User login
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
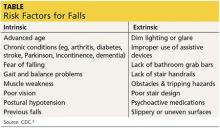
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.