User login
From the Multi-County eConsult Initiative, Rancho Cucamonga, CA.
The COVID-19 pandemic has forced many health care professionals and their patients to use telehealth and virtual care to address care needs in new ways.1 To shed light on care coordination decisions with respect to specialty resource access, we analyzed data collected from the Multi-County eConsult Initiative (MCeI)—the second-largest electronic consultation (eConsult) program in the United States—before and during the COVID-19 pandemic. Our analysis of these data suggests opportunities for improving access to care and reducing unnecessary costs in the health system nationally.
The Inland Empire Health Plan (IEHP) launched MCeI (econsultie.com) in 2018. The initiative is a partnership between IEHP, Arrowhead Regional Medical Center, and Riverside University Health System aimed at improving access to specialty care for the safety-net population across San Bernardino and Riverside counties. IEHP is 1 of the 10 largest Medicaid health plans and the largest not-for-profit Medicare-Medicaid plan in the country, serving more than 1.2 million members.2 Data from MCel reveal the impacts of COVID-19 on eConsult use and offer insights into specialty resource availability during and outside of a crisis.
At the time of this analysis, 86 IEHP clinics in rural and urban settings across 38 specialties used the eConsult process to provide and obtain virtual specialty care, as well as timely appointments for in-person specialty care.3 eConsults are facilitated through a HIPAA-secure web-based portal that enables communication and sharing of information between the primary care provider (PCP) and a specialist. eConsult gives PCPs virtual access to specialists to coordinate care for their patients and determine the need for in-person specialty visits. Through the PCP-specialist eConsult dialogue, patients gain virtual access to specialty care. If a PCP-specialist care team determines the patient needs an in-person visit, that specialty referral is automatically authorized by IEHP, without the need for further review. At IEHP, eConsult is the primary method used for obtaining outpatient specialty referrals.
To analyze eConsult utilization before and during the pandemic, we gathered data from the MCeI program for the periods February 20–March 19, 2020, and March 20–April 19, 2020. Measures included eConsult volume and outcomes of eConsults (eConsults closed as referrals for face-to-face specialist visits versus eConsults closed without resulting in referrals for face-to-face specialist visits). Statistical analysis using chi-square tests for independence was performed using IBM SPSS Statistics 25 (IBM, Armonk, NY).
The data show that after California’s stay-at-home order, issued on March 19, 2020,4 eConsult volumes initially decreased, reflecting a similar decrease in clinic visits and authorization requests submitted to IEHP. We observed a 4-week average of 1100 eConsults processed before the pandemic, and then a steep drop to a 4-week average of 500 eConsults processed after the stay-at-home order was issued. Despite the overall drop in the volume of eConsults submitted, demand for specialties like hematology and neurology remained high throughout the pandemic.
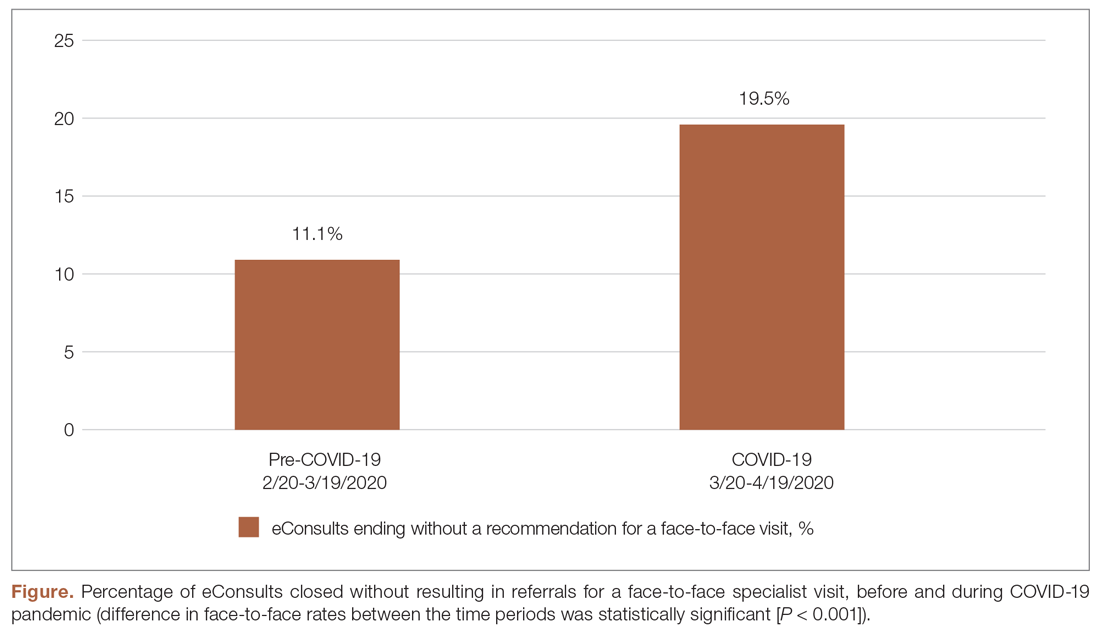
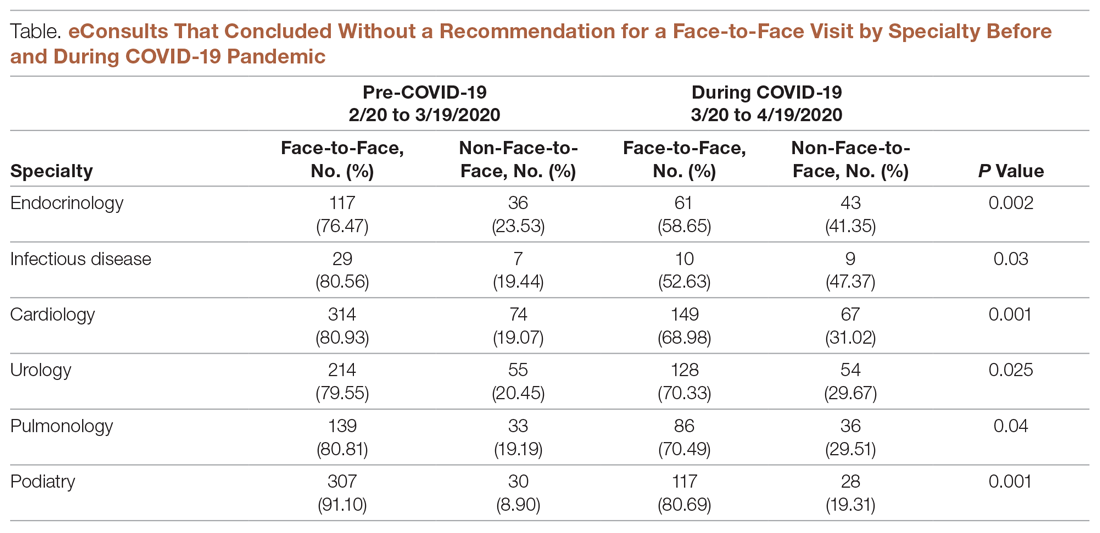
During the pandemic, certain specialties displayed rising rates of eConsults completed with specialists providing care recommendations to the PCP instead of resulting in a recommendation for a face-to-face (in-person or via telehealth) visit with a specialist (see Figure and Table). The trend of increasing eConsults that concluded without a face-to-face visit suggests newfound clinical consideration of limited medical resources, along with the desire to eliminate unnecessary risks of infection.
eConsults between PCPs and specialist reviewers via the IEHP portal resulted in higher rates of non-face-to-face recommendations. The specialist reviewers were able to provide treatment plans for PCPs to take care of patients without having to refer their patients to a specialist. This increase was significant across most of the specialties live on the MCeI program.
We believe that clinicians’ heightened awareness of the limitations of the US health care system should remain a key consideration and factor in medical decision-making about appropriate referrals after the pandemic has passed. The data demonstrate that the pandemic drove clinicians to make different decisions about referrals and care coordination. Physicians scrutinized individual cases more keenly and were not as quick to recommend a face-to-face visit. This awareness and consideration of specialty access before making a referral provides a valuable lesson. If this approach is applied to health care delivery post-pandemic, eConsults will help reduce unnecessary in-person specialist visits and will free up space and time for patients who genuinely do need in-person specialty care. In this way, eConsult will improve appropriate access to care for everyone and reduce unnecessary costs to the health care system at large.
