User login
ANSWER
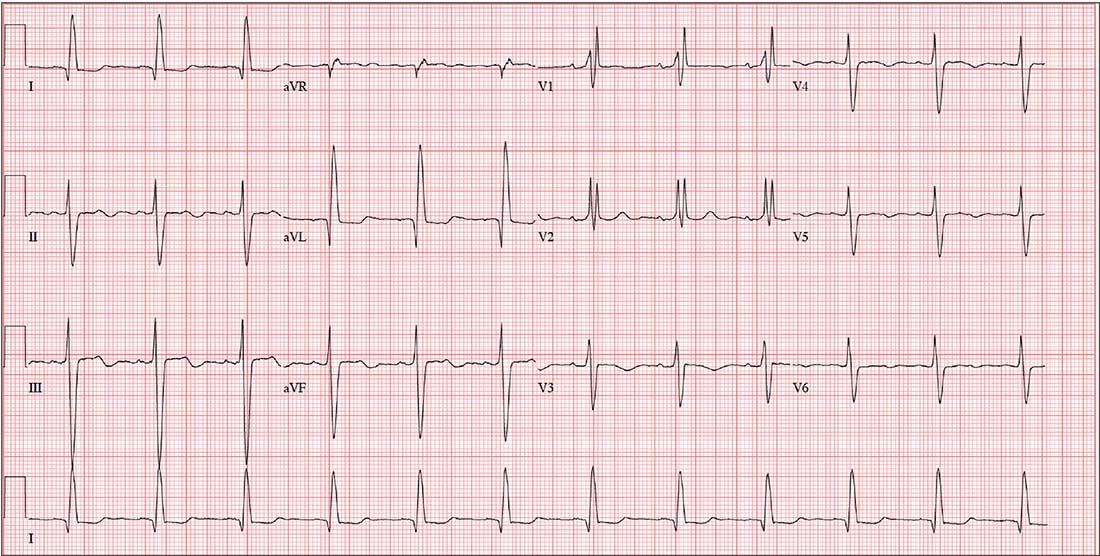
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
ANSWER
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
ANSWER
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
A 79-year-old man with a history of aortic stenosis presents for preoperative evaluation for aortic valve replacement versus transcatheter aortic valve placement. Over the past three months, he has developed worsening shortness of breath, dyspnea on exertion, chest tightness, and lightheadedness, but no frank syncope. One month ago, he was hospitalized for heart failure, which improved with IV diuresis.
An echocardiogram performed one week ago showed an aortic valve area of 0.5 cm, with a peak velocity of 5.4 m/s and a mean gradient of 64 mm Hg. The left ventricular function was normal, with an ejection fraction of 72%. The pulmonary artery pressure measured 40 mm Hg. Other findings included mild-to-moderate mitral and tricuspid valve regurgitation.
Cardiac history is also positive for coronary artery disease, with a recent coronary angiogram showing 60% stenosis in the proximal left anterior descending artery and 80% stenosis of the mid-portion of the right coronary artery.
Medical history is positive for hypertension, type 2 diabetes, and osteoarthritis. Surgical history includes bilateral knee replacements. Current medications include aspirin, furosemide, metformin, atorvastatin, and metoprolol. The patient is allergic to sulfa-containing medications.
Social history reveals that he is a retired police officer who is married and has three adult children. He does not smoke, enjoys an occasional beer, and denies recreational drug use. Family history is notable for coronary artery disease, hypertension, and diabetes.
Review of systems reveals no additional complaints. It is noted that he wears hearing aids and glasses.
Vital signs include a blood pressure of 110/64 mm Hg; pulse, 70 beats/min; and respiratory rate, 14 breaths/min-1. O2 saturation is 96% on room air. His weight is 214 lb and his height, 74 in.
On physical exam, you find a congenial but inquisitive male in no distress, with jugular venous distention at 8 cm, clear lung fields, and a regular heart rate and rhythm. There is a grade 3/6 systolic ejection murmur at the right upper sternal border but no extra heart sounds or rubs. The abdomen is soft and nontender. Peripheral pulses are 2+ bilaterally without femoral bruits, and surgical scars are present over both knees. There is trace pitting edema bilaterally in the lower extremities. The neurologic exam is intact, without focal signs.
An ECG, obtained as part of his preoperative workup, reveals a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation?