User login
An 8-Year-Old Male With Asymptomatic Brown Rough Plaques on the Dorsum of the Right Hand and Fingers, Accompanied by Widening of the Knuckles
During examination, the patient was observed repetitively cracking his knuckles, making a fist with the right hand, placing the left hand on top, and rubbing the hand, a behavior he routinely did multiple times daily. The observed pattern of finger involvement on the dorsum of the right hand corresponded to areas subjected to significant pressure during the described activity. Consequently, a diagnosis of lichen simplex chronicus (LSC) secondary to mechanical rubbing, along with associated pachydermodactyly on the fingers of the right hand, was established.
Lichen simplex chronicus and pachydermodactyly are both attributed to microtrauma inflicted upon the skin. Lichen simplex chronicus often constitutes a diagnosis of exclusion and is characterized by repetitive trauma-induced keratinocyte proliferation and melanocyte activation, resulting in hyperpigmentation and skin thickening. Although typically observed in women between the fourth and fifth decades of life, LSC is rarely reported in children. In adults, LSC-related rubbing or scratching frequently arises from chronic pruritic dermatitis such as eczema or psoriasis, neurodermatitis from dysesthesia, or habitual movements, as exhibited by this young patient. While generally benign, LSC may become infected. In rare instances, malignant transformation may occur.
The association with pachydermodactyly implicates microtrauma, necessitating careful observation and questioning to elucidate the cause, as demonstrated in this case. Lesions are typically hyperpigmented, though cases of associated hypopigmentation or depigmentation have been documented. Affected areas typically fall within the patient’s hand and finger reach, with lesion improvement over several months achievable through trigger avoidance.
Pachydermodactyly, a rare but benign fibromatosis around the proximal interphalangeal joints, is often misdiagnosed as juvenile idiopathic arthritis, potentially leading to unnecessary treatments and patient anxiety. Microtrauma history due to digit manipulation is prevalent among affected individuals, with most also exhibiting neuropsychiatric disorders. Histological examination of pachydermodactyly reveals hypergranulosis and dermal thickening, accompanied by increased fibroblasts and collagen types I, III, and V, differing from the epidermal changes seen in LSC.
The differential diagnosis also included phytophotodermatitis, a phototoxic dermatologic reaction following exposure to ultraviolet light subsequent to contact with furocoumarin-containing plant chemicals. However, the persistence of the patient’s lesions for over a year precluded this diagnosis. Secondary hyperpigmentation was also contemplated but excluded due to the absence of preceding inflammatory dermatitis.
Treatment of LSC primarily involves identifying and addressing any underlying conditions, repairing the skin barrier, reducing inflammation, and modifying behaviors contributing to chronic microtrauma, as observed in this patient. Topical corticosteroids may aid in decreasing epidermal thickening and discoloration, though lesion resolution necessitates behavior cessation.
It’s important to identify these types of skin changes in children to avoid unnecessary medical treatments for these benign conditions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Seier JA, Dissemond J. Lichen Simplex Chronicus Due to Mechanical Irritation. Dtsch Arztebl Int. 2022 Nov 18;119(46):802. doi: 10.3238/arztebl.m2022.0213.
Small S et al. A 12-Year-Old Boy Presenting With Unilateral Proximal Interphalangeal Joint Swelling. BMJ Case Rep. 2011 Apr 13:2011:bcr0120113719. doi: 10.1136/bcr.01.2011.3719.
Voicu C et al Lichen Simplex Chronicus as an Essential Part of the Dermatologic Masquerade. Open Access Maced J Med Sci. 2017 Jul 24;5(4):556-557. doi: 10.3889/oamjms.2017.133.
During examination, the patient was observed repetitively cracking his knuckles, making a fist with the right hand, placing the left hand on top, and rubbing the hand, a behavior he routinely did multiple times daily. The observed pattern of finger involvement on the dorsum of the right hand corresponded to areas subjected to significant pressure during the described activity. Consequently, a diagnosis of lichen simplex chronicus (LSC) secondary to mechanical rubbing, along with associated pachydermodactyly on the fingers of the right hand, was established.
