User login
ANSWER
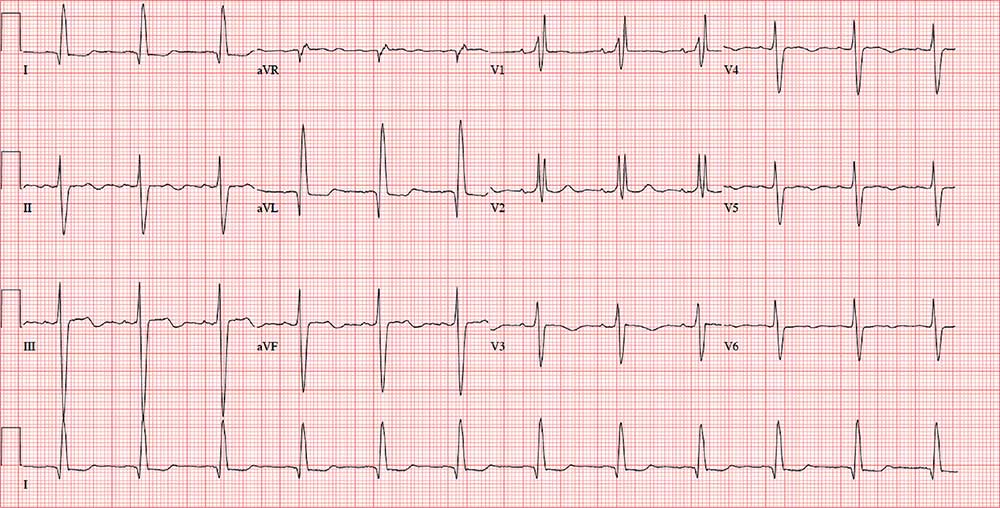
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with a right bundle branch block (RBBB) and a left anterior fascicular block (LAFB). The patient also has T-wave inversions in the inferior leads.
Normal sinus rhythm is evidenced by a ventricular rate ≥ 60 beats/min and < 100 beats/min, as well as a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval.
Criteria for a RBBB include a QRS > 120 ms with a biphasic RSR’ seen in leads V1–V3 and slurred S waves in leads I, aVL, V5, and V6. An LAFB is defined by left-axis deviation (–48° on this ECG), small Q waves with tall R waves in leads I and aVL, and small R waves and deep S waves in leads II, III, and aVF.
An RBBB plus an LAFB constitutes bifascicular block. In such cases, the ventricles are depolarized from one remaining fascicle: the left posterior. Affected patients are susceptible to complete heart block, particularly in the presence of congestive heart failure.
For those inexperienced with ECG interpretation, fascicular blocks may be confusing. Recall that evidence of Q waves in leads II, III, and aVF is associated with inferior myocardial infarction; by substituting the Q waves with S waves in the same leads, you won’t miss an LAFB.
For several years, a 75-year-old woman has been followed for aortic stenosis. Historically, she has done well—but about a year ago, she began experiencing shortness of breath. Within the past 2 months, she has had significantly increasing dyspnea with minimal activity and has experienced 2 episodes of near-syncope. This morning, she complains of chest tightness.
Her medical history is remarkable for hypertension, rheumatoid arthritis, and coronary artery disease. Two years ago, catheterization for chest pain revealed stenoses of her left anterior descending artery (LAD), a diagonal branch of the LAD, and an occluded right coronary artery. A drug-eluding stent was placed, and she has had no symptoms since. She also has a history of paroxysmal atrial fibrillation but has had no episodes in the past year.
An echocardiogram performed 1 week ago revealed severe aortic valve stenosis with a trileaflet valve with heavily calcified leaflets; an aortic valve gradient of 0.4 cm2, with a peak velocity of 5 m/s and a mean gradient of 61 mm Hg; and mild aortic regurgitation. It also showed an enlarged left atrium and mild-to-moderate mitral regurgitation.
Her current medications include senna glycoside, prednisone, metoprolol, atorvastatin, and apixaban. She has a true anaphylactic allergy to penicillin.
The patient, a retired administrative assistant, was widowed 4 years ago, when her husband died as a result of an automobile accident. They had no children. She has never smoked but reports having 1 to 2 glasses of wine each night.
Review of symptoms is positive for joint pain, particularly in her hands, hips, and knees. It is worse in the morning and improves as the day progresses. She tried NSAIDs but experienced bleeding, so she was recently started on prednisone. She also has chronic constipation, for which she takes senna with reasonable results. She denies any significant constitutional, respiratory, urologic, or neurologic symptoms.
Vital signs include a blood pressure of 146/86 mm Hg; pulse, 70 beats/min; respiratory rate, 14 breaths/min-1; temperature, 97.6°F; and O2 saturation, 96% on room air. Her weight is 139 lb and her height, 5 ft 5 in; her BMI is 23.1.
Physical exam reveals corrective lenses and bilateral hearing aids. The patient has multiple bruises of varying stages on both upper extremities. Her teeth are in good repair. There is no significant jugular venous distention or thyromegaly. The lungs are clear in all fields.
The cardiac exam is remarkable for a regular rate and rhythm, with a grade III/VI crescendo-decrescendo systolic murmur best heard at the right upper sternal border. She also has a grade II/VI late systolic murmur at the apex in the left lateral decubitus position. The A2 component of the second heart sound is absent, and there are no gallops or rubs.
The abdominal exam is normal, without palpable masses. Her peripheral pulses are strong and equal bilaterally. She has arthritic changes in her hands bilaterally and has no focal neurologic symptoms.
Her ECG reveals a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation?