomen is obese but otherwise normal. There is no peripheral edema. Pulses are strong and equal bilaterally. The neurologic exam is grossly intact. A bandaged second-degree burn is noted on the lower right forearm.
A repeat ECG shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation?