User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Follow our continuing CROI coverage
Keep up to date with the Conference on Retroviruses and Opportunistic Infections home page for the latest in ID Practitioner's continuing reporting from the CROI meeting and our follow-ups afterward. You can also check out our archival coverage from last year's meeting.
Keep up to date with the Conference on Retroviruses and Opportunistic Infections home page for the latest in ID Practitioner's continuing reporting from the CROI meeting and our follow-ups afterward. You can also check out our archival coverage from last year's meeting.
Keep up to date with the Conference on Retroviruses and Opportunistic Infections home page for the latest in ID Practitioner's continuing reporting from the CROI meeting and our follow-ups afterward. You can also check out our archival coverage from last year's meeting.
Social Adversity Increases Mortality Risk in Patients With Pulmonary Hypertension
BOSTON — Social adversity is associated with worse survival among patients with pulmonary hypertension (PH), according to a new retrospective study of a New York City population.
A sub-analysis of both HIV+ and HIV– patients showed worse mortality outcomes with social adversity in both groups.
“Almost the majority of patients that we treat have either some social adversity or no insurance or are undocumented, so as a group of residents, we decided to study the impact of these factors on their health and the care that can be provided. We started using the two cohorts and now we keep it going with every new resident,” said Luca Biavati, MD, who presented the study at the CHEST Annual Meeting.
“The presence of any form of socioeconomic disadvantage is negatively impacting care and for a large part of the population, there are some factors that could probably be addressed by either an institutional or hospital policy,” said Dr. Biavati, who is an internal medicine resident at Jacobi Medical Center, New York.
Other factors are more difficult to address, such as lack of education. “[Some patients] don’t understand the gravity of their issue and medical condition until it’s too late, and then they’re not fit enough for the treatment, or just because of the social situation, they cannot qualify for advanced therapies,” said Dr. Biavati.
The researchers established two cohorts: One consisting of patients with HIV and heart failure who may or may not have had PH and one comprising patients with PH with or without HIV and heart failure. In the HIV/heart failure group, PH without social adversity was associated with a nearly threefold increase in all-cause mortality (hazard ratio [HR], 2.83; P = .004), whereas PH with social adversity was linked to a more than sevenfold increase in all-cause mortality (HR, 7.14; P < .001). Social adversity without PA was associated with a more than fourfold increase (HR, 4.47; P < .001).
Within the PH cohort, social adversity was associated with lower survival (P < .001). When the researchers broke down the results by types of social adversity, they found statistically significant relationships between greater mortality risk and economic instability within the HIV+ population (HR, 2.59; P = .040), transportation issues within the HIV– population (HR, 12.8; P < .001), and lack of social or family support within both the HIV– (HR, 5.49; P < .001) and the HIV+ population (HR, 2.03; P = .028).
The research has prompted interventions, which are now being studied at the institution, according to Dr. Biavati. “We have a policy of giving medications in bags when we discharge a patient with a social adversity. We literally go to the pharmacy, bring up the bag of medication, and we [put it] in their hands before they leave the hospital. They get a 1- or 3-month supply, depending on the medication, and then we usually discharge them with a clinical appointment already scheduled with either a pulmonary or primary care provider, and we usually call them before every appointment to confirm that they’re coming. That increases the chances of some success, but there’s still a very long way to go,” said Dr. Biavati.
Dr. Biavati was blinded to the results of the intervention, so he could not report on whether it was working. “But I can tell you that I’ve had busier clinics, so hopefully that means that they’re showing up more,” he said.
The problem is complex, according to Sandeep Jain, MD, who moderated the session. “Social adversity means lack of education. Lack of education means lack of compliance. Lack of compliance means what can you do if people are not taking medications? So it’s all matched together. It’s all lack of education and lack of money, lack of family support. And these drugs they have to take every single day. It’s not that easy. It’s very easy for us to say I had antiretroviral treatment for 6 months. It is almost impossible to continue regular treatment for that long [for a patient with social adversity]. You can’t blame them if they aren’t taking treatments. It’s very difficult for them,” said Dr. Jain.
That underscores the need for interventions that can address the needs of patients with social adversity. “We have to [practice] medicine considering the social situation of the patient and not just the medicine that we study in books. That’s kind of what we are faced with every day. We have therapies, and then life happens. It’s much harder to care for those patients,” said Dr. Biavati.
Dr. Biavati and Dr. Jain reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON — Social adversity is associated with worse survival among patients with pulmonary hypertension (PH), according to a new retrospective study of a New York City population.
A sub-analysis of both HIV+ and HIV– patients showed worse mortality outcomes with social adversity in both groups.
“Almost the majority of patients that we treat have either some social adversity or no insurance or are undocumented, so as a group of residents, we decided to study the impact of these factors on their health and the care that can be provided. We started using the two cohorts and now we keep it going with every new resident,” said Luca Biavati, MD, who presented the study at the CHEST Annual Meeting.
“The presence of any form of socioeconomic disadvantage is negatively impacting care and for a large part of the population, there are some factors that could probably be addressed by either an institutional or hospital policy,” said Dr. Biavati, who is an internal medicine resident at Jacobi Medical Center, New York.
Other factors are more difficult to address, such as lack of education. “[Some patients] don’t understand the gravity of their issue and medical condition until it’s too late, and then they’re not fit enough for the treatment, or just because of the social situation, they cannot qualify for advanced therapies,” said Dr. Biavati.
The researchers established two cohorts: One consisting of patients with HIV and heart failure who may or may not have had PH and one comprising patients with PH with or without HIV and heart failure. In the HIV/heart failure group, PH without social adversity was associated with a nearly threefold increase in all-cause mortality (hazard ratio [HR], 2.83; P = .004), whereas PH with social adversity was linked to a more than sevenfold increase in all-cause mortality (HR, 7.14; P < .001). Social adversity without PA was associated with a more than fourfold increase (HR, 4.47; P < .001).
Within the PH cohort, social adversity was associated with lower survival (P < .001). When the researchers broke down the results by types of social adversity, they found statistically significant relationships between greater mortality risk and economic instability within the HIV+ population (HR, 2.59; P = .040), transportation issues within the HIV– population (HR, 12.8; P < .001), and lack of social or family support within both the HIV– (HR, 5.49; P < .001) and the HIV+ population (HR, 2.03; P = .028).
The research has prompted interventions, which are now being studied at the institution, according to Dr. Biavati. “We have a policy of giving medications in bags when we discharge a patient with a social adversity. We literally go to the pharmacy, bring up the bag of medication, and we [put it] in their hands before they leave the hospital. They get a 1- or 3-month supply, depending on the medication, and then we usually discharge them with a clinical appointment already scheduled with either a pulmonary or primary care provider, and we usually call them before every appointment to confirm that they’re coming. That increases the chances of some success, but there’s still a very long way to go,” said Dr. Biavati.
Dr. Biavati was blinded to the results of the intervention, so he could not report on whether it was working. “But I can tell you that I’ve had busier clinics, so hopefully that means that they’re showing up more,” he said.
The problem is complex, according to Sandeep Jain, MD, who moderated the session. “Social adversity means lack of education. Lack of education means lack of compliance. Lack of compliance means what can you do if people are not taking medications? So it’s all matched together. It’s all lack of education and lack of money, lack of family support. And these drugs they have to take every single day. It’s not that easy. It’s very easy for us to say I had antiretroviral treatment for 6 months. It is almost impossible to continue regular treatment for that long [for a patient with social adversity]. You can’t blame them if they aren’t taking treatments. It’s very difficult for them,” said Dr. Jain.
That underscores the need for interventions that can address the needs of patients with social adversity. “We have to [practice] medicine considering the social situation of the patient and not just the medicine that we study in books. That’s kind of what we are faced with every day. We have therapies, and then life happens. It’s much harder to care for those patients,” said Dr. Biavati.
Dr. Biavati and Dr. Jain reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON — Social adversity is associated with worse survival among patients with pulmonary hypertension (PH), according to a new retrospective study of a New York City population.
A sub-analysis of both HIV+ and HIV– patients showed worse mortality outcomes with social adversity in both groups.
“Almost the majority of patients that we treat have either some social adversity or no insurance or are undocumented, so as a group of residents, we decided to study the impact of these factors on their health and the care that can be provided. We started using the two cohorts and now we keep it going with every new resident,” said Luca Biavati, MD, who presented the study at the CHEST Annual Meeting.
“The presence of any form of socioeconomic disadvantage is negatively impacting care and for a large part of the population, there are some factors that could probably be addressed by either an institutional or hospital policy,” said Dr. Biavati, who is an internal medicine resident at Jacobi Medical Center, New York.