Lichen simplex chronicus and pachydermodactyly are both attributed to microtrauma inflicted upon the skin. Lichen simplex chronicus often constitutes a diagnosis of exclusion and is characterized by repetitive trauma-induced keratinocyte proliferation and melanocyte activation, resulting in hyperpigmentation and skin thickening. Although typically observed in women between the fourth and fifth decades of life, LSC is rarely reported in children. In adults, LSC-related rubbing or scratching frequently arises from chronic pruritic dermatitis such as eczema or psoriasis, neurodermatitis from dysesthesia, or habitual movements, as exhibited by this young patient. While generally benign, LSC may become infected. In rare instances, malignant transformation may occur.
The association with pachydermodactyly implicates microtrauma, necessitating careful observation and questioning to elucidate the cause, as demonstrated in this case. Lesions are typically hyperpigmented, though cases of associated hypopigmentation or depigmentation have been documented. Affected areas typically fall within the patient’s hand and finger reach, with lesion improvement over several months achievable through trigger avoidance.
Pachydermodactyly, a rare but benign fibromatosis around the proximal interphalangeal joints, is often misdiagnosed as juvenile idiopathic arthritis, potentially leading to unnecessary treatments and patient anxiety. Microtrauma history due to digit manipulation is prevalent among affected individuals, with most also exhibiting neuropsychiatric disorders. Histological examination of pachydermodactyly reveals hypergranulosis and dermal thickening, accompanied by increased fibroblasts and collagen types I, III, and V, differing from the epidermal changes seen in LSC.
The differential diagnosis also included phytophotodermatitis, a phototoxic dermatologic reaction following exposure to ultraviolet light subsequent to contact with furocoumarin-containing plant chemicals. However, the persistence of the patient’s lesions for over a year precluded this diagnosis. Secondary hyperpigmentation was also contemplated but excluded due to the absence of preceding inflammatory dermatitis.
Treatment of LSC primarily involves identifying and addressing any underlying conditions, repairing the skin barrier, reducing inflammation, and modifying behaviors contributing to chronic microtrauma, as observed in this patient. Topical corticosteroids may aid in decreasing epidermal thickening and discoloration, though lesion resolution necessitates behavior cessation.
It’s important to identify these types of skin changes in children to avoid unnecessary medical treatments for these benign conditions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Seier JA, Dissemond J. Lichen Simplex Chronicus Due to Mechanical Irritation. Dtsch Arztebl Int. 2022 Nov 18;119(46):802. doi: 10.3238/arztebl.m2022.0213.
Small S et al. A 12-Year-Old Boy Presenting With Unilateral Proximal Interphalangeal Joint Swelling. BMJ Case Rep. 2011 Apr 13:2011:bcr0120113719. doi: 10.1136/bcr.01.2011.3719.
Voicu C et al Lichen Simplex Chronicus as an Essential Part of the Dermatologic Masquerade. Open Access Maced J Med Sci. 2017 Jul 24;5(4):556-557. doi: 10.3889/oamjms.2017.133.
During examination, the patient was observed repetitively cracking his knuckles, making a fist with the right hand, placing the left hand on top, and rubbing the hand, a behavior he routinely did multiple times daily. The observed pattern of finger involvement on the dorsum of the right hand corresponded to areas subjected to significant pressure during the described activity. Consequently, a diagnosis of lichen simplex chronicus (LSC) secondary to mechanical rubbing, along with associated pachydermodactyly on the fingers of the right hand, was established.
Lichen simplex chronicus and pachydermodactyly are both attributed to microtrauma inflicted upon the skin. Lichen simplex chronicus often constitutes a diagnosis of exclusion and is characterized by repetitive trauma-induced keratinocyte proliferation and melanocyte activation, resulting in hyperpigmentation and skin thickening. Although typically observed in women between the fourth and fifth decades of life, LSC is rarely reported in children. In adults, LSC-related rubbing or scratching frequently arises from chronic pruritic dermatitis such as eczema or psoriasis, neurodermatitis from dysesthesia, or habitual movements, as exhibited by this young patient. While generally benign, LSC may become infected. In rare instances, malignant transformation may occur.
