User login
New CPR Guide Sets Compression Limits, Scratches Vasopressin
By Shannon Aymes
From Circulation
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
Vitals Key clinical point: The percentage of nonmedical use of prescription opioids declined during the last decade, but the prevalence of use disorders, the frequency of abuse, and related mortality all increased. Major finding: The 1-year prevalence of opioid use disorders rose from 0.6% to 0.9%, that of high-frequency use increased from 0.3% to 0.4%, and that of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. Data source: An analysis of time trends in prescription opioid use, based on two nationally representative data sets involving 472,200 adults. Disclosures: The Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the US Food and Drug Administration (FDA) sponsored the study. Dr Han reported having no relevant disclosures; an associate reported owning stock in General Electric, 3M Company, and Pfizer. |
The American Heart Association (AHA) published its revised guidelines October 15 in Circulation.1 The AHA released its previous guidelines in 2010.2
“When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” Dr Mark Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, said in a statement.
The 2015 guidelines’ new recommendations include the following:
Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In an OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps—such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval—can be accomplished simultaneously.
High-quality CPR. The guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote.
Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32°C and 36°C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32°C to 34°C for 12 to 24 hours.
The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
Complex Picture Emerges of Prescription Opioid Abuse
By Mary Ann Moon
From JAMA
These findings—from an analysis of two large nationally representative data sets—paint a picture that is complex and more nuanced than that suggested by some recent reports. For example, a study of the Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) System found that the abuse and diversion of prescription opioids plateaued or decreased in recent years.3 “The nationally representative results in our study may be especially important in providing an accurate picture of the current status of the epidemic,” said Dr Beth Han of the Substance Abuse and Mental Health Services Administration (SAMHSA), Rockville, Maryland, and her associates.
The nonmedical use of prescription opioids is an acknowledged epidemic, but that epidemic’s changing pattern over time needed to be updated. The investigators assessed the changes in use during the most recent decade for which data are available (2003-2013) using annual surveys conducted by SAMHSA and cause of death files from the National Vital Statistics System.
Based on responses from 472,200 people aged 18 to 64 years, the 1-year prevalence of nonmedical use of prescription opioids decreased from 5.4% to 4.9% during the study period. However, the 1-year prevalence of use disorders rose from 0.6% to 0.9%, the 1-year prevalence of high-frequency use (200 days or more per year) increased from 0.3% to 0.4%, and the rate of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. In addition, the mean number of days of opioid abuse increased from 2.1 to 2.6 per year in the general population and from 40.0 to 54.2 days per year among acknowledged opioid users, the investigators said.1
Compared with white users of prescription opioids, both black and Hispanic users had a lower prevalence of use disorders. The prevalence of use disorders was higher among less-educated than more-educated adults, among those with no health insurance or Medicaid as opposed to private health insurance, and among smokers than nonsmokers, Dr Han and her associates added.
Previous research has shown that most adults who abuse prescription opioids neither receive treatment nor perceive that they need treatment. Clinicians can help by using prescription-drug monitoring programs to identify inappropriate receipt of prescription opioids, then offering treatments, which are highly effective, for patients who need them, the investigators noted.
The slight decline (approximately 0.4% over 10 years) in opioid initiation reported by Han et al1 may be encouraging, but their other findings suggest that more patients are experiencing an inexorable progression from initial opioid use to frequent use to highly frequent use to a use disorder.
The source of most opioid abuse is often a seemingly legitimate prescription, and the key to addressing the opioid-abuse epidemic is to keep opioid-naive patients opioid naive. It is still unclear why clinicians continue to prescribe opioids, despite recommendations to the contrary and the fact that these agents provide little or no long-term benefit for most types of chronic pain.
Lewis S. Nelson, MD, is in the Ronald O. Perelman department of emergency medicine at New York University. He and his associates made these remarks in an editorial2 accompanying Dr Han’s report.1
US Injury Costs Topped $671 Billion in 2013
By Richard Franki
From MMWR
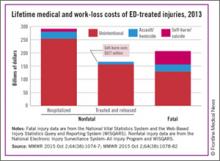
Over 30 million injuries were treated in US EDs in 2013, costing an estimated $671 billion, the CDC reported.
The largest share of that cost—almost $290 billion, or about 43%—came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from EDs were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, PhD, of the CDC’s National Center for Injury Prevention and Control, Atlanta, Georgia, and associates.
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said.1
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr Florence and associates noted.
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
Peramivir Effective Against Most Flu Viruses Circulating Globally
By Doug Brunk
AT ICAAC 2015
Vitals Key clinical point: Peramivir is potently effective against seasonal influenza viruses circulating globally. Major finding: During the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir. Data source: An analysis of 8,426 influenza viruses that were tested during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System.1 Disclosures: The researchers reporting having no financial disclosures. |
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013 to 2014 and 2014 to 2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, PhD, at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC/ICC 2015). In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr Okomo-Adhiambo of the influenza division at the US Centers for Disease Control and Prevention (CDC), Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.1
Dr Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
Parasitic Infection Emerging in the Southwestern United States
By Doug Brunk
At IDWEEK 2015
Vitals Key clinical point: Lesions containing a zoonotic parasite known as Onchocerca lupi are appearing in humans who reside in the Southwestern United States. Major finding: In three of six human cases, nodules containing Onchocerca lupi were located in the cervical spinal canal. Data source: A case report of the first six people in the United States to be infected with Onchocerca lupi. Disclosures: The researchers reported having no financial disclosures. |
SAN DIEGO – Onchocerca lupi, a zoonotic parasite previously described as causing eye disease in cats and dogs, as well as in humans from Europe, Asia, and the Middle East, is emerging in the Southwestern United States.
“The life cycle of this organism is not yet clearly defined, but likely includes a canine and/or feline animal reservoir, as well as an insect vector,” Dr Christiana Smith said in an interview at an annual scientific meeting on infectious diseases.1 “No specific risk factors for developing this disease have been identified, other than residing in or traveling through the Southwestern US.”
To date, six cases of humans infected by Onchocerca lupi have come to the attention of health officials, including those at the CDC, due to symptoms from a nodule containing the parasite, according to Dr Smith, a pediatrician with the University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora. The affected patients range in age from 22 months to 50 years of age; three of the six reside in Arizona, two in New Mexico, and one in Texas.
In three of the six cases, the nodule was located in the cervical spinal canal. In the remaining three cases, nodules were located on the scalp, the forearm, and the superior rectus muscle of the orbit. Two of the patients reported insect bites at the nodule site years prior to presentation, while another patient owned a dog with eye lesions.
“No previous Onchocerca parasites are known to have tropism for the central nervous system,” Dr Smith said. “In addition, five of the six cases presented in children. It is not clear whether children are disproportionately affected by this disease, or whether they are diagnosed more frequently.”
Treatment included surgical excision and antiparasitic treatment for most cases. To date, all patients have remained asymptomatic following treatment. Dr Smith said that more information about Onchocerca lupi will become available as additional cases are described. “Continued epidemiologic investigation will help define the life cycle of this organism, describe the spectrum of human disease, develop approaches to diagnosis and management, and design prevention strategies,” she said.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
Europeans Adopt 1-Hour ED Chest Pain Triage
By Bruce Jancin
At the ESC Congress 2015
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study1 reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university ED with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.2
To view the video, search “Huber” at http://www.emed-journal.com/
- New CPR Guide Sets Compression Limits, Scratches Vasopressin
- Bhanji F, Donoghue AJ, Wolff MS, et al. Part 14: Education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S561-S573.
- Cave DM, Gazmuri RJ, Otto CW, et al. Part 7: CPR techniques and devices: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S720-S728.
- Complex Picture Emerges of Prescription Opioid Abuse
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468-1478.
- Nelson LS, Juurlink DN, Perrone J. Addressing the opioid epidemic. JAMA. 2015;314(14):1453-1454.
- Severtson SG, Bartelson BB, Davis JM, et al. Reduced abuse, therapeutic errors, and diversion following reformulation of extended-release ocycodone in 2010. J Pain. 2013;14(10):1122-1130.
