User login
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
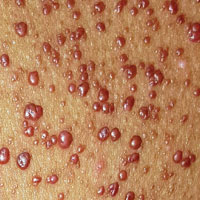
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.
ANSWER
The correct diagnosis in this case is juvenile xanthogranuloma (JXG; choice “d”).
Anderson-Fabry disease (choice “a”) is a rare inherited disorder characterized by widespread red papules; these lesions, however, are much smaller and far more widespread than those of JXG.
Considered a possibility at initial presentation, molluscum contagiosum (choice “b”) was quickly ruled out upon further inspection. This patient’s condition lacked the typical features of molluscum: umbilicated, white, firm papules caused by a pox virus.
Eruptive xanthomata (choice “c”) is a collection of lipid-laden macrophages caused by hypertriglyceridemia. They present as papules and nodules under, rather than on, the skin.
DISCUSSION
Solitary JXG lesions are fairly common, developing on the trunk, face, or extremities as smooth, reddish brown to cream papules. Typically, they cause no problems—but when multiple lesions manifest at birth, the condition can affect the eye (especially the iris, as in this case).
JXG is considered a form of histiocytosis, specifically classified as a type II non-Langerhans cell-mediated lesion. It is believed to result from a disordered macrophage response to a nonspecific tissue injury, which leads to a distinct variety of granulomatous change. These lesions are part of a spectrum of related conditions that also includes Langerhans cell histiocytosis.
No perfect treatment exists for this patient’s multitudinous skin lesions, because her darker skin could easily be permanently changed by burning, freezing, laser, or other destructive modality. Fair or not, in many cases, insurance coverage (or lack thereof) ultimately dictates what treatment is used.
Once the biopsy confirmed the diagnosis and effectively ruled out the other items in the differential, she was referred to ophthalmology for ongoing care of her eyes. Beyond that, she’ll need an annual physical with labs, because JXG is known to affect internal organs as well.
Since shortly after birth, a now 12-year-old African-American girl has had lesions on her trunk. She has never been given a diagnosis and has always been told she would “outgrow the problem.” Instead, the number and distribution of lesions continues to increase, and her pediatrician finally refers her to dermatology for evaluation.
About 150 to 200 nearly identical lesions scatter around the patient’s body, clustered mostly on the left upper back but also on the abdomen and bilateral upper thighs. The fleshy, reddish brown, mushroom-like papules range in size from 2 to 4 mm and exhibit no central umbilication. Two brown spots (each measuring 2 mm) are seen in the iris of the patient’s left eye.
There are no other apparent medical problems to report and no visual deficits. Aside from being unsightly, the lesions are asymptomatic. A shave biopsy of one of them is performed.