An examination of eConsult utilization trends across Riverside and San Bernardino counties before and during the COVID-19 pandemic provides useful insights into how to reduce costs and improve access to care. Although the risk of exposure to COVID-19 currently presents a significant obstacle to obtaining in-person specialty care, pre-existing and long-standing barriers, such as long wait times and scarcity of specialists, remain critical issues to receiving care during and after the pandemic. The pandemic has proven eConsult’s value as a tool for effective care coordination. Leveraging provider-to-provider asynchronous communication offers an opportunity to reduce unnecessary utilization of scarce resources during and beyond the pandemic.
Corresponding author: Lisa Aubry, Aubry-L@iehp.org.
Financial disclosures: None.
Keywords: electronic consultation; care coordination; telehealth; telemedicine; virtual care.
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957-962.
2. Nash-Wong K. Inland Empire Health Plan Multi-county eConsult Initiative with Safety Net Connect improves specialty care for Southern California residents. [Press Release]. (July 24, 2019). www.businesswire.com/news/home/20190724005208/en/Inland-Empire-Health-Plan-Multi-county-eConsult-Initiative. Accessed July 16, 2020.
3. The Multi-County eConsult Initiative (March 2018). https://www.eConsultie.com. Accessed July 16, 2020.
4. Executive Department State of California. Exec. Order No. N-33-20 of March 19, 2020. Safer at Home, Stay at Home. www.gov.ca.gov. Accessed July 16, 2020.
From the Multi-County eConsult Initiative, Rancho Cucamonga, CA.
The COVID-19 pandemic has forced many health care professionals and their patients to use telehealth and virtual care to address care needs in new ways.1 To shed light on care coordination decisions with respect to specialty resource access, we analyzed data collected from the Multi-County eConsult Initiative (MCeI)—the second-largest electronic consultation (eConsult) program in the United States—before and during the COVID-19 pandemic. Our analysis of these data suggests opportunities for improving access to care and reducing unnecessary costs in the health system nationally.
The Inland Empire Health Plan (IEHP) launched MCeI (econsultie.com) in 2018. The initiative is a partnership between IEHP, Arrowhead Regional Medical Center, and Riverside University Health System aimed at improving access to specialty care for the safety-net population across San Bernardino and Riverside counties. IEHP is 1 of the 10 largest Medicaid health plans and the largest not-for-profit Medicare-Medicaid plan in the country, serving more than 1.2 million members.2 Data from MCel reveal the impacts of COVID-19 on eConsult use and offer insights into specialty resource availability during and outside of a crisis.
At the time of this analysis, 86 IEHP clinics in rural and urban settings across 38 specialties used the eConsult process to provide and obtain virtual specialty care, as well as timely appointments for in-person specialty care.3 eConsults are facilitated through a HIPAA-secure web-based portal that enables communication and sharing of information between the primary care provider (PCP) and a specialist. eConsult gives PCPs virtual access to specialists to coordinate care for their patients and determine the need for in-person specialty visits. Through the PCP-specialist eConsult dialogue, patients gain virtual access to specialty care. If a PCP-specialist care team determines the patient needs an in-person visit, that specialty referral is automatically authorized by IEHP, without the need for further review. At IEHP, eConsult is the primary method used for obtaining outpatient specialty referrals.
To analyze eConsult utilization before and during the pandemic, we gathered data from the MCeI program for the periods February 20–March 19, 2020, and March 20–April 19, 2020. Measures included eConsult volume and outcomes of eConsults (eConsults closed as referrals for face-to-face specialist visits versus eConsults closed without resulting in referrals for face-to-face specialist visits). Statistical analysis using chi-square tests for independence was performed using IBM SPSS Statistics 25 (IBM, Armonk, NY).
The data show that after California’s stay-at-home order, issued on March 19, 2020,4 eConsult volumes initially decreased, reflecting a similar decrease in clinic visits and authorization requests submitted to IEHP. We observed a 4-week average of 1100 eConsults processed before the pandemic, and then a steep drop to a 4-week average of 500 eConsults processed after the stay-at-home order was issued. Despite the overall drop in the volume of eConsults submitted, demand for specialties like hematology and neurology remained high throughout the pandemic.