Other factors are more difficult to address, such as lack of education. “[Some patients] don’t understand the gravity of their issue and medical condition until it’s too late, and then they’re not fit enough for the treatment, or just because of the social situation, they cannot qualify for advanced therapies,” said Dr. Biavati.
The researchers established two cohorts: One consisting of patients with HIV and heart failure who may or may not have had PH and one comprising patients with PH with or without HIV and heart failure. In the HIV/heart failure group, PH without social adversity was associated with a nearly threefold increase in all-cause mortality (hazard ratio [HR], 2.83; P = .004), whereas PH with social adversity was linked to a more than sevenfold increase in all-cause mortality (HR, 7.14; P < .001). Social adversity without PA was associated with a more than fourfold increase (HR, 4.47; P < .001).
Within the PH cohort, social adversity was associated with lower survival (P < .001). When the researchers broke down the results by types of social adversity, they found statistically significant relationships between greater mortality risk and economic instability within the HIV+ population (HR, 2.59; P = .040), transportation issues within the HIV– population (HR, 12.8; P < .001), and lack of social or family support within both the HIV– (HR, 5.49; P < .001) and the HIV+ population (HR, 2.03; P = .028).
The research has prompted interventions, which are now being studied at the institution, according to Dr. Biavati. “We have a policy of giving medications in bags when we discharge a patient with a social adversity. We literally go to the pharmacy, bring up the bag of medication, and we [put it] in their hands before they leave the hospital. They get a 1- or 3-month supply, depending on the medication, and then we usually discharge them with a clinical appointment already scheduled with either a pulmonary or primary care provider, and we usually call them before every appointment to confirm that they’re coming. That increases the chances of some success, but there’s still a very long way to go,” said Dr. Biavati.
Dr. Biavati was blinded to the results of the intervention, so he could not report on whether it was working. “But I can tell you that I’ve had busier clinics, so hopefully that means that they’re showing up more,” he said.
The problem is complex, according to Sandeep Jain, MD, who moderated the session. “Social adversity means lack of education. Lack of education means lack of compliance. Lack of compliance means what can you do if people are not taking medications? So it’s all matched together. It’s all lack of education and lack of money, lack of family support. And these drugs they have to take every single day. It’s not that easy. It’s very easy for us to say I had antiretroviral treatment for 6 months. It is almost impossible to continue regular treatment for that long [for a patient with social adversity]. You can’t blame them if they aren’t taking treatments. It’s very difficult for them,” said Dr. Jain.
That underscores the need for interventions that can address the needs of patients with social adversity. “We have to [practice] medicine considering the social situation of the patient and not just the medicine that we study in books. That’s kind of what we are faced with every day. We have therapies, and then life happens. It’s much harder to care for those patients,” said Dr. Biavati.
Dr. Biavati and Dr. Jain reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CHEST 2024
Metformin May Reduce Long COVID in Non-Diabetic Population
LOS ANGELES — , according to data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
Long COVID was determined by using the diagnostic code U09.9 or a computable phenotype based on symptoms and conditions. Most participants in this study were infected with the Omicron variant.
Researchers, led by Carolyn Bramante, MD, MPH, an internist, pediatrician, and obesity medicine specialist at the University of Minnesota Medical School in Minneapolis, simulated a randomized controlled trial of metformin vs control using the National COVID Cohort Collaborative (N3C) Electronic Health Record Database.
The intervention was a prescription for metformin within 6 days of SARS-CoV-2 infection. Those in the control group, which was designed to mimic placebo, had a prescription for fluvoxamine, fluticasone, ivermectin, or montelukast (all drugs that have been used off-label for COVID but have shown no effect on acute COVID outcomes in clinical trials). Exclusions included anyone with a previous metformin prescription or a comparator prescription; any indication for chronic metformin use; or a contraindication for metformin.
Why Study Metformin for Long COVID?
Dr. Bramante led a previous randomized controlled trial, COVID-OUT, with 1323 people that indicated metformin showed possible benefit for preventing the more severe components of COVID-19. She also led a 2020 review, in which she examined electronic health records from adults with type 2 diabetes or obesity. The researchers found that women taking metformin before they developed COVID-19 were significantly less likely to die after being hospitalized — although men didn’t see the same protective effect. Another randomized trial of 20 people found that 60% of those taking metformin vs 100% of those given a placebo had detectable SARS-CoV-2 viral load by day 4.
Other trials have highlighted the anti-inflammatory and antiviral properties of metformin. The existing evidence coupled with metformin’s well-established safety profile, led Dr. Bramante’s team to conduct the current simulated trial in people without diabetes or prediabetes. Dr. Bramante noted that metformin’s only US Food and Drug Administration–approved indication is for diabetes.
The current study featured a similar racial/ethnic makeup in the metformin and control groups: 16% and 17% were Black and 16% and 13% were Hispanic, respectively. Within 6 months, 4.0% in the metformin group developed long COVID or died compared with 8.5% in the control group (Relative Risk [RR], 0.47; 95% CI, 0.25-0.89). For prescriptions made on days 0-1 relative to infection, the RR was 0.39 (95% CI, 0.12-1.24). When metformin was prescribed on days 0-14, the RR was 0.75 (95% CI, 0.52-1.08).
The reason it’s important to have an active comparator is to control for things that can’t be measured, such as engagement in healthcare and the placebo effect, Dr. Bramante said.
Emily Erbelding, MD, MPH, director of the Division of Microbiology and Infectious Diseases at the National Institute of Allergy and Infectious Diseases, who was not part of the study, noted the potential implications of the findings.
Proven Safety and Low Cost of Metformin
“We don’t have therapies for long COVID, and we don’t know how to prevent it in people who have SARS-CoV-2 infections,” Dr. Erbelding noted. “This analysis points to metformin, a drug that millions of people have taken safely for their diabetes or their borderline diabetes. It’s licensed, it’s out there, and it’s inexpensive. The fact that we have data that point to this potentially being a therapy is important. I think that’s the power of this.”
Dr. Erbelding said a strength of the study is the size of the N3C Electronic Health Record Database (with data on nearly 9 million COVID cases) the researchers used to simulate the randomized controlled trial.
“(These results) gives us a reason to think about doing a large randomized controlled study with metformin,” she said. However, there are some limitations, she noted.
“The definition of long COVID may not have been applied exactly the same way across all the patients and you don’t know what led the prescribers to prescribe metformin. There might have been confounders that couldn’t be controlled for or weren’t evident in the way they approached the data.”
This study has “relatively rigorous methodology for an observational study,” Dr. Erbelding said. “It’s novel to try to simulate a randomized controlled trial through a large, observational, electronic record–based cohort. Maybe we should be doing more of this because these bioinformatic systems exist now. And we need to get all the public health use out of them that we can.”
“The fact that they may be unlocking something new here that needs follow-up in a truly randomized controlled trial is important as well because there are a lot of people out there suffering from long COVID.”
Bramante and Erbelding disclosed no relevant financial relationships. This research was supported in part by the intramural/extramural research program of the National Center for Advancing Translational Science, National Institutes of Health.
A version of this article appeared on Medscape.com.
LOS ANGELES — , according to data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
Long COVID was determined by using the diagnostic code U09.9 or a computable phenotype based on symptoms and conditions. Most participants in this study were infected with the Omicron variant.
Researchers, led by Carolyn Bramante, MD, MPH, an internist, pediatrician, and obesity medicine specialist at the University of Minnesota Medical School in Minneapolis, simulated a randomized controlled trial of metformin vs control using the National COVID Cohort Collaborative (N3C) Electronic Health Record Database.
The intervention was a prescription for metformin within 6 days of SARS-CoV-2 infection. Those in the control group, which was designed to mimic placebo, had a prescription for fluvoxamine, fluticasone, ivermectin, or montelukast (all drugs that have been used off-label for COVID but have shown no effect on acute COVID outcomes in clinical trials). Exclusions included anyone with a previous metformin prescription or a comparator prescription; any indication for chronic metformin use; or a contraindication for metformin.
Why Study Metformin for Long COVID?
Dr. Bramante led a previous randomized controlled trial, COVID-OUT, with 1323 people that indicated metformin showed possible benefit for preventing the more severe components of COVID-19. She also led a 2020 review, in which she examined electronic health records from adults with type 2 diabetes or obesity. The researchers found that women taking metformin before they developed COVID-19 were significantly less likely to die after being hospitalized — although men didn’t see the same protective effect. Another randomized trial of 20 people found that 60% of those taking metformin vs 100% of those given a placebo had detectable SARS-CoV-2 viral load by day 4.
Other trials have highlighted the anti-inflammatory and antiviral properties of metformin. The existing evidence coupled with metformin’s well-established safety profile, led Dr. Bramante’s team to conduct the current simulated trial in people without diabetes or prediabetes. Dr. Bramante noted that metformin’s only US Food and Drug Administration–approved indication is for diabetes.