- US Injury Costs Topped $671 Billion in 2013
- Florence C, Simon T, Haegerich T, Luo F, Zhou C. Estimated lifetime medical and work-loss costs of fatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;46(38):1074-1077.
- Florence C, Haegerich T, Simon T, Zhou C, Luo F. Estimated lifetime medical and work-loss costs of emergency department-treated nonfatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(38):1078-1082.
- Peramivir Effective Against Most Flu Viruses Circulating Globally
- Okomo-Adhiambo M, Daniels J, Nguyen HT, et al. Peramivir Susceptibility Surveillance of Influenza A and B Viruses Circulated Globally, 2013-2015. Presented at: Interscience Conference of Antimicrobial Agents and Chemotherapy (ICAAC) and the International Society of Chemotherapy (ISC)’s International Congress of Chemotherapy and Infection (ICC) 2015; September 17-21, 2015; San Diego, California
- Parasitic Infection Emerging in the Southwestern United States
- Smith C, Rao S, Dehority W, et al. Onchocerca lupi: An Emerging Parasitic Infection in the Southwestern United States. Poster presented at: Infectious Disease (ID) Week 2015; October 7-11, 2015; San Diego, California; Abstract 1971.
- Europeans Adopt 1-Hour ED Chest Pain Triage
- Universitätsklinikum Hamburg-Eppendorf. Biomarkers in Acute Cardiac Care (BACC). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02355457. NLM Identifier: NCT02355457.
- Westermann D. Accurate and rapid diagnosis of myocardial infarction using a high sensitivity Troponin I 1-hour algorithm. Presented at: European Society of Cardiology (ESC) Congress; August 29 - September 2, 2015; London, England. FP NR 1161.
New CPR Guide Sets Compression Limits, Scratches Vasopressin
By Shannon Aymes
From Circulation
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
Vitals Key clinical point: The percentage of nonmedical use of prescription opioids declined during the last decade, but the prevalence of use disorders, the frequency of abuse, and related mortality all increased. Major finding: The 1-year prevalence of opioid use disorders rose from 0.6% to 0.9%, that of high-frequency use increased from 0.3% to 0.4%, and that of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. Data source: An analysis of time trends in prescription opioid use, based on two nationally representative data sets involving 472,200 adults. Disclosures: The Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the US Food and Drug Administration (FDA) sponsored the study. Dr Han reported having no relevant disclosures; an associate reported owning stock in General Electric, 3M Company, and Pfizer. |
The American Heart Association (AHA) published its revised guidelines October 15 in Circulation.1 The AHA released its previous guidelines in 2010.2
“When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” Dr Mark Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, said in a statement.
The 2015 guidelines’ new recommendations include the following:
Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In an OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps—such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval—can be accomplished simultaneously.
High-quality CPR. The guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote.
Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32°C and 36°C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32°C to 34°C for 12 to 24 hours.
The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
Complex Picture Emerges of Prescription Opioid Abuse
By Mary Ann Moon
From JAMA
These findings—from an analysis of two large nationally representative data sets—paint a picture that is complex and more nuanced than that suggested by some recent reports. For example, a study of the Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) System found that the abuse and diversion of prescription opioids plateaued or decreased in recent years.3 “The nationally representative results in our study may be especially important in providing an accurate picture of the current status of the epidemic,” said Dr Beth Han of the Substance Abuse and Mental Health Services Administration (SAMHSA), Rockville, Maryland, and her associates.
The nonmedical use of prescription opioids is an acknowledged epidemic, but that epidemic’s changing pattern over time needed to be updated. The investigators assessed the changes in use during the most recent decade for which data are available (2003-2013) using annual surveys conducted by SAMHSA and cause of death files from the National Vital Statistics System.