During the pandemic, certain specialties displayed rising rates of eConsults completed with specialists providing care recommendations to the PCP instead of resulting in a recommendation for a face-to-face (in-person or via telehealth) visit with a specialist (see Figure and Table). The trend of increasing eConsults that concluded without a face-to-face visit suggests newfound clinical consideration of limited medical resources, along with the desire to eliminate unnecessary risks of infection.
eConsults between PCPs and specialist reviewers via the IEHP portal resulted in higher rates of non-face-to-face recommendations. The specialist reviewers were able to provide treatment plans for PCPs to take care of patients without having to refer their patients to a specialist. This increase was significant across most of the specialties live on the MCeI program.
We believe that clinicians’ heightened awareness of the limitations of the US health care system should remain a key consideration and factor in medical decision-making about appropriate referrals after the pandemic has passed. The data demonstrate that the pandemic drove clinicians to make different decisions about referrals and care coordination. Physicians scrutinized individual cases more keenly and were not as quick to recommend a face-to-face visit. This awareness and consideration of specialty access before making a referral provides a valuable lesson. If this approach is applied to health care delivery post-pandemic, eConsults will help reduce unnecessary in-person specialist visits and will free up space and time for patients who genuinely do need in-person specialty care. In this way, eConsult will improve appropriate access to care for everyone and reduce unnecessary costs to the health care system at large.
An examination of eConsult utilization trends across Riverside and San Bernardino counties before and during the COVID-19 pandemic provides useful insights into how to reduce costs and improve access to care. Although the risk of exposure to COVID-19 currently presents a significant obstacle to obtaining in-person specialty care, pre-existing and long-standing barriers, such as long wait times and scarcity of specialists, remain critical issues to receiving care during and after the pandemic. The pandemic has proven eConsult’s value as a tool for effective care coordination. Leveraging provider-to-provider asynchronous communication offers an opportunity to reduce unnecessary utilization of scarce resources during and beyond the pandemic.
Corresponding author: Lisa Aubry, Aubry-L@iehp.org.
Financial disclosures: None.
Keywords: electronic consultation; care coordination; telehealth; telemedicine; virtual care.
From the Multi-County eConsult Initiative, Rancho Cucamonga, CA.
The COVID-19 pandemic has forced many health care professionals and their patients to use telehealth and virtual care to address care needs in new ways.1 To shed light on care coordination decisions with respect to specialty resource access, we analyzed data collected from the Multi-County eConsult Initiative (MCeI)—the second-largest electronic consultation (eConsult) program in the United States—before and during the COVID-19 pandemic. Our analysis of these data suggests opportunities for improving access to care and reducing unnecessary costs in the health system nationally.
The Inland Empire Health Plan (IEHP) launched MCeI (econsultie.com) in 2018. The initiative is a partnership between IEHP, Arrowhead Regional Medical Center, and Riverside University Health System aimed at improving access to specialty care for the safety-net population across San Bernardino and Riverside counties. IEHP is 1 of the 10 largest Medicaid health plans and the largest not-for-profit Medicare-Medicaid plan in the country, serving more than 1.2 million members.2 Data from MCel reveal the impacts of COVID-19 on eConsult use and offer insights into specialty resource availability during and outside of a crisis.
At the time of this analysis, 86 IEHP clinics in rural and urban settings across 38 specialties used the eConsult process to provide and obtain virtual specialty care, as well as timely appointments for in-person specialty care.3 eConsults are facilitated through a HIPAA-secure web-based portal that enables communication and sharing of information between the primary care provider (PCP) and a specialist. eConsult gives PCPs virtual access to specialists to coordinate care for their patients and determine the need for in-person specialty visits. Through the PCP-specialist eConsult dialogue, patients gain virtual access to specialty care. If a PCP-specialist care team determines the patient needs an in-person visit, that specialty referral is automatically authorized by IEHP, without the need for further review. At IEHP, eConsult is the primary method used for obtaining outpatient specialty referrals.