The current study featured a similar racial/ethnic makeup in the metformin and control groups: 16% and 17% were Black and 16% and 13% were Hispanic, respectively. Within 6 months, 4.0% in the metformin group developed long COVID or died compared with 8.5% in the control group (Relative Risk [RR], 0.47; 95% CI, 0.25-0.89). For prescriptions made on days 0-1 relative to infection, the RR was 0.39 (95% CI, 0.12-1.24). When metformin was prescribed on days 0-14, the RR was 0.75 (95% CI, 0.52-1.08).
The reason it’s important to have an active comparator is to control for things that can’t be measured, such as engagement in healthcare and the placebo effect, Dr. Bramante said.
Emily Erbelding, MD, MPH, director of the Division of Microbiology and Infectious Diseases at the National Institute of Allergy and Infectious Diseases, who was not part of the study, noted the potential implications of the findings.
Proven Safety and Low Cost of Metformin
“We don’t have therapies for long COVID, and we don’t know how to prevent it in people who have SARS-CoV-2 infections,” Dr. Erbelding noted. “This analysis points to metformin, a drug that millions of people have taken safely for their diabetes or their borderline diabetes. It’s licensed, it’s out there, and it’s inexpensive. The fact that we have data that point to this potentially being a therapy is important. I think that’s the power of this.”
Dr. Erbelding said a strength of the study is the size of the N3C Electronic Health Record Database (with data on nearly 9 million COVID cases) the researchers used to simulate the randomized controlled trial.
“(These results) gives us a reason to think about doing a large randomized controlled study with metformin,” she said. However, there are some limitations, she noted.
“The definition of long COVID may not have been applied exactly the same way across all the patients and you don’t know what led the prescribers to prescribe metformin. There might have been confounders that couldn’t be controlled for or weren’t evident in the way they approached the data.”
This study has “relatively rigorous methodology for an observational study,” Dr. Erbelding said. “It’s novel to try to simulate a randomized controlled trial through a large, observational, electronic record–based cohort. Maybe we should be doing more of this because these bioinformatic systems exist now. And we need to get all the public health use out of them that we can.”
“The fact that they may be unlocking something new here that needs follow-up in a truly randomized controlled trial is important as well because there are a lot of people out there suffering from long COVID.”
Bramante and Erbelding disclosed no relevant financial relationships. This research was supported in part by the intramural/extramural research program of the National Center for Advancing Translational Science, National Institutes of Health.
A version of this article appeared on Medscape.com.
LOS ANGELES — , according to data presented at the Infectious Disease Week (IDWeek) 2024 Annual Meeting.
Long COVID was determined by using the diagnostic code U09.9 or a computable phenotype based on symptoms and conditions. Most participants in this study were infected with the Omicron variant.
Researchers, led by Carolyn Bramante, MD, MPH, an internist, pediatrician, and obesity medicine specialist at the University of Minnesota Medical School in Minneapolis, simulated a randomized controlled trial of metformin vs control using the National COVID Cohort Collaborative (N3C) Electronic Health Record Database.
The intervention was a prescription for metformin within 6 days of SARS-CoV-2 infection. Those in the control group, which was designed to mimic placebo, had a prescription for fluvoxamine, fluticasone, ivermectin, or montelukast (all drugs that have been used off-label for COVID but have shown no effect on acute COVID outcomes in clinical trials). Exclusions included anyone with a previous metformin prescription or a comparator prescription; any indication for chronic metformin use; or a contraindication for metformin.
Why Study Metformin for Long COVID?
Dr. Bramante led a previous randomized controlled trial, COVID-OUT, with 1323 people that indicated metformin showed possible benefit for preventing the more severe components of COVID-19. She also led a 2020 review, in which she examined electronic health records from adults with type 2 diabetes or obesity. The researchers found that women taking metformin before they developed COVID-19 were significantly less likely to die after being hospitalized — although men didn’t see the same protective effect. Another randomized trial of 20 people found that 60% of those taking metformin vs 100% of those given a placebo had detectable SARS-CoV-2 viral load by day 4.
Other trials have highlighted the anti-inflammatory and antiviral properties of metformin. The existing evidence coupled with metformin’s well-established safety profile, led Dr. Bramante’s team to conduct the current simulated trial in people without diabetes or prediabetes. Dr. Bramante noted that metformin’s only US Food and Drug Administration–approved indication is for diabetes.
The current study featured a similar racial/ethnic makeup in the metformin and control groups: 16% and 17% were Black and 16% and 13% were Hispanic, respectively. Within 6 months, 4.0% in the metformin group developed long COVID or died compared with 8.5% in the control group (Relative Risk [RR], 0.47; 95% CI, 0.25-0.89). For prescriptions made on days 0-1 relative to infection, the RR was 0.39 (95% CI, 0.12-1.24). When metformin was prescribed on days 0-14, the RR was 0.75 (95% CI, 0.52-1.08).
The reason it’s important to have an active comparator is to control for things that can’t be measured, such as engagement in healthcare and the placebo effect, Dr. Bramante said.
Emily Erbelding, MD, MPH, director of the Division of Microbiology and Infectious Diseases at the National Institute of Allergy and Infectious Diseases, who was not part of the study, noted the potential implications of the findings.
Proven Safety and Low Cost of Metformin
“We don’t have therapies for long COVID, and we don’t know how to prevent it in people who have SARS-CoV-2 infections,” Dr. Erbelding noted. “This analysis points to metformin, a drug that millions of people have taken safely for their diabetes or their borderline diabetes. It’s licensed, it’s out there, and it’s inexpensive. The fact that we have data that point to this potentially being a therapy is important. I think that’s the power of this.”
Dr. Erbelding said a strength of the study is the size of the N3C Electronic Health Record Database (with data on nearly 9 million COVID cases) the researchers used to simulate the randomized controlled trial.
“(These results) gives us a reason to think about doing a large randomized controlled study with metformin,” she said. However, there are some limitations, she noted.
“The definition of long COVID may not have been applied exactly the same way across all the patients and you don’t know what led the prescribers to prescribe metformin. There might have been confounders that couldn’t be controlled for or weren’t evident in the way they approached the data.”
This study has “relatively rigorous methodology for an observational study,” Dr. Erbelding said. “It’s novel to try to simulate a randomized controlled trial through a large, observational, electronic record–based cohort. Maybe we should be doing more of this because these bioinformatic systems exist now. And we need to get all the public health use out of them that we can.”
“The fact that they may be unlocking something new here that needs follow-up in a truly randomized controlled trial is important as well because there are a lot of people out there suffering from long COVID.”
Bramante and Erbelding disclosed no relevant financial relationships. This research was supported in part by the intramural/extramural research program of the National Center for Advancing Translational Science, National Institutes of Health.
A version of this article appeared on Medscape.com.
FROM IDWEEK 2024
Minor Progress in Gender Pay Equity, But a Big Gap Persists
Despite some recent progress in compensation equity, women in medicine continue to be paid significantly lower salaries than men.
According to the Female Compensation Report 2024 by Medscape, male doctors of any kind earned an average salary of about $400,000, whereas female doctors earned approximately $309,000 — a 29% gap.
The report analyzed survey data from 7000 practicing physicians who were recruited over a 4-month period starting in October 2023. The respondents comprised roughly 60% women representing over 29 specialties.
In the 2022 report, the pay gap between the genders was 32%. But some women in the field argued substantial headway is still needed.
“You can try and pick apart the data, but I’d say we’re not really making progress,” said Susan T. Hingle, MD, an internist in Illinois and president of the American Medical Women’s Association. “A decline by a couple of percentage points is not significantly addressing this pay gap that over a lifetime is huge, can be millions of dollars.”
The gender gap was narrower among female primary care physicians (PCPs) vs medical specialists. Female PCPs earned around $253,000 per year, whereas male PCPs earned about $295,000 per year. Hingle suggested that female PCPs may enjoy more pay equity because health systems have a harder time filling these positions.
On the other hand, the gap for specialists rose from 27% in 2022 to 31% in 2023. Differences in how aggressively women and men negotiate compensation packages may play a role, said Hingle.
“Taking negotiation out of the equation would be progress to me,” said Hingle.
Pay disparity did not appear to be the result of time spent on the job — female doctors reported an average of 49 work hours per week, whereas their male counterparts reported 50 work hours per week.
Meanwhile, the pay gap progressively worsened over time. Among doctors aged 28-34 years, men earned an average of $53,000 more than women. By ages 46-49, men earned an average of $157,000 more than women.
“I had to take my employer to court to get equal compensation, sad as it is to say,” said a hospitalist in North Carolina.
Nearly 60% of women surveyed felt they were not being paid fairly for their efforts, up from less than half reported in Medscape’s 2021 report. Hingle said that this figure may not only reflect sentiments about the compensation gap, but also less support on the job, including fewer physician assistants (PAs), nurses, and administrative staff.
“At my job, I do the work of multiple people,” said a survey respondent. “Junior resident, senior resident, social worker, nurse practitioner, PA — as well as try to be a teacher, researcher, [and] an excellent doctor and have the time to make patients feel as if they are not in a rush.”
Roughly 30% of women physicians said they would not choose to go into medicine again if given the chance compared with 26% of male physicians.
“Gender inequities in our profession have a direct impact,” said Shikha Jain, MD, an oncologist in Chicago and founder of the Women in Medicine nonprofit. “I think women in general don’t feel valued in the care they’re providing.”
Jain cited bullying, harassment, and fewer opportunities for leadership and recognition as factors beyond pay that affect female physicians’ feelings of being valued.
A version of this article first appeared on Medscape.com.
Despite some recent progress in compensation equity, women in medicine continue to be paid significantly lower salaries than men.
According to the Female Compensation Report 2024 by Medscape, male doctors of any kind earned an average salary of about $400,000, whereas female doctors earned approximately $309,000 — a 29% gap.
The report analyzed survey data from 7000 practicing physicians who were recruited over a 4-month period starting in October 2023. The respondents comprised roughly 60% women representing over 29 specialties.
In the 2022 report, the pay gap between the genders was 32%. But some women in the field argued substantial headway is still needed.
“You can try and pick apart the data, but I’d say we’re not really making progress,” said Susan T. Hingle, MD, an internist in Illinois and president of the American Medical Women’s Association. “A decline by a couple of percentage points is not significantly addressing this pay gap that over a lifetime is huge, can be millions of dollars.”
The gender gap was narrower among female primary care physicians (PCPs) vs medical specialists. Female PCPs earned around $253,000 per year, whereas male PCPs earned about $295,000 per year. Hingle suggested that female PCPs may enjoy more pay equity because health systems have a harder time filling these positions.
On the other hand, the gap for specialists rose from 27% in 2022 to 31% in 2023. Differences in how aggressively women and men negotiate compensation packages may play a role, said Hingle.
“Taking negotiation out of the equation would be progress to me,” said Hingle.
Pay disparity did not appear to be the result of time spent on the job — female doctors reported an average of 49 work hours per week, whereas their male counterparts reported 50 work hours per week.
Meanwhile, the pay gap progressively worsened over time. Among doctors aged 28-34 years, men earned an average of $53,000 more than women. By ages 46-49, men earned an average of $157,000 more than women.
“I had to take my employer to court to get equal compensation, sad as it is to say,” said a hospitalist in North Carolina.
Nearly 60% of women surveyed felt they were not being paid fairly for their efforts, up from less than half reported in Medscape’s 2021 report. Hingle said that this figure may not only reflect sentiments about the compensation gap, but also less support on the job, including fewer physician assistants (PAs), nurses, and administrative staff.
“At my job, I do the work of multiple people,” said a survey respondent. “Junior resident, senior resident, social worker, nurse practitioner, PA — as well as try to be a teacher, researcher, [and] an excellent doctor and have the time to make patients feel as if they are not in a rush.”
Roughly 30% of women physicians said they would not choose to go into medicine again if given the chance compared with 26% of male physicians.
“Gender inequities in our profession have a direct impact,” said Shikha Jain, MD, an oncologist in Chicago and founder of the Women in Medicine nonprofit. “I think women in general don’t feel valued in the care they’re providing.”
Jain cited bullying, harassment, and fewer opportunities for leadership and recognition as factors beyond pay that affect female physicians’ feelings of being valued.
A version of this article first appeared on Medscape.com.
Despite some recent progress in compensation equity, women in medicine continue to be paid significantly lower salaries than men.
According to the Female Compensation Report 2024 by Medscape, male doctors of any kind earned an average salary of about $400,000, whereas female doctors earned approximately $309,000 — a 29% gap.
The report analyzed survey data from 7000 practicing physicians who were recruited over a 4-month period starting in October 2023. The respondents comprised roughly 60% women representing over 29 specialties.
In the 2022 report, the pay gap between the genders was 32%. But some women in the field argued substantial headway is still needed.
“You can try and pick apart the data, but I’d say we’re not really making progress,” said Susan T. Hingle, MD, an internist in Illinois and president of the American Medical Women’s Association. “A decline by a couple of percentage points is not significantly addressing this pay gap that over a lifetime is huge, can be millions of dollars.”
The gender gap was narrower among female primary care physicians (PCPs) vs medical specialists. Female PCPs earned around $253,000 per year, whereas male PCPs earned about $295,000 per year. Hingle suggested that female PCPs may enjoy more pay equity because health systems have a harder time filling these positions.
On the other hand, the gap for specialists rose from 27% in 2022 to 31% in 2023. Differences in how aggressively women and men negotiate compensation packages may play a role, said Hingle.
“Taking negotiation out of the equation would be progress to me,” said Hingle.
Pay disparity did not appear to be the result of time spent on the job — female doctors reported an average of 49 work hours per week, whereas their male counterparts reported 50 work hours per week.
Meanwhile, the pay gap progressively worsened over time. Among doctors aged 28-34 years, men earned an average of $53,000 more than women. By ages 46-49, men earned an average of $157,000 more than women.
“I had to take my employer to court to get equal compensation, sad as it is to say,” said a hospitalist in North Carolina.
Nearly 60% of women surveyed felt they were not being paid fairly for their efforts, up from less than half reported in Medscape’s 2021 report. Hingle said that this figure may not only reflect sentiments about the compensation gap, but also less support on the job, including fewer physician assistants (PAs), nurses, and administrative staff.
“At my job, I do the work of multiple people,” said a survey respondent. “Junior resident, senior resident, social worker, nurse practitioner, PA — as well as try to be a teacher, researcher, [and] an excellent doctor and have the time to make patients feel as if they are not in a rush.”
Roughly 30% of women physicians said they would not choose to go into medicine again if given the chance compared with 26% of male physicians.
“Gender inequities in our profession have a direct impact,” said Shikha Jain, MD, an oncologist in Chicago and founder of the Women in Medicine nonprofit. “I think women in general don’t feel valued in the care they’re providing.”
Jain cited bullying, harassment, and fewer opportunities for leadership and recognition as factors beyond pay that affect female physicians’ feelings of being valued.
A version of this article first appeared on Medscape.com.
COVID on the Floor Linked to Outbreaks on Two Hospital Wards
The viral burden of SARS-CoV-2 on floors, even in healthcare worker–only areas, was strongly associated with COVID-19 outbreaks in two acute-care hospitals, according to a new study from Ontario, Canada.
With every 10-fold increase in viral copies, the chance of an impending outbreak of COVID-19 rose 22-fold.
“These data add to the mounting evidence that built environment detection for SARS-CoV-2 may provide an additional layer of monitoring and could help inform local infection prevention and control measures,” they wrote.
The study was published online in Infection Control & Hospital Epidemiology.
Preventing Future Suffering
The current study builds on the researchers’ previous work, which found the same correlation between viral load on floors and COVID outbreaks in long-term care homes.
Currently, the best-known method of environmental surveillance for COVID is wastewater detection. “Swabbing the floors would be another approach to surveillance,” senior author Caroline Nott, MD, infectious disease physician at the Ottawa Hospital, said in an interview.
“We do have environmental surveillance with wastewater, but while this may tell you what’s going on in the city, it doesn’t tell you what is going on in a particular ward of a hospital, for instance,” she added.
Nott and her colleagues believe that swabbing, which is easy and relatively inexpensive, will become another tool to examine the built environment. “Instead of having to close a whole hospital, for example, we could just close one room instead of an entire ward if swabbing showed a high concentration of COVID,” Nott said.
The current study was conducted at two hospitals in Ontario between July 2022 and March 2023. The floors of healthcare worker–only areas on four inpatient adult wards were swabbed. These areas included changing rooms, meeting rooms, staff washrooms, nursing stations, and interdisciplinary team rooms.
SARS-CoV-2 RNA was detected on 537 of 760 floor swabs (71%). The overall positivity rate in the first hospital was 90% (n = 280). In the second hospital, the rate was 60% (n = 480).
Four COVID-19 outbreaks occurred in the first acute care hospital, and seven outbreaks occurred at the second hospital. Outbreaks occurred mostly among hospitalized patients (140 cases), but also in four hospital workers.
COVID-19 still requires vigilance, said Nott. “We weren’t prepared for COVID, and so as a result, many people died or have suffered long-term effects, especially vulnerable people like those being treated in hospital or in long-term care facilities. We want to develop methods to prevent similar suffering in the future, whether it’s a new COVID variant or a different pathogen altogether.”
