User login
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
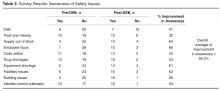
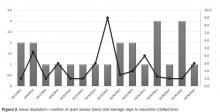
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
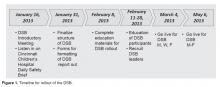
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.