The association with pachydermodactyly implicates microtrauma, necessitating careful observation and questioning to elucidate the cause, as demonstrated in this case. Lesions are typically hyperpigmented, though cases of associated hypopigmentation or depigmentation have been documented. Affected areas typically fall within the patient’s hand and finger reach, with lesion improvement over several months achievable through trigger avoidance.
Pachydermodactyly, a rare but benign fibromatosis around the proximal interphalangeal joints, is often misdiagnosed as juvenile idiopathic arthritis, potentially leading to unnecessary treatments and patient anxiety. Microtrauma history due to digit manipulation is prevalent among affected individuals, with most also exhibiting neuropsychiatric disorders. Histological examination of pachydermodactyly reveals hypergranulosis and dermal thickening, accompanied by increased fibroblasts and collagen types I, III, and V, differing from the epidermal changes seen in LSC.
The differential diagnosis also included phytophotodermatitis, a phototoxic dermatologic reaction following exposure to ultraviolet light subsequent to contact with furocoumarin-containing plant chemicals. However, the persistence of the patient’s lesions for over a year precluded this diagnosis. Secondary hyperpigmentation was also contemplated but excluded due to the absence of preceding inflammatory dermatitis.
Treatment of LSC primarily involves identifying and addressing any underlying conditions, repairing the skin barrier, reducing inflammation, and modifying behaviors contributing to chronic microtrauma, as observed in this patient. Topical corticosteroids may aid in decreasing epidermal thickening and discoloration, though lesion resolution necessitates behavior cessation.
It’s important to identify these types of skin changes in children to avoid unnecessary medical treatments for these benign conditions.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Seier JA, Dissemond J. Lichen Simplex Chronicus Due to Mechanical Irritation. Dtsch Arztebl Int. 2022 Nov 18;119(46):802. doi: 10.3238/arztebl.m2022.0213.
Small S et al. A 12-Year-Old Boy Presenting With Unilateral Proximal Interphalangeal Joint Swelling. BMJ Case Rep. 2011 Apr 13:2011:bcr0120113719. doi: 10.1136/bcr.01.2011.3719.
Voicu C et al Lichen Simplex Chronicus as an Essential Part of the Dermatologic Masquerade. Open Access Maced J Med Sci. 2017 Jul 24;5(4):556-557. doi: 10.3889/oamjms.2017.133.
The patient was otherwise healthy, with no current medication intake, and he engaged in baseball and soccer activities. Upon physical examination, a hyperpigmented lichenified irregular plaque was observed on the dorsum of the right hand, along with irregular hyperpigmented macules and plaques on the fingers. Fusiform widening of the interphalangeal joints on the second, third, and fourth fingers of the right hand was noted, without associated pain, edema, or erythema.
Do you agree with recent authors that patient satisfaction questionnaires should be modified to account for inherent societal biases, such as gender inequality and racism, to improve patient feedback?
[polldaddy:12782738]
[polldaddy:12782738]
[polldaddy:12782738]
When having discussions with your patients about recommended cancer screenings, have you been asked to answer questions related to liquid biopsy technology?
[polldaddy:11991465]
[polldaddy:11991465]
[polldaddy:11991465]
Woman presents with cough and bronchorrhea
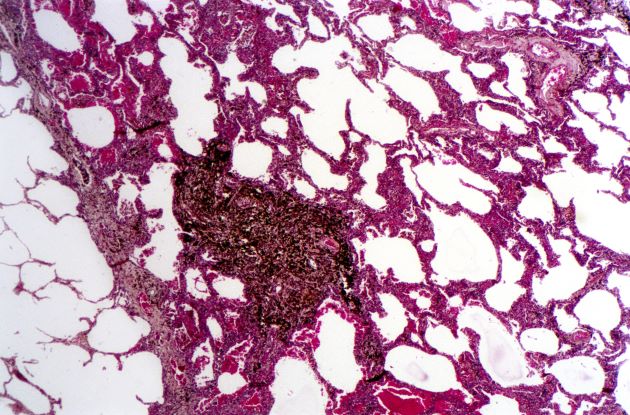
Bronchioalveolar cell carcinoma (BAC) is a variant of non–small cell lung cancer (NSCLC) that, in recent years, has received a new identity in some of the literature. Adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) are relatively new entities that in some published literature have replaced the term BAC. The National Comprehensive Cancer Network recognizes these terms. AIS is defined as a localized adenocarcinoma of < 3 cm that exhibits a lepidic growth pattern, with neoplastic cells along the alveolar structures but without stromal, vascular, or pleural invasion. MIA refers to small, solitary adenocarcinomas < 3 cm with either pure lepidic growth or predominant lepidic growth with ≤ 5 mm of stromal invasion. BAC has unique epidemiologic, pathologic, and clinical features compared with other NSCLC subtypes. For example, although it is smoking-related, the relationship of BAC to smoking is less strong than with other types of NSCLC. About a third of patients with BAC are never-smokers.
There are also some unique radiographic features — its presentation may be confused with pneumonia or other inflammatory conditions in the lung, and only after a patient does not improve after a course of antibiotics should a diagnosis of BAC be considered. Unlike other types of lung cancer where chemotherapy may be the first plan of attack, surgery is often the first choice for treating BAC, particularly when there is no mediastinal node involvement (10%-25% of cases) or distal metastases (5% of cases). BAC usually harbors EGFR mutation. It is responsive to new targeted therapies for lung cancer, particularly osimertinib, afatinib, erlotinib, and gefitinib. Thus, people with BAC are good candidates for genetic testing.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Bronchioalveolar cell carcinoma (BAC) is a variant of non–small cell lung cancer (NSCLC) that, in recent years, has received a new identity in some of the literature. Adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) are relatively new entities that in some published literature have replaced the term BAC. The National Comprehensive Cancer Network recognizes these terms. AIS is defined as a localized adenocarcinoma of < 3 cm that exhibits a lepidic growth pattern, with neoplastic cells along the alveolar structures but without stromal, vascular, or pleural invasion. MIA refers to small, solitary adenocarcinomas < 3 cm with either pure lepidic growth or predominant lepidic growth with ≤ 5 mm of stromal invasion. BAC has unique epidemiologic, pathologic, and clinical features compared with other NSCLC subtypes. For example, although it is smoking-related, the relationship of BAC to smoking is less strong than with other types of NSCLC. About a third of patients with BAC are never-smokers.
There are also some unique radiographic features — its presentation may be confused with pneumonia or other inflammatory conditions in the lung, and only after a patient does not improve after a course of antibiotics should a diagnosis of BAC be considered. Unlike other types of lung cancer where chemotherapy may be the first plan of attack, surgery is often the first choice for treating BAC, particularly when there is no mediastinal node involvement (10%-25% of cases) or distal metastases (5% of cases). BAC usually harbors EGFR mutation. It is responsive to new targeted therapies for lung cancer, particularly osimertinib, afatinib, erlotinib, and gefitinib. Thus, people with BAC are good candidates for genetic testing.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Bronchioalveolar cell carcinoma (BAC) is a variant of non–small cell lung cancer (NSCLC) that, in recent years, has received a new identity in some of the literature. Adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) are relatively new entities that in some published literature have replaced the term BAC. The National Comprehensive Cancer Network recognizes these terms. AIS is defined as a localized adenocarcinoma of < 3 cm that exhibits a lepidic growth pattern, with neoplastic cells along the alveolar structures but without stromal, vascular, or pleural invasion. MIA refers to small, solitary adenocarcinomas < 3 cm with either pure lepidic growth or predominant lepidic growth with ≤ 5 mm of stromal invasion. BAC has unique epidemiologic, pathologic, and clinical features compared with other NSCLC subtypes. For example, although it is smoking-related, the relationship of BAC to smoking is less strong than with other types of NSCLC. About a third of patients with BAC are never-smokers.
