User login
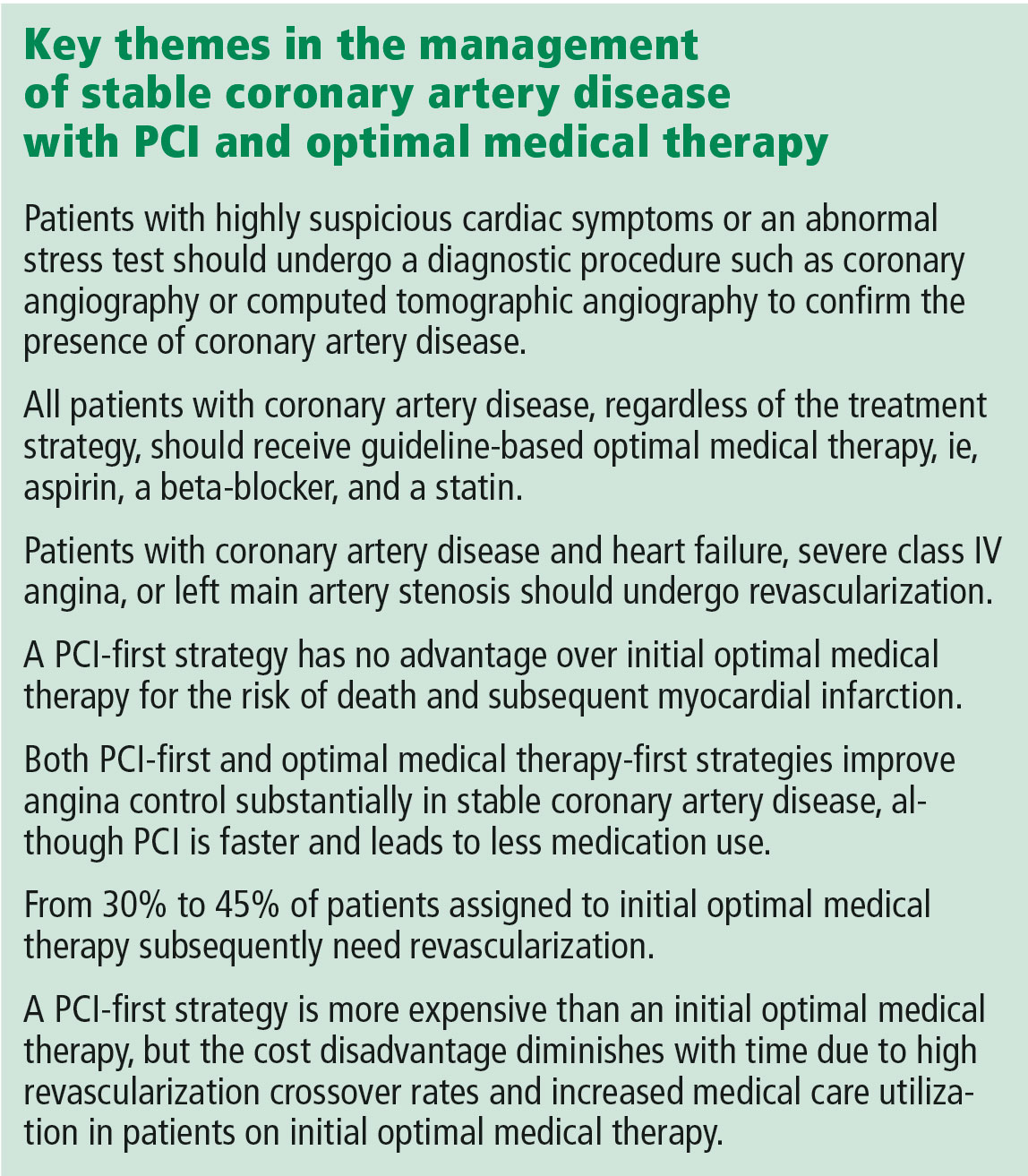
Invented by Andreas Grüntzig in 1977, percutaneous coronary intervention (PCI) has revolutionized the management of coronary artery disease.1 Initially, PCI was more attractive than conventional revascularization with coronary artery bypass grafting because it was less invasive, but as time went on PCI acquired its own evidence base of improved clinical outcomes. In fact, for ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, and cardiogenic shock, there is clear evidence that PCI saves lives in both the short and long term.2,3
But PCI is also used widely in stable coronary artery disease, and in contrast to the clear-cut benefit in the acute conditions noted above, a series of reports culminating in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial has shown that PCI in stable coronary artery disease does not reduce the risk of death or of subsequent myocardial infarction.4,5 Cardiologists have heeded the COURAGE trial findings in their clinical decision-making, and the rate of PCI for stable coronary artery disease dropped by 60% from 2006 to 2011.6
In an article in this issue,7 Dr. Michael Rothberg describes a 55-year-old man who develops new-onset angina and then undergoes a Bruce protocol stress test that is stopped at 6 minutes due to chest pain and ST-segment depression. Dr. Rothberg argues that, based on COURAGE trial data, this patient and other patients with stable coronary artery disease should not be treated with PCI but instead should receive optimal medical therapy.
KEY ISSUES ABOUT THE COURAGE TRIAL
To understand the applicability of the results of the COURAGE trial to patient care, it is important to examine a number of key issues about this trial.
First, COURAGE enrolled a narrow group of patients with stable coronary artery disease and excluded many common patient subgroups, such as those with heart failure, severe anginal symptoms, or left main