Changing Surveillance Practice?
“This is a good study,” Steven Rogak, PhD, professor of mechanical engineering at the University of British Columbia (UBC) in Vancouver, Canada, said in an interivew. “The fundamental idea is that respiratory droplets and aerosols will deposit on the floor, and polymerase chain reaction [PCR] tests of swabs will provide a surrogate measurement of what might have been inhaled. There are solid statistics that it worked for the hospitals studied,” said Rogak, who studies aerosols at UBC’s Energy and Aerosols Laboratory. Rogak did not participate in the study.
“The authors note several limitations, including that increased healthcare worker testing may have been triggered by the higher values of PCR counts from the floor swabs. But this doesn’t seem to be a problem to me, because if the floor swabs motivate the hospital to test workers more, and that results in identifying outbreaks sooner, then great,” he said.
“Another limitation is that if the hospital has better HVAC or uses air purifiers, it could remove the most infectious aerosols, but the large droplets that fall quickly to the ground would remain, and this would still result in high PCR counts from floor swabs. In this case, perhaps the floor swabs would be a poorer indication of impending outbreaks,” said Rogak.
Determining the best timing and location for floor swabbing might be challenging and specific to the particular hospital, he added. ”For example, you would not want to take swabs from floors right after they are cleaned. Overall, I think this method deserves further development, and it could become a standard technique, but the details might require refinement for widespread application.”
Adrian Popp, MD, chair of the Infectious Disease Service at Huntington Hospital–Northwell Health in New York, said that, although interesting, the study would not change his current practice.
“I’m going to start testing the environment in different rooms in the hospital, and yes, I might find different amounts of COVID, but what does that mean? If pieces of RNA from COVID are on the floor, the likelihood is that they’re not infectious,” Popp said in an interview.
“Hospital workers do get sick with COVID, and sometimes they are asymptomatic and come to work. Patients may come into the hospital for another reason and be sick with COVID. There are many ways people who work in the hospital, as well as the patients, can get COVID. To me, it means that in that hospital and community there is a lot of COVID, but I can’t tell if there is causation here. Who is giving COVID to whom? What am I supposed to do with the information?”
The study was supported by the Northern Ontario Academic Medicine Association Clinical Innovation Opportunities Fund, the Ottawa Hospital Academic Medical Organization Innovation Fund, and a Canadian Institutes of Health Research Operating Grant. One author was a consultant for ProofDx, a startup company creating a point-of-care diagnostic test for COVID-19, and is an advisor for SIGNAL1, a startup company deploying machine-learning models to improve inpatient care. Nott, Rogak, and Popp reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The viral burden of SARS-CoV-2 on floors, even in healthcare worker–only areas, was strongly associated with COVID-19 outbreaks in two acute-care hospitals, according to a new study from Ontario, Canada.
With every 10-fold increase in viral copies, the chance of an impending outbreak of COVID-19 rose 22-fold.
“These data add to the mounting evidence that built environment detection for SARS-CoV-2 may provide an additional layer of monitoring and could help inform local infection prevention and control measures,” they wrote.
The study was published online in Infection Control & Hospital Epidemiology.
Preventing Future Suffering
The current study builds on the researchers’ previous work, which found the same correlation between viral load on floors and COVID outbreaks in long-term care homes.
Currently, the best-known method of environmental surveillance for COVID is wastewater detection. “Swabbing the floors would be another approach to surveillance,” senior author Caroline Nott, MD, infectious disease physician at the Ottawa Hospital, said in an interview.
“We do have environmental surveillance with wastewater, but while this may tell you what’s going on in the city, it doesn’t tell you what is going on in a particular ward of a hospital, for instance,” she added.
Nott and her colleagues believe that swabbing, which is easy and relatively inexpensive, will become another tool to examine the built environment. “Instead of having to close a whole hospital, for example, we could just close one room instead of an entire ward if swabbing showed a high concentration of COVID,” Nott said.
The current study was conducted at two hospitals in Ontario between July 2022 and March 2023. The floors of healthcare worker–only areas on four inpatient adult wards were swabbed. These areas included changing rooms, meeting rooms, staff washrooms, nursing stations, and interdisciplinary team rooms.
SARS-CoV-2 RNA was detected on 537 of 760 floor swabs (71%). The overall positivity rate in the first hospital was 90% (n = 280). In the second hospital, the rate was 60% (n = 480).
Four COVID-19 outbreaks occurred in the first acute care hospital, and seven outbreaks occurred at the second hospital. Outbreaks occurred mostly among hospitalized patients (140 cases), but also in four hospital workers.
COVID-19 still requires vigilance, said Nott. “We weren’t prepared for COVID, and so as a result, many people died or have suffered long-term effects, especially vulnerable people like those being treated in hospital or in long-term care facilities. We want to develop methods to prevent similar suffering in the future, whether it’s a new COVID variant or a different pathogen altogether.”
Changing Surveillance Practice?
“This is a good study,” Steven Rogak, PhD, professor of mechanical engineering at the University of British Columbia (UBC) in Vancouver, Canada, said in an interivew. “The fundamental idea is that respiratory droplets and aerosols will deposit on the floor, and polymerase chain reaction [PCR] tests of swabs will provide a surrogate measurement of what might have been inhaled. There are solid statistics that it worked for the hospitals studied,” said Rogak, who studies aerosols at UBC’s Energy and Aerosols Laboratory. Rogak did not participate in the study.
“The authors note several limitations, including that increased healthcare worker testing may have been triggered by the higher values of PCR counts from the floor swabs. But this doesn’t seem to be a problem to me, because if the floor swabs motivate the hospital to test workers more, and that results in identifying outbreaks sooner, then great,” he said.
“Another limitation is that if the hospital has better HVAC or uses air purifiers, it could remove the most infectious aerosols, but the large droplets that fall quickly to the ground would remain, and this would still result in high PCR counts from floor swabs. In this case, perhaps the floor swabs would be a poorer indication of impending outbreaks,” said Rogak.
Determining the best timing and location for floor swabbing might be challenging and specific to the particular hospital, he added. ”For example, you would not want to take swabs from floors right after they are cleaned. Overall, I think this method deserves further development, and it could become a standard technique, but the details might require refinement for widespread application.”
Adrian Popp, MD, chair of the Infectious Disease Service at Huntington Hospital–Northwell Health in New York, said that, although interesting, the study would not change his current practice.
“I’m going to start testing the environment in different rooms in the hospital, and yes, I might find different amounts of COVID, but what does that mean? If pieces of RNA from COVID are on the floor, the likelihood is that they’re not infectious,” Popp said in an interview.
“Hospital workers do get sick with COVID, and sometimes they are asymptomatic and come to work. Patients may come into the hospital for another reason and be sick with COVID. There are many ways people who work in the hospital, as well as the patients, can get COVID. To me, it means that in that hospital and community there is a lot of COVID, but I can’t tell if there is causation here. Who is giving COVID to whom? What am I supposed to do with the information?”
The study was supported by the Northern Ontario Academic Medicine Association Clinical Innovation Opportunities Fund, the Ottawa Hospital Academic Medical Organization Innovation Fund, and a Canadian Institutes of Health Research Operating Grant. One author was a consultant for ProofDx, a startup company creating a point-of-care diagnostic test for COVID-19, and is an advisor for SIGNAL1, a startup company deploying machine-learning models to improve inpatient care. Nott, Rogak, and Popp reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The viral burden of SARS-CoV-2 on floors, even in healthcare worker–only areas, was strongly associated with COVID-19 outbreaks in two acute-care hospitals, according to a new study from Ontario, Canada.
With every 10-fold increase in viral copies, the chance of an impending outbreak of COVID-19 rose 22-fold.
“These data add to the mounting evidence that built environment detection for SARS-CoV-2 may provide an additional layer of monitoring and could help inform local infection prevention and control measures,” they wrote.
The study was published online in Infection Control & Hospital Epidemiology.
Preventing Future Suffering
The current study builds on the researchers’ previous work, which found the same correlation between viral load on floors and COVID outbreaks in long-term care homes.
Currently, the best-known method of environmental surveillance for COVID is wastewater detection. “Swabbing the floors would be another approach to surveillance,” senior author Caroline Nott, MD, infectious disease physician at the Ottawa Hospital, said in an interview.
“We do have environmental surveillance with wastewater, but while this may tell you what’s going on in the city, it doesn’t tell you what is going on in a particular ward of a hospital, for instance,” she added.
Nott and her colleagues believe that swabbing, which is easy and relatively inexpensive, will become another tool to examine the built environment. “Instead of having to close a whole hospital, for example, we could just close one room instead of an entire ward if swabbing showed a high concentration of COVID,” Nott said.