There are also some unique radiographic features — its presentation may be confused with pneumonia or other inflammatory conditions in the lung, and only after a patient does not improve after a course of antibiotics should a diagnosis of BAC be considered. Unlike other types of lung cancer where chemotherapy may be the first plan of attack, surgery is often the first choice for treating BAC, particularly when there is no mediastinal node involvement (10%-25% of cases) or distal metastases (5% of cases). BAC usually harbors EGFR mutation. It is responsive to new targeted therapies for lung cancer, particularly osimertinib, afatinib, erlotinib, and gefitinib. Thus, people with BAC are good candidates for genetic testing.
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
A 50-year-old woman, a never-smoker, presented with complaints of intermittent cough and shortness of breath for 3 months, associated with bronchorrhea (copious watery sputum production). She had lost 15 pounds in the past 2 months and had dyspnea on exertion for 1 month. Her pulse rate was 88/min, respiratory rate 18/min, and oxygen saturation 96% on room air. A chest x-ray (posteroanterior view) showed dense opacity in the right lower zone. Contrast-enhanced CT of the thorax showed diffuse ground-glass opacities around nodules and consolidation involving the apical and basal segments of the right lower lobe. Despite several courses of antimicrobials, bronchodilators, and IV corticosteroid therapy, the patient's condition worsened.
Question 2
Q2. Correct answer: A - No monitoring of PPI side effects.
Rationale
There are several putative risks associated with long-term PPI use: chronic kidney disease, dementia, vitamin and mineral deficiencies, and others. However, the overall quality of evidence to support these conclusions is low or very low, and the majority of the findings have low effect sizes that may be attributed to confounding. An American Gastroenterological Association clinical practice update recommended against routine monitoring for patients receiving long-term PPI treatment. However, data show that more than one-third of gastroenterologists still check for PPI side effects at least annually in their patients.
References
Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-Term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
Leiman DA, Ravi K, Freedberg DE, Gyawali CP. Proton Pump Inhibitor Prescribing and Monitoring Patterns Among Gastroenterology Practitioners (published online ahead of print, 2021 Oct 4). J Clin Gastroenterol. 2021;10.1097/MCG.0000000000001623. doi: 10.1097/MCG.0000000000001623.
Q2. Correct answer: A - No monitoring of PPI side effects.
Rationale
There are several putative risks associated with long-term PPI use: chronic kidney disease, dementia, vitamin and mineral deficiencies, and others. However, the overall quality of evidence to support these conclusions is low or very low, and the majority of the findings have low effect sizes that may be attributed to confounding. An American Gastroenterological Association clinical practice update recommended against routine monitoring for patients receiving long-term PPI treatment. However, data show that more than one-third of gastroenterologists still check for PPI side effects at least annually in their patients.
References
Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-Term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
Leiman DA, Ravi K, Freedberg DE, Gyawali CP. Proton Pump Inhibitor Prescribing and Monitoring Patterns Among Gastroenterology Practitioners (published online ahead of print, 2021 Oct 4). J Clin Gastroenterol. 2021;10.1097/MCG.0000000000001623. doi: 10.1097/MCG.0000000000001623.
Q2. Correct answer: A - No monitoring of PPI side effects.
Rationale
There are several putative risks associated with long-term PPI use: chronic kidney disease, dementia, vitamin and mineral deficiencies, and others. However, the overall quality of evidence to support these conclusions is low or very low, and the majority of the findings have low effect sizes that may be attributed to confounding. An American Gastroenterological Association clinical practice update recommended against routine monitoring for patients receiving long-term PPI treatment. However, data show that more than one-third of gastroenterologists still check for PPI side effects at least annually in their patients.
References
Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-Term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
Leiman DA, Ravi K, Freedberg DE, Gyawali CP. Proton Pump Inhibitor Prescribing and Monitoring Patterns Among Gastroenterology Practitioners (published online ahead of print, 2021 Oct 4). J Clin Gastroenterol. 2021;10.1097/MCG.0000000000001623. doi: 10.1097/MCG.0000000000001623.
Q2. A 76-year-old man with atrial fibrillation treated with long-term anticoagulation with warfarin and coronary artery disease treated with aspirin was recently admitted with melena. Upper endoscopy revealed a duodenal ulcer with visible vessel. Endoscopic therapy was performed, and he was started on twice-daily proton-pump inhibitors (PPIs).
Question 1
Q1. Correct answer: B - Adding calcium carbonate (antacid) to her current regimen
Rationale
Compared with proton pump inhibitors (PPIs), vonoprazan is a potassium-competitive acid blocker (PCAB), which inhibits acid secretion by competitively blocking availability of potassium to hydrogen-potassium ATPase. Vonoprazan is rapidly absorbed independent of eating and is not affected by CYP2C19 polymorphisms. Several studies have compared PPIs with vonoprazan. Although vonoprazan is highly effective for treating LA Grade A and B esophagitis, so is lansoprazole, and healing rates at 8 weeks are 100% versus 99.2%, respectively. In contrast, vonoprazan healing of LA Grade C and D esophagitis at 8 weeks is 98.7% compared with 87.5% for lansoprazole.
Sleeping on pillows is not a reliable way to reduce reflux, as patients often move during sleep and lose any benefit from being propped on them. Antacids would not provide superior acid inhibition, compared with vonoprazan, and avoiding spicy foods would not address the underlying permissive reflux barrier that exists (hiatal hernia).
Reference
Graham DY and Dore MP. Update on the Use of Vonoprazan: A Competitive Acid Blocker. Gastroenterology. 2018;154(3):462-6. doi: 10.1053/j.gastro.2018.01.018.
Q1. Correct answer: B - Adding calcium carbonate (antacid) to her current regimen
Rationale
Compared with proton pump inhibitors (PPIs), vonoprazan is a potassium-competitive acid blocker (PCAB), which inhibits acid secretion by competitively blocking availability of potassium to hydrogen-potassium ATPase. Vonoprazan is rapidly absorbed independent of eating and is not affected by CYP2C19 polymorphisms. Several studies have compared PPIs with vonoprazan. Although vonoprazan is highly effective for treating LA Grade A and B esophagitis, so is lansoprazole, and healing rates at 8 weeks are 100% versus 99.2%, respectively. In contrast, vonoprazan healing of LA Grade C and D esophagitis at 8 weeks is 98.7% compared with 87.5% for lansoprazole.
Sleeping on pillows is not a reliable way to reduce reflux, as patients often move during sleep and lose any benefit from being propped on them. Antacids would not provide superior acid inhibition, compared with vonoprazan, and avoiding spicy foods would not address the underlying permissive reflux barrier that exists (hiatal hernia).
Reference
Graham DY and Dore MP. Update on the Use of Vonoprazan: A Competitive Acid Blocker. Gastroenterology. 2018;154(3):462-6. doi: 10.1053/j.gastro.2018.01.018.
Q1. Correct answer: B - Adding calcium carbonate (antacid) to her current regimen
Rationale
Compared with proton pump inhibitors (PPIs), vonoprazan is a potassium-competitive acid blocker (PCAB), which inhibits acid secretion by competitively blocking availability of potassium to hydrogen-potassium ATPase. Vonoprazan is rapidly absorbed independent of eating and is not affected by CYP2C19 polymorphisms. Several studies have compared PPIs with vonoprazan. Although vonoprazan is highly effective for treating LA Grade A and B esophagitis, so is lansoprazole, and healing rates at 8 weeks are 100% versus 99.2%, respectively. In contrast, vonoprazan healing of LA Grade C and D esophagitis at 8 weeks is 98.7% compared with 87.5% for lansoprazole.
Sleeping on pillows is not a reliable way to reduce reflux, as patients often move during sleep and lose any benefit from being propped on them. Antacids would not provide superior acid inhibition, compared with vonoprazan, and avoiding spicy foods would not address the underlying permissive reflux barrier that exists (hiatal hernia).
Reference
Graham DY and Dore MP. Update on the Use of Vonoprazan: A Competitive Acid Blocker. Gastroenterology. 2018;154(3):462-6. doi: 10.1053/j.gastro.2018.01.018.