Based on responses from 472,200 people aged 18 to 64 years, the 1-year prevalence of nonmedical use of prescription opioids decreased from 5.4% to 4.9% during the study period. However, the 1-year prevalence of use disorders rose from 0.6% to 0.9%, the 1-year prevalence of high-frequency use (200 days or more per year) increased from 0.3% to 0.4%, and the rate of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. In addition, the mean number of days of opioid abuse increased from 2.1 to 2.6 per year in the general population and from 40.0 to 54.2 days per year among acknowledged opioid users, the investigators said.1
Compared with white users of prescription opioids, both black and Hispanic users had a lower prevalence of use disorders. The prevalence of use disorders was higher among less-educated than more-educated adults, among those with no health insurance or Medicaid as opposed to private health insurance, and among smokers than nonsmokers, Dr Han and her associates added.
Previous research has shown that most adults who abuse prescription opioids neither receive treatment nor perceive that they need treatment. Clinicians can help by using prescription-drug monitoring programs to identify inappropriate receipt of prescription opioids, then offering treatments, which are highly effective, for patients who need them, the investigators noted.
The slight decline (approximately 0.4% over 10 years) in opioid initiation reported by Han et al1 may be encouraging, but their other findings suggest that more patients are experiencing an inexorable progression from initial opioid use to frequent use to highly frequent use to a use disorder.
The source of most opioid abuse is often a seemingly legitimate prescription, and the key to addressing the opioid-abuse epidemic is to keep opioid-naive patients opioid naive. It is still unclear why clinicians continue to prescribe opioids, despite recommendations to the contrary and the fact that these agents provide little or no long-term benefit for most types of chronic pain.
Lewis S. Nelson, MD, is in the Ronald O. Perelman department of emergency medicine at New York University. He and his associates made these remarks in an editorial2 accompanying Dr Han’s report.1
US Injury Costs Topped $671 Billion in 2013
By Richard Franki
From MMWR
Over 30 million injuries were treated in US EDs in 2013, costing an estimated $671 billion, the CDC reported.
The largest share of that cost—almost $290 billion, or about 43%—came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from EDs were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, PhD, of the CDC’s National Center for Injury Prevention and Control, Atlanta, Georgia, and associates.
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said.1
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr Florence and associates noted.
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
Peramivir Effective Against Most Flu Viruses Circulating Globally
By Doug Brunk
AT ICAAC 2015
Vitals Key clinical point: Peramivir is potently effective against seasonal influenza viruses circulating globally. Major finding: During the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir. Data source: An analysis of 8,426 influenza viruses that were tested during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System.1 Disclosures: The researchers reporting having no financial disclosures. |
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013 to 2014 and 2014 to 2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, PhD, at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC/ICC 2015). In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr Okomo-Adhiambo of the influenza division at the US Centers for Disease Control and Prevention (CDC), Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.1
Dr Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
Parasitic Infection Emerging in the Southwestern United States
By Doug Brunk
At IDWEEK 2015
Vitals Key clinical point: Lesions containing a zoonotic parasite known as Onchocerca lupi are appearing in humans who reside in the Southwestern United States. Major finding: In three of six human cases, nodules containing Onchocerca lupi were located in the cervical spinal canal. Data source: A case report of the first six people in the United States to be infected with Onchocerca lupi. Disclosures: The researchers reported having no financial disclosures. |
SAN DIEGO – Onchocerca lupi, a zoonotic parasite previously described as causing eye disease in cats and dogs, as well as in humans from Europe, Asia, and the Middle East, is emerging in the Southwestern United States.
“The life cycle of this organism is not yet clearly defined, but likely includes a canine and/or feline animal reservoir, as well as an insect vector,” Dr Christiana Smith said in an interview at an annual scientific meeting on infectious diseases.1 “No specific risk factors for developing this disease have been identified, other than residing in or traveling through the Southwestern US.”
To date, six cases of humans infected by Onchocerca lupi have come to the attention of health officials, including those at the CDC, due to symptoms from a nodule containing the parasite, according to Dr Smith, a pediatrician with the University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora. The affected patients range in age from 22 months to 50 years of age; three of the six reside in Arizona, two in New Mexico, and one in Texas.
In three of the six cases, the nodule was located in the cervical spinal canal. In the remaining three cases, nodules were located on the scalp, the forearm, and the superior rectus muscle of the orbit. Two of the patients reported insect bites at the nodule site years prior to presentation, while another patient owned a dog with eye lesions.
“No previous Onchocerca parasites are known to have tropism for the central nervous system,” Dr Smith said. “In addition, five of the six cases presented in children. It is not clear whether children are disproportionately affected by this disease, or whether they are diagnosed more frequently.”
Treatment included surgical excision and antiparasitic treatment for most cases. To date, all patients have remained asymptomatic following treatment. Dr Smith said that more information about Onchocerca lupi will become available as additional cases are described. “Continued epidemiologic investigation will help define the life cycle of this organism, describe the spectrum of human disease, develop approaches to diagnosis and management, and design prevention strategies,” she said.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
Europeans Adopt 1-Hour ED Chest Pain Triage
By Bruce Jancin
At the ESC Congress 2015
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study1 reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university ED with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.2
To view the video, search “Huber” at http://www.emed-journal.com/
New CPR Guide Sets Compression Limits, Scratches Vasopressin
By Shannon Aymes
From Circulation
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
Vitals Key clinical point: The percentage of nonmedical use of prescription opioids declined during the last decade, but the prevalence of use disorders, the frequency of abuse, and related mortality all increased. Major finding: The 1-year prevalence of opioid use disorders rose from 0.6% to 0.9%, that of high-frequency use increased from 0.3% to 0.4%, and that of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. Data source: An analysis of time trends in prescription opioid use, based on two nationally representative data sets involving 472,200 adults. Disclosures: The Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the US Food and Drug Administration (FDA) sponsored the study. Dr Han reported having no relevant disclosures; an associate reported owning stock in General Electric, 3M Company, and Pfizer. |
The American Heart Association (AHA) published its revised guidelines October 15 in Circulation.1 The AHA released its previous guidelines in 2010.2
“When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” Dr Mark Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, said in a statement.
The 2015 guidelines’ new recommendations include the following:
Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In an OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps—such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval—can be accomplished simultaneously.
High-quality CPR. The guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote.
Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32°C and 36°C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32°C to 34°C for 12 to 24 hours.
The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
Complex Picture Emerges of Prescription Opioid Abuse
By Mary Ann Moon
From JAMA
These findings—from an analysis of two large nationally representative data sets—paint a picture that is complex and more nuanced than that suggested by some recent reports. For example, a study of the Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) System found that the abuse and diversion of prescription opioids plateaued or decreased in recent years.3 “The nationally representative results in our study may be especially important in providing an accurate picture of the current status of the epidemic,” said Dr Beth Han of the Substance Abuse and Mental Health Services Administration (SAMHSA), Rockville, Maryland, and her associates.
The nonmedical use of prescription opioids is an acknowledged epidemic, but that epidemic’s changing pattern over time needed to be updated. The investigators assessed the changes in use during the most recent decade for which data are available (2003-2013) using annual surveys conducted by SAMHSA and cause of death files from the National Vital Statistics System.
Based on responses from 472,200 people aged 18 to 64 years, the 1-year prevalence of nonmedical use of prescription opioids decreased from 5.4% to 4.9% during the study period. However, the 1-year prevalence of use disorders rose from 0.6% to 0.9%, the 1-year prevalence of high-frequency use (200 days or more per year) increased from 0.3% to 0.4%, and the rate of opioid-related deaths increased from 4.5 per 100,000 to 7.8 per 100,000. In addition, the mean number of days of opioid abuse increased from 2.1 to 2.6 per year in the general population and from 40.0 to 54.2 days per year among acknowledged opioid users, the investigators said.1
Compared with white users of prescription opioids, both black and Hispanic users had a lower prevalence of use disorders. The prevalence of use disorders was higher among less-educated than more-educated adults, among those with no health insurance or Medicaid as opposed to private health insurance, and among smokers than nonsmokers, Dr Han and her associates added.
Previous research has shown that most adults who abuse prescription opioids neither receive treatment nor perceive that they need treatment. Clinicians can help by using prescription-drug monitoring programs to identify inappropriate receipt of prescription opioids, then offering treatments, which are highly effective, for patients who need them, the investigators noted.