The current study was conducted at two hospitals in Ontario between July 2022 and March 2023. The floors of healthcare worker–only areas on four inpatient adult wards were swabbed. These areas included changing rooms, meeting rooms, staff washrooms, nursing stations, and interdisciplinary team rooms.
SARS-CoV-2 RNA was detected on 537 of 760 floor swabs (71%). The overall positivity rate in the first hospital was 90% (n = 280). In the second hospital, the rate was 60% (n = 480).
Four COVID-19 outbreaks occurred in the first acute care hospital, and seven outbreaks occurred at the second hospital. Outbreaks occurred mostly among hospitalized patients (140 cases), but also in four hospital workers.
COVID-19 still requires vigilance, said Nott. “We weren’t prepared for COVID, and so as a result, many people died or have suffered long-term effects, especially vulnerable people like those being treated in hospital or in long-term care facilities. We want to develop methods to prevent similar suffering in the future, whether it’s a new COVID variant or a different pathogen altogether.”
Changing Surveillance Practice?
“This is a good study,” Steven Rogak, PhD, professor of mechanical engineering at the University of British Columbia (UBC) in Vancouver, Canada, said in an interivew. “The fundamental idea is that respiratory droplets and aerosols will deposit on the floor, and polymerase chain reaction [PCR] tests of swabs will provide a surrogate measurement of what might have been inhaled. There are solid statistics that it worked for the hospitals studied,” said Rogak, who studies aerosols at UBC’s Energy and Aerosols Laboratory. Rogak did not participate in the study.
“The authors note several limitations, including that increased healthcare worker testing may have been triggered by the higher values of PCR counts from the floor swabs. But this doesn’t seem to be a problem to me, because if the floor swabs motivate the hospital to test workers more, and that results in identifying outbreaks sooner, then great,” he said.
“Another limitation is that if the hospital has better HVAC or uses air purifiers, it could remove the most infectious aerosols, but the large droplets that fall quickly to the ground would remain, and this would still result in high PCR counts from floor swabs. In this case, perhaps the floor swabs would be a poorer indication of impending outbreaks,” said Rogak.
Determining the best timing and location for floor swabbing might be challenging and specific to the particular hospital, he added. ”For example, you would not want to take swabs from floors right after they are cleaned. Overall, I think this method deserves further development, and it could become a standard technique, but the details might require refinement for widespread application.”
Adrian Popp, MD, chair of the Infectious Disease Service at Huntington Hospital–Northwell Health in New York, said that, although interesting, the study would not change his current practice.
“I’m going to start testing the environment in different rooms in the hospital, and yes, I might find different amounts of COVID, but what does that mean? If pieces of RNA from COVID are on the floor, the likelihood is that they’re not infectious,” Popp said in an interview.
“Hospital workers do get sick with COVID, and sometimes they are asymptomatic and come to work. Patients may come into the hospital for another reason and be sick with COVID. There are many ways people who work in the hospital, as well as the patients, can get COVID. To me, it means that in that hospital and community there is a lot of COVID, but I can’t tell if there is causation here. Who is giving COVID to whom? What am I supposed to do with the information?”
The study was supported by the Northern Ontario Academic Medicine Association Clinical Innovation Opportunities Fund, the Ottawa Hospital Academic Medical Organization Innovation Fund, and a Canadian Institutes of Health Research Operating Grant. One author was a consultant for ProofDx, a startup company creating a point-of-care diagnostic test for COVID-19, and is an advisor for SIGNAL1, a startup company deploying machine-learning models to improve inpatient care. Nott, Rogak, and Popp reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM INFECTION CONTROL & HOSPITAL EPIDEMIOLOGY
Is Being ‘Manly’ a Threat to a Man’s Health?
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
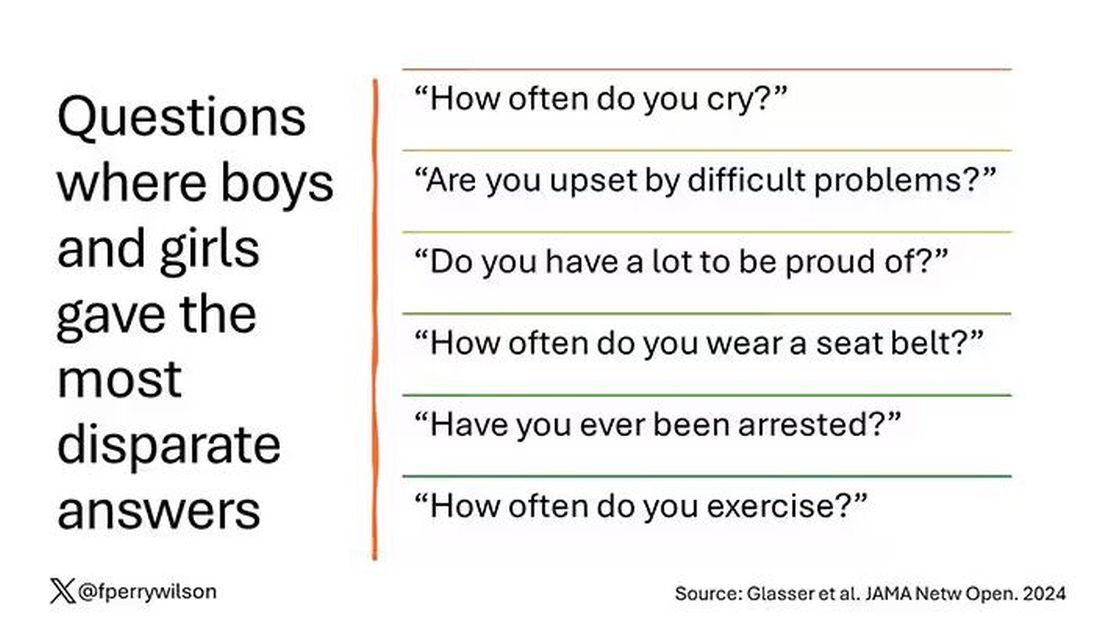
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here.
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
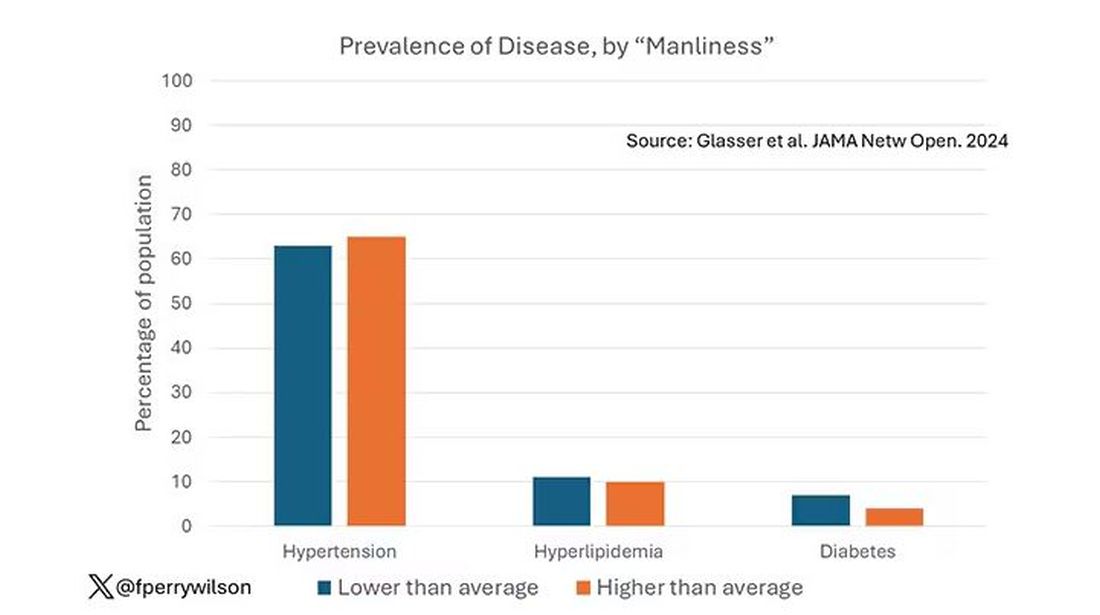
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
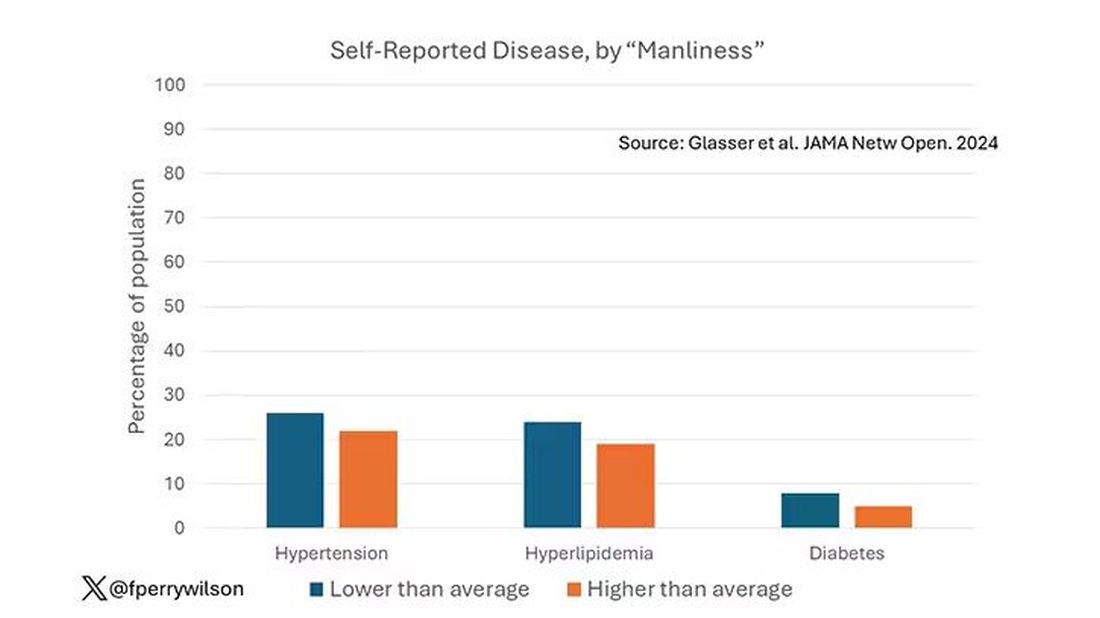
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.
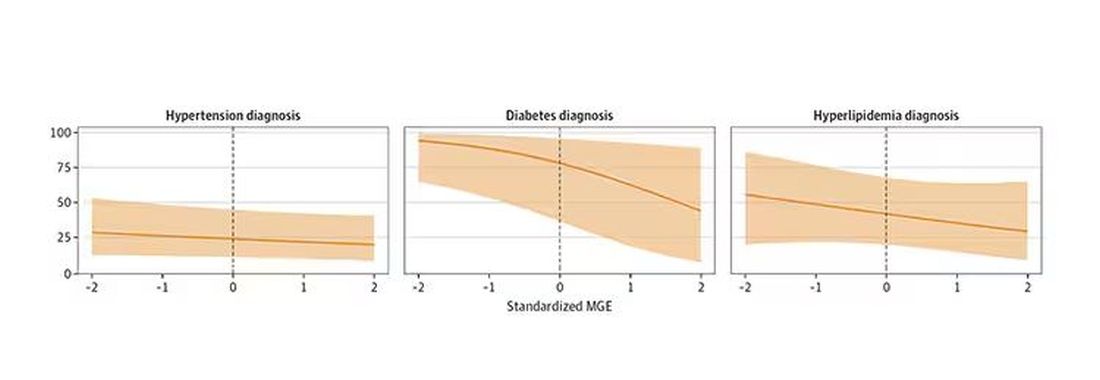
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here.
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here.
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
New mRNA Vaccine May Shield Against C difficile Infections
A group of researchers from the University of Pennsylvania, Philadelphia, has developed a messenger RNA (mRNA) vaccine, delivered via lipid nanoparticles (LNPs) — the same type as the COVID-19 vaccine produced by Moderna and Pfizer — targeting Clostridioides difficile (formerly Clostridium difficile). According to the authors, the results of their preclinical study, published in Science, demonstrated this technology as a promising platform for C difficile vaccine development and could be the starting point for curbing intestinal infections that, in their most severe forms (pseudomembranous colitis, toxic megacolon), can be fatal.
An Increasingly Pressing Issue
C difficile is the leading cause of infectious diarrhea acquired in healthcare settings.
A 2019 study reported a global incidence of C difficile infections at 2.2 per 1000 hospital admissions per year and 3.5 per 10,000 patient-days per year.
The Vaccine Candidate
Vaccine candidates tested so far have used toxoids or recombinant proteins targeting the combined repetitive oligopeptide (CROP) or receptor-binding domain (RBD) of the two primary C difficile toxins, TcdA and TcdB. The US researchers are now exploring the mRNA-LNP vaccine approach to target multiple antigens simultaneously. They developed a bivalent vaccine (including the CROP and RBD domains of both toxins) and a trivalent vaccine (with an additional virulence factor, the metalloprotease Pro-Pro endopeptidase-1).
Mice vaccinated with the bivalent and trivalent vaccines produced immunoglobulin G antibody titers two to four times higher than those elicited by recombinant protein with an adjuvant. The vaccination stimulated the proliferation of follicular T helper cells and the antigen-specific response of B lymphocytes, laying the foundation for a strong and long-lasting humoral response. The vaccines were also immunogenic in hamsters.
Vaccinated mice not only survived a toxin dose five times higher than the 100% lethal dose but also demonstrated the vaccine’s protective effect through serum transfer; unvaccinated mice given serum from vaccinated mice survived the lethal challenge. More importantly, when exposed to a lethal dose of the bacterium itself, all vaccinated mice survived.
To demonstrate the vaccine’s efficacy in patients with a history of C difficile infection and high recurrence risk — ideal candidates for vaccination — the researchers vaccinated mice that had previously survived a sublethal infection. Six months after the initial infection and vaccination, these mice remained protected against mortality when reexposed to the bacterium.
Additionally, a quadrivalent vaccine that included an immunogen targeting C difficile spores — key agents in transmission — also proved effective. Low levels of bacteria and toxins in the feces of mice vaccinated in this way suggested that spore vaccination could limit initial colonization.
In tests with nonhuman primates, two doses of the vaccines targeting either the vegetative form or the spores elicited strong immune responses against bacterial toxins and virulence factors. Human trials may indeed be on the horizon.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
A group of researchers from the University of Pennsylvania, Philadelphia, has developed a messenger RNA (mRNA) vaccine, delivered via lipid nanoparticles (LNPs) — the same type as the COVID-19 vaccine produced by Moderna and Pfizer — targeting Clostridioides difficile (formerly Clostridium difficile). According to the authors, the results of their preclinical study, published in Science, demonstrated this technology as a promising platform for C difficile vaccine development and could be the starting point for curbing intestinal infections that, in their most severe forms (pseudomembranous colitis, toxic megacolon), can be fatal.
An Increasingly Pressing Issue
C difficile is the leading cause of infectious diarrhea acquired in healthcare settings.
A 2019 study reported a global incidence of C difficile infections at 2.2 per 1000 hospital admissions per year and 3.5 per 10,000 patient-days per year.
The Vaccine Candidate
Vaccine candidates tested so far have used toxoids or recombinant proteins targeting the combined repetitive oligopeptide (CROP) or receptor-binding domain (RBD) of the two primary C difficile toxins, TcdA and TcdB. The US researchers are now exploring the mRNA-LNP vaccine approach to target multiple antigens simultaneously. They developed a bivalent vaccine (including the CROP and RBD domains of both toxins) and a trivalent vaccine (with an additional virulence factor, the metalloprotease Pro-Pro endopeptidase-1).
Mice vaccinated with the bivalent and trivalent vaccines produced immunoglobulin G antibody titers two to four times higher than those elicited by recombinant protein with an adjuvant. The vaccination stimulated the proliferation of follicular T helper cells and the antigen-specific response of B lymphocytes, laying the foundation for a strong and long-lasting humoral response. The vaccines were also immunogenic in hamsters.
Vaccinated mice not only survived a toxin dose five times higher than the 100% lethal dose but also demonstrated the vaccine’s protective effect through serum transfer; unvaccinated mice given serum from vaccinated mice survived the lethal challenge. More importantly, when exposed to a lethal dose of the bacterium itself, all vaccinated mice survived.
To demonstrate the vaccine’s efficacy in patients with a history of C difficile infection and high recurrence risk — ideal candidates for vaccination — the researchers vaccinated mice that had previously survived a sublethal infection. Six months after the initial infection and vaccination, these mice remained protected against mortality when reexposed to the bacterium.
Additionally, a quadrivalent vaccine that included an immunogen targeting C difficile spores — key agents in transmission — also proved effective. Low levels of bacteria and toxins in the feces of mice vaccinated in this way suggested that spore vaccination could limit initial colonization.