Q1. A 62-year-old woman with rheumatoid arthritis reports regurgitation, heartburn, and dysphagia. She undergoes upper endoscopy, which reveals a 3-cm hiatal hernia and Los Angeles (LA) Grade D esophagitis. Previously performed esophageal function tests revealed absent contractility and a total acid exposure time of 8.2%. Her thoracic surgeon is concerned about the postoperative risks of dysphagia with hernia repair; therefore, surgery is deferred. Although improved, she continues to have symptoms of heartburn with daily lansoprazole.
Quick Quiz Question 2
Q2. Correct answer: A. Enteric infection
Rationale
Despite the numerous side effects associated with long-term PPI use, the quality of evidence and risk of confounding from these studies limits the ability to ascribe sufficient cause and effect between PPI use and these outcomes. However, a recent large randomized controlled trial that evaluated the use of pantoprazole versus placebo demonstrated a statistically significant difference between the pantoprazole and placebo groups only in enteric infections (1.4% vs 1.0%; odds ratio, 1.33; 95% confidence interval, 1.01-1.75). Despite a nearly double increased risk of Clostridioides difficile infection in the PPI group, compared with the placebo group, the number of events was low, and the difference did not reach statistical significance. In the context of these data, and more recent studies suggesting an increased risk of COVID-19 in patients who take PPIs, compared with those who do not, the risk of enteric infections is likely small but significantly increased among long-term PPI users.
References
- Freedberg DE et al. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
- Moayyedi P et al. Gastroenterology. 2019;157(3):682-91.e2. doi: 10.1053/j.gastro.2019.05.056.
Q2. Correct answer: A. Enteric infection
Rationale
Despite the numerous side effects associated with long-term PPI use, the quality of evidence and risk of confounding from these studies limits the ability to ascribe sufficient cause and effect between PPI use and these outcomes. However, a recent large randomized controlled trial that evaluated the use of pantoprazole versus placebo demonstrated a statistically significant difference between the pantoprazole and placebo groups only in enteric infections (1.4% vs 1.0%; odds ratio, 1.33; 95% confidence interval, 1.01-1.75). Despite a nearly double increased risk of Clostridioides difficile infection in the PPI group, compared with the placebo group, the number of events was low, and the difference did not reach statistical significance. In the context of these data, and more recent studies suggesting an increased risk of COVID-19 in patients who take PPIs, compared with those who do not, the risk of enteric infections is likely small but significantly increased among long-term PPI users.
References
- Freedberg DE et al. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
- Moayyedi P et al. Gastroenterology. 2019;157(3):682-91.e2. doi: 10.1053/j.gastro.2019.05.056.
Q2. Correct answer: A. Enteric infection
Rationale
Despite the numerous side effects associated with long-term PPI use, the quality of evidence and risk of confounding from these studies limits the ability to ascribe sufficient cause and effect between PPI use and these outcomes. However, a recent large randomized controlled trial that evaluated the use of pantoprazole versus placebo demonstrated a statistically significant difference between the pantoprazole and placebo groups only in enteric infections (1.4% vs 1.0%; odds ratio, 1.33; 95% confidence interval, 1.01-1.75). Despite a nearly double increased risk of Clostridioides difficile infection in the PPI group, compared with the placebo group, the number of events was low, and the difference did not reach statistical significance. In the context of these data, and more recent studies suggesting an increased risk of COVID-19 in patients who take PPIs, compared with those who do not, the risk of enteric infections is likely small but significantly increased among long-term PPI users.
References
- Freedberg DE et al. Gastroenterology. 2017;152(4):706-15. doi: 10.1053/j.gastro.2017.01.031.
- Moayyedi P et al. Gastroenterology. 2019;157(3):682-91.e2. doi: 10.1053/j.gastro.2019.05.056.
.
Question 2
Correct answer: B. Selenium exposure.
Rationale
Helicobacter pylori infection is by far the most important risk factor for gastric cancer worldwide. Less common risk factors for gastric cancer include Lynch syndrome, Peutz-Jeghers syndrome, Menetrier's disease, and germline mutations in the CDH gene (encoding E-cadherin). However, there is some evidence that selenium, as well as high consumption of fruits and vegetables, may have protective effects against gastric cancer.