The slight decline (approximately 0.4% over 10 years) in opioid initiation reported by Han et al1 may be encouraging, but their other findings suggest that more patients are experiencing an inexorable progression from initial opioid use to frequent use to highly frequent use to a use disorder.
The source of most opioid abuse is often a seemingly legitimate prescription, and the key to addressing the opioid-abuse epidemic is to keep opioid-naive patients opioid naive. It is still unclear why clinicians continue to prescribe opioids, despite recommendations to the contrary and the fact that these agents provide little or no long-term benefit for most types of chronic pain.
Lewis S. Nelson, MD, is in the Ronald O. Perelman department of emergency medicine at New York University. He and his associates made these remarks in an editorial2 accompanying Dr Han’s report.1
US Injury Costs Topped $671 Billion in 2013
By Richard Franki
From MMWR
Over 30 million injuries were treated in US EDs in 2013, costing an estimated $671 billion, the CDC reported.
The largest share of that cost—almost $290 billion, or about 43%—came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from EDs were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, PhD, of the CDC’s National Center for Injury Prevention and Control, Atlanta, Georgia, and associates.
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said.1
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr Florence and associates noted.
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.
Peramivir Effective Against Most Flu Viruses Circulating Globally
By Doug Brunk
AT ICAAC 2015
Vitals Key clinical point: Peramivir is potently effective against seasonal influenza viruses circulating globally. Major finding: During the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir. Data source: An analysis of 8,426 influenza viruses that were tested during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System.1 Disclosures: The researchers reporting having no financial disclosures. |
SAN DIEGO – The neuraminidase inhibitor peramivir inhibited about 99% of seasonal influenza A and B viruses circulating globally during the 2013 to 2014 and 2014 to 2015 influenza seasons, a large analysis demonstrated.
“The frequency of H1N1pdm09 viruses carrying neuraminidase (NA) H275Y remained low during both seasons; this mutation confers resistance to oseltamivir and peramivir,” said Margaret Okomo-Adhiambo, PhD, at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC/ICC 2015). In addition, “a small proportion of viruses contained other neuraminidase changes that affect binding of peramivir to viral enzymes and may decrease virus susceptibility. These changes need to be closely monitored.”
Approved by the FDA in December of 2014, peramivir (Rapivab) is the only antiviral agent for influenza treatment to come to market in nearly 20 years. Approved for intravenous administration as a single dose, it is indicated for adults with acute uncomplicated influenza who may have trouble taking orally administered or inhaled neuraminidase (NA) inhibitors. Other NA inhibitors approved by the FDA for influenza infection include oseltamivir, which is orally administered, and zanamivir, which is inhaled.
For the current analysis, Dr Okomo-Adhiambo of the influenza division at the US Centers for Disease Control and Prevention (CDC), Atlanta, and her associates tested influenza virus susceptibility to peramivir during the 2013-2014 and 2014-2015 influenza seasons as part of the World Health Organization Global Influenza Surveillance and Response System. A total of 8,426 viruses were tested, 75% of which were circulating in the United States.1
Dr Okomo-Adhiambo reported that during the 2013-2014 and 2014-2015 influenza seasons, about 99% of influenza type A and B viruses were inhibited by peramivir, except for a few viruses belonging to subtype A(H1N1)pdm09 (1.5%), subtype A(H3N2) (0.2%), and type B (0.4%). In addition, NA activity of type A viruses was five to six times more sensitive to inhibition by peramivir, compared with type B NA.
Parasitic Infection Emerging in the Southwestern United States
By Doug Brunk
At IDWEEK 2015
Vitals Key clinical point: Lesions containing a zoonotic parasite known as Onchocerca lupi are appearing in humans who reside in the Southwestern United States. Major finding: In three of six human cases, nodules containing Onchocerca lupi were located in the cervical spinal canal. Data source: A case report of the first six people in the United States to be infected with Onchocerca lupi. Disclosures: The researchers reported having no financial disclosures. |
SAN DIEGO – Onchocerca lupi, a zoonotic parasite previously described as causing eye disease in cats and dogs, as well as in humans from Europe, Asia, and the Middle East, is emerging in the Southwestern United States.