In tests with nonhuman primates, two doses of the vaccines targeting either the vegetative form or the spores elicited strong immune responses against bacterial toxins and virulence factors. Human trials may indeed be on the horizon.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
A group of researchers from the University of Pennsylvania, Philadelphia, has developed a messenger RNA (mRNA) vaccine, delivered via lipid nanoparticles (LNPs) — the same type as the COVID-19 vaccine produced by Moderna and Pfizer — targeting Clostridioides difficile (formerly Clostridium difficile). According to the authors, the results of their preclinical study, published in Science, demonstrated this technology as a promising platform for C difficile vaccine development and could be the starting point for curbing intestinal infections that, in their most severe forms (pseudomembranous colitis, toxic megacolon), can be fatal.
An Increasingly Pressing Issue
C difficile is the leading cause of infectious diarrhea acquired in healthcare settings.
A 2019 study reported a global incidence of C difficile infections at 2.2 per 1000 hospital admissions per year and 3.5 per 10,000 patient-days per year.
The Vaccine Candidate
Vaccine candidates tested so far have used toxoids or recombinant proteins targeting the combined repetitive oligopeptide (CROP) or receptor-binding domain (RBD) of the two primary C difficile toxins, TcdA and TcdB. The US researchers are now exploring the mRNA-LNP vaccine approach to target multiple antigens simultaneously. They developed a bivalent vaccine (including the CROP and RBD domains of both toxins) and a trivalent vaccine (with an additional virulence factor, the metalloprotease Pro-Pro endopeptidase-1).
Mice vaccinated with the bivalent and trivalent vaccines produced immunoglobulin G antibody titers two to four times higher than those elicited by recombinant protein with an adjuvant. The vaccination stimulated the proliferation of follicular T helper cells and the antigen-specific response of B lymphocytes, laying the foundation for a strong and long-lasting humoral response. The vaccines were also immunogenic in hamsters.
Vaccinated mice not only survived a toxin dose five times higher than the 100% lethal dose but also demonstrated the vaccine’s protective effect through serum transfer; unvaccinated mice given serum from vaccinated mice survived the lethal challenge. More importantly, when exposed to a lethal dose of the bacterium itself, all vaccinated mice survived.
To demonstrate the vaccine’s efficacy in patients with a history of C difficile infection and high recurrence risk — ideal candidates for vaccination — the researchers vaccinated mice that had previously survived a sublethal infection. Six months after the initial infection and vaccination, these mice remained protected against mortality when reexposed to the bacterium.
Additionally, a quadrivalent vaccine that included an immunogen targeting C difficile spores — key agents in transmission — also proved effective. Low levels of bacteria and toxins in the feces of mice vaccinated in this way suggested that spore vaccination could limit initial colonization.
In tests with nonhuman primates, two doses of the vaccines targeting either the vegetative form or the spores elicited strong immune responses against bacterial toxins and virulence factors. Human trials may indeed be on the horizon.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
AI in Medicine: Are Large Language Models Ready for the Exam Room?
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
Six Tips for Media Interviews
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
H pylori: ACG Guideline Advises New Approaches to Treatment
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.
Helicobacter pylori is one of the most common human bacterial chronic infections globally. Its prevalence has actually decreased in North America in recent years, although its current range of approximately 30%-40% remains substantial given the potential clinical implications of infection.
Standards have changed considerably regarding the testing, treatment, and follow-up of H pylori. This is made clear by the just-published clinical practice guideline from the American College of Gastroenterology (ACG), which provides several new recommendations based on recent scientific evidence that should change your clinical approach to managing this common infection.
This discussion aims to synthesize and highlight key concepts from the ACG’s comprehensive publication.
Who Should Be Tested and Treated?
The cardinal diseases caused by H pylori have traditionally included peptic ulcer disease, marginal zone B-cell lymphoma, gastric adenocarcinoma, and dyspepsia.
Additional associations have been made with idiopathic thrombocytopenic purpura and otherwise unexplained iron deficiency.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose aspirin, are relatively more susceptible to infection.
The ACG’s guideline also recommends testing persons at an increased risk for gastric adenocarcinoma (eg, those with autoimmune gastritis, current or history of premalignant conditions, or first-degree relative with gastric cancer), as well as household members of patients with a positive nonserologic test for H pylori.
The authors note that those with an indication for testing should be offered treatment if determined to have an infection. These patients should also undergo a posttreatment test-of-cure, which should occur at least 4 weeks afterwards using a urea breath test, fecal antigen test, or gastric biopsy.
Caveats to Treatment
Patients with H pylori infections are advised to undergo treatment for a duration of 14 days. Some of the commercial prepackaged H pylori treatment options (eg, Pylera, which contains bismuth subcitrate/metronidazole/tetracycline) are dispensed in regimens lasting only 10 days and currently are viewed as inadequate.
In the United States, the patterns of antibiotic resistance for the previously used standard drugs in the treatment of H pylori have increased considerably. They range from 32% for clarithromycin, 38% for levofloxacin, and 42% for metronidazole, in contrast to 3% for amoxicillin, 1% for tetracycline, and 0% for rifabutin.
Clarithromycin- and levofloxacin-containing treatments should be avoided in treatment-naive patients unless specifically directed following the results of susceptibility tests with either a phenotypic method (culture-based) or a molecular method (polymerase chain reaction or next-generation sequencing). Notably, the mutations responsible for both clarithromycin and levofloxacin resistance may be detectable by stool-based testing.
Maintenance of intragastric acid suppression is key to H pylori eradication, as elevated intragastric pH promotes active replication of H pylori and makes it more susceptible to bactericidal antibiotics.
Therefore, the use of histamine-2 receptors is not recommended, as they are inadequate for achieving acid suppression. Instead, a dual-based therapy of either the potassium-competitive acid blocker (PCAB) vonoprazan (20 mg) or a high-dose proton pump inhibitor (PPI) and amoxicillin, administered twice daily, is effective, although this finding is based on limited evidence.
Treatment-Naive Patients
In treatment-naive patients without penicillin allergy and for whom antibiotic susceptibility testing has not been obtained, the guideline offers its strongest recommendation for bismuth quadruple therapy. This therapy typically consists of a PPI, bismuth subcitrate or subsalicylate, tetracycline, and metronidazole.
Among those with a penicillin allergy, bismuth quadruple therapy is also the primary treatment choice. The authors suggest that patients with a suspected allergy are referred to an allergist for possible penicillin desensitization, given that less than 1% of the population is thought to present with a “true” allergy.
The guideline also presented conditional recommendations, based on low- to moderate-quality evidence, for using a rifabutin-based triple regimen of omeprazole, amoxicillin, and rifabutin (Talicia); a PCAB-based dual regimen of vonoprazan and amoxicillin (Voquezna Dual Pak); and a PCAB-based triple regimen of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak). In patients with unknown clarithromycin susceptibility, the PCAB-based triple therapy is preferred over PPI-clarithromycin triple therapy.
Although probiotics have been suggested to possibly lead to increased effectiveness or tolerability for H pylori eradication, this was based on studies with significant heterogeneity in their designs. At present, no high-quality data support probiotic therapy.
Clinicians may substitute doxycycline for tetracycline due to availability or cost, and also may prescribe metronidazole at a lower dose than recommended (1.5-2 g/d) to limit side effects. Both modifications have been associated with lower rates of H pylori eradication and are not recommended.
Treatment-Experienced Patients
Quadruple bismuth therapy is the optimal approach among treatment-experienced patients with persistent H pylori infection who have not previously received this therapy. However, this recommendation was rated as conditional, given that it was based on a low quality of evidence.
The guideline offered other recommendations for treatment-experienced patients with persistent infection who had received bismuth quadruple therapy — also conditionally based on a low quality of evidence.
In such patients, it is recommended to consider the use of a rifabutin-based triple therapy (ie, a PPI standard to double dose, amoxicillin, and rifabutin) and a levofloxacin-based triple therapy (ie, a PPI standard dose, levofloxacin, and amoxicillin or metronidazole).
Although significant evidence gaps prevented the authors from providing formal recommendations, they included a PCAB-based triple therapy of vonoprazan, clarithromycin, and amoxicillin (Voquezna Triple Pak) and a high-dose dual therapy of either vonoprazan (20 mg) or PPI (double dose) and amoxicillin among their suggested salvage regimens for these patients.
A New Standard
We must recognize, however, that there are still substantial evidence gaps, particularly around the use of a PCAB-based regimen and its relative advantages over a standard or high-dose PPI-based regimen. This may be of particular importance based on the variable prevalence of cytochrome P450 2C19 (CYP2C19) polymorphisms in the specific patient populations, as PCABs are not metabolized by CYP2C19.
Reviewing the entirety of the ACG’s clinical guideline is encouraged for additional details about the management of H pylori beyond what is highlighted herein.
Dr. Johnson, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School, Norfolk, Virginia, disclosed ties with ISOTHRIVE and Johnson & Johnson.
A version of this article appeared on Medscape.com.