References
de Martel C et al. Gastroenterol Clin North Am. 2013 Jun;42(2):219-40.
Giardiello FM et al. N Engl J Med. 1987 Jun 11;316(24):1511-4.
Qiao YL et al. J Natl Cancer Inst. 2009 Apr 1;101(7):507-18.
Correct answer: B. Selenium exposure.
Rationale
Helicobacter pylori infection is by far the most important risk factor for gastric cancer worldwide. Less common risk factors for gastric cancer include Lynch syndrome, Peutz-Jeghers syndrome, Menetrier's disease, and germline mutations in the CDH gene (encoding E-cadherin). However, there is some evidence that selenium, as well as high consumption of fruits and vegetables, may have protective effects against gastric cancer.
References
de Martel C et al. Gastroenterol Clin North Am. 2013 Jun;42(2):219-40.
Giardiello FM et al. N Engl J Med. 1987 Jun 11;316(24):1511-4.
Qiao YL et al. J Natl Cancer Inst. 2009 Apr 1;101(7):507-18.
Correct answer: B. Selenium exposure.
Rationale
Helicobacter pylori infection is by far the most important risk factor for gastric cancer worldwide. Less common risk factors for gastric cancer include Lynch syndrome, Peutz-Jeghers syndrome, Menetrier's disease, and germline mutations in the CDH gene (encoding E-cadherin). However, there is some evidence that selenium, as well as high consumption of fruits and vegetables, may have protective effects against gastric cancer.
References
de Martel C et al. Gastroenterol Clin North Am. 2013 Jun;42(2):219-40.
Giardiello FM et al. N Engl J Med. 1987 Jun 11;316(24):1511-4.
Qiao YL et al. J Natl Cancer Inst. 2009 Apr 1;101(7):507-18.
.
Question 1
Correct answer: E. Cervical dysplasia.
Rationale
In a nationwide cohort study, women with Crohn's disease and ulcerative colitis were found to have an increased risk of cervical dysplasia. Patients with ulcerative colitis had increased risks of low- and high-grade squamous intraepithelial lesions, whereas patients with Crohn's disease also had increased risks of cervical cancer. Age-appropriate screening with pap smears is important for women diagnosed with inflammatory bowel disease regardless of treatment type.
Reference
Rungoe et al. Clin Gastroenterol Hepatol. 2015 Apr;13(4):693-700.e1.
Correct answer: E. Cervical dysplasia.
Rationale
In a nationwide cohort study, women with Crohn's disease and ulcerative colitis were found to have an increased risk of cervical dysplasia. Patients with ulcerative colitis had increased risks of low- and high-grade squamous intraepithelial lesions, whereas patients with Crohn's disease also had increased risks of cervical cancer. Age-appropriate screening with pap smears is important for women diagnosed with inflammatory bowel disease regardless of treatment type.
Reference
Rungoe et al. Clin Gastroenterol Hepatol. 2015 Apr;13(4):693-700.e1.
Correct answer: E. Cervical dysplasia.
Rationale
In a nationwide cohort study, women with Crohn's disease and ulcerative colitis were found to have an increased risk of cervical dysplasia. Patients with ulcerative colitis had increased risks of low- and high-grade squamous intraepithelial lesions, whereas patients with Crohn's disease also had increased risks of cervical cancer. Age-appropriate screening with pap smears is important for women diagnosed with inflammatory bowel disease regardless of treatment type.
Reference
Rungoe et al. Clin Gastroenterol Hepatol. 2015 Apr;13(4):693-700.e1.
Q1. A 25-year-old woman with colonic Crohn's disease presents for routine follow-up. She is in remission on her regimen of vedolizumab. When discussing her medication regimen, she asks about the long-term risks associated with her Crohn's disease and treatment.
Which of the following is a nonsurgical treatment for stress urinary incontinence?
[polldaddy:11216821]
[polldaddy:11216821]
[polldaddy:11216821]