“The life cycle of this organism is not yet clearly defined, but likely includes a canine and/or feline animal reservoir, as well as an insect vector,” Dr Christiana Smith said in an interview at an annual scientific meeting on infectious diseases.1 “No specific risk factors for developing this disease have been identified, other than residing in or traveling through the Southwestern US.”
To date, six cases of humans infected by Onchocerca lupi have come to the attention of health officials, including those at the CDC, due to symptoms from a nodule containing the parasite, according to Dr Smith, a pediatrician with the University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora. The affected patients range in age from 22 months to 50 years of age; three of the six reside in Arizona, two in New Mexico, and one in Texas.
In three of the six cases, the nodule was located in the cervical spinal canal. In the remaining three cases, nodules were located on the scalp, the forearm, and the superior rectus muscle of the orbit. Two of the patients reported insect bites at the nodule site years prior to presentation, while another patient owned a dog with eye lesions.
“No previous Onchocerca parasites are known to have tropism for the central nervous system,” Dr Smith said. “In addition, five of the six cases presented in children. It is not clear whether children are disproportionately affected by this disease, or whether they are diagnosed more frequently.”
Treatment included surgical excision and antiparasitic treatment for most cases. To date, all patients have remained asymptomatic following treatment. Dr Smith said that more information about Onchocerca lupi will become available as additional cases are described. “Continued epidemiologic investigation will help define the life cycle of this organism, describe the spectrum of human disease, develop approaches to diagnosis and management, and design prevention strategies,” she said.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
Europeans Adopt 1-Hour ED Chest Pain Triage
By Bruce Jancin
At the ESC Congress 2015
LONDON – The positive findings of the Biomarkers in Acute Cardiovascular Care (BACC) study1 reinforce a key change contained in the brand-new European Society of Cardiology guidelines for management of patients with acute coronary syndrome without ST-segment elevation: namely, that it’s appropriate to assess such patients using two measurements of a validated high-sensitivity cardiac troponin assay taken just 1 hour apart, according to Dr Kurt Huber.
The BACC results are the evidence-based icing on the cake in support of the new recommendation in the guidelines, released at the annual congress of the European Society of Cardiology. The BACC study, which included 1,045 patients who presented to a university ED with acute chest pain suggestive of an acute coronary syndrome without ST-segment elevation, was the latest of several studies to show that most such patients can either be safely sent home from the ED or ruled-in for acute MI in just 1 hour when evaluated using a high-sensitivity troponin assay backed by a validated patient-management algorithm. The result means reduced pressure on overcrowded EDs and less patient anxiety because of delayed diagnosis, Dr Huber, director of cardiology and emergency medicine at Wilhelminen Hospital in Vienna, observed during an interview at the meeting.
The BACC study, presented by Dr Dirk Westermann of the University Heart Center Hamburg (Germany), utilized a high-sensitivity cardiac troponin I assay. The 1-hour algorithm had a 99.7% negative predictive value for acute MI. A total of 53% of patients were ruled out or in for MI at the 1-hour mark; the rest required further evaluation.2
To view the video, search “Huber” at http://www.emed-journal.com/
- New CPR Guide Sets Compression Limits, Scratches Vasopressin
- Bhanji F, Donoghue AJ, Wolff MS, et al. Part 14: Education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S561-S573.
- Cave DM, Gazmuri RJ, Otto CW, et al. Part 7: CPR techniques and devices: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S720-S728.
- Complex Picture Emerges of Prescription Opioid Abuse
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468-1478.
- Nelson LS, Juurlink DN, Perrone J. Addressing the opioid epidemic. JAMA. 2015;314(14):1453-1454.
- Severtson SG, Bartelson BB, Davis JM, et al. Reduced abuse, therapeutic errors, and diversion following reformulation of extended-release ocycodone in 2010. J Pain. 2013;14(10):1122-1130.