To analyze eConsult utilization before and during the pandemic, we gathered data from the MCeI program for the periods February 20–March 19, 2020, and March 20–April 19, 2020. Measures included eConsult volume and outcomes of eConsults (eConsults closed as referrals for face-to-face specialist visits versus eConsults closed without resulting in referrals for face-to-face specialist visits). Statistical analysis using chi-square tests for independence was performed using IBM SPSS Statistics 25 (IBM, Armonk, NY).
The data show that after California’s stay-at-home order, issued on March 19, 2020,4 eConsult volumes initially decreased, reflecting a similar decrease in clinic visits and authorization requests submitted to IEHP. We observed a 4-week average of 1100 eConsults processed before the pandemic, and then a steep drop to a 4-week average of 500 eConsults processed after the stay-at-home order was issued. Despite the overall drop in the volume of eConsults submitted, demand for specialties like hematology and neurology remained high throughout the pandemic.
During the pandemic, certain specialties displayed rising rates of eConsults completed with specialists providing care recommendations to the PCP instead of resulting in a recommendation for a face-to-face (in-person or via telehealth) visit with a specialist (see Figure and Table). The trend of increasing eConsults that concluded without a face-to-face visit suggests newfound clinical consideration of limited medical resources, along with the desire to eliminate unnecessary risks of infection.
eConsults between PCPs and specialist reviewers via the IEHP portal resulted in higher rates of non-face-to-face recommendations. The specialist reviewers were able to provide treatment plans for PCPs to take care of patients without having to refer their patients to a specialist. This increase was significant across most of the specialties live on the MCeI program.
We believe that clinicians’ heightened awareness of the limitations of the US health care system should remain a key consideration and factor in medical decision-making about appropriate referrals after the pandemic has passed. The data demonstrate that the pandemic drove clinicians to make different decisions about referrals and care coordination. Physicians scrutinized individual cases more keenly and were not as quick to recommend a face-to-face visit. This awareness and consideration of specialty access before making a referral provides a valuable lesson. If this approach is applied to health care delivery post-pandemic, eConsults will help reduce unnecessary in-person specialist visits and will free up space and time for patients who genuinely do need in-person specialty care. In this way, eConsult will improve appropriate access to care for everyone and reduce unnecessary costs to the health care system at large.
An examination of eConsult utilization trends across Riverside and San Bernardino counties before and during the COVID-19 pandemic provides useful insights into how to reduce costs and improve access to care. Although the risk of exposure to COVID-19 currently presents a significant obstacle to obtaining in-person specialty care, pre-existing and long-standing barriers, such as long wait times and scarcity of specialists, remain critical issues to receiving care during and after the pandemic. The pandemic has proven eConsult’s value as a tool for effective care coordination. Leveraging provider-to-provider asynchronous communication offers an opportunity to reduce unnecessary utilization of scarce resources during and beyond the pandemic.
Corresponding author: Lisa Aubry, Aubry-L@iehp.org.
Financial disclosures: None.
Keywords: electronic consultation; care coordination; telehealth; telemedicine; virtual care.
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957-962.
2. Nash-Wong K. Inland Empire Health Plan Multi-county eConsult Initiative with Safety Net Connect improves specialty care for Southern California residents. [Press Release]. (July 24, 2019). www.businesswire.com/news/home/20190724005208/en/Inland-Empire-Health-Plan-Multi-county-eConsult-Initiative. Accessed July 16, 2020.
3. The Multi-County eConsult Initiative (March 2018). https://www.eConsultie.com. Accessed July 16, 2020.
4. Executive Department State of California. Exec. Order No. N-33-20 of March 19, 2020. Safer at Home, Stay at Home. www.gov.ca.gov. Accessed July 16, 2020.
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957-962.
2. Nash-Wong K. Inland Empire Health Plan Multi-county eConsult Initiative with Safety Net Connect improves specialty care for Southern California residents. [Press Release]. (July 24, 2019). www.businesswire.com/news/home/20190724005208/en/Inland-Empire-Health-Plan-Multi-county-eConsult-Initiative. Accessed July 16, 2020.
3. The Multi-County eConsult Initiative (March 2018). https://www.eConsultie.com. Accessed July 16, 2020.
4. Executive Department State of California. Exec. Order No. N-33-20 of March 19, 2020. Safer at Home, Stay at Home. www.gov.ca.gov. Accessed July 16, 2020.