- US Injury Costs Topped $671 Billion in 2013
- Florence C, Simon T, Haegerich T, Luo F, Zhou C. Estimated lifetime medical and work-loss costs of fatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;46(38):1074-1077.
- Florence C, Haegerich T, Simon T, Zhou C, Luo F. Estimated lifetime medical and work-loss costs of emergency department-treated nonfatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(38):1078-1082.
- Peramivir Effective Against Most Flu Viruses Circulating Globally
- Okomo-Adhiambo M, Daniels J, Nguyen HT, et al. Peramivir Susceptibility Surveillance of Influenza A and B Viruses Circulated Globally, 2013-2015. Presented at: Interscience Conference of Antimicrobial Agents and Chemotherapy (ICAAC) and the International Society of Chemotherapy (ISC)’s International Congress of Chemotherapy and Infection (ICC) 2015; September 17-21, 2015; San Diego, California
- Parasitic Infection Emerging in the Southwestern United States
- Smith C, Rao S, Dehority W, et al. Onchocerca lupi: An Emerging Parasitic Infection in the Southwestern United States. Poster presented at: Infectious Disease (ID) Week 2015; October 7-11, 2015; San Diego, California; Abstract 1971.
- Europeans Adopt 1-Hour ED Chest Pain Triage
- Universitätsklinikum Hamburg-Eppendorf. Biomarkers in Acute Cardiac Care (BACC). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02355457. NLM Identifier: NCT02355457.
- Westermann D. Accurate and rapid diagnosis of myocardial infarction using a high sensitivity Troponin I 1-hour algorithm. Presented at: European Society of Cardiology (ESC) Congress; August 29 - September 2, 2015; London, England. FP NR 1161.
- New CPR Guide Sets Compression Limits, Scratches Vasopressin
- Bhanji F, Donoghue AJ, Wolff MS, et al. Part 14: Education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S561-S573.
- Cave DM, Gazmuri RJ, Otto CW, et al. Part 7: CPR techniques and devices: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S720-S728.
- Complex Picture Emerges of Prescription Opioid Abuse
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468-1478.
- Nelson LS, Juurlink DN, Perrone J. Addressing the opioid epidemic. JAMA. 2015;314(14):1453-1454.
- Severtson SG, Bartelson BB, Davis JM, et al. Reduced abuse, therapeutic errors, and diversion following reformulation of extended-release ocycodone in 2010. J Pain. 2013;14(10):1122-1130.
- US Injury Costs Topped $671 Billion in 2013
- Florence C, Simon T, Haegerich T, Luo F, Zhou C. Estimated lifetime medical and work-loss costs of fatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;46(38):1074-1077.
- Florence C, Haegerich T, Simon T, Zhou C, Luo F. Estimated lifetime medical and work-loss costs of emergency department-treated nonfatal injuries – United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(38):1078-1082.
- Peramivir Effective Against Most Flu Viruses Circulating Globally
- Okomo-Adhiambo M, Daniels J, Nguyen HT, et al. Peramivir Susceptibility Surveillance of Influenza A and B Viruses Circulated Globally, 2013-2015. Presented at: Interscience Conference of Antimicrobial Agents and Chemotherapy (ICAAC) and the International Society of Chemotherapy (ISC)’s International Congress of Chemotherapy and Infection (ICC) 2015; September 17-21, 2015; San Diego, California
- Parasitic Infection Emerging in the Southwestern United States
- Smith C, Rao S, Dehority W, et al. Onchocerca lupi: An Emerging Parasitic Infection in the Southwestern United States. Poster presented at: Infectious Disease (ID) Week 2015; October 7-11, 2015; San Diego, California; Abstract 1971.
- Europeans Adopt 1-Hour ED Chest Pain Triage
- Universitätsklinikum Hamburg-Eppendorf. Biomarkers in Acute Cardiac Care (BACC). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02355457. NLM Identifier: NCT02355457.
- Westermann D. Accurate and rapid diagnosis of myocardial infarction using a high sensitivity Troponin I 1-hour algorithm. Presented at: European Society of Cardiology (ESC) Congress; August 29 - September 2, 2015; London, England. FP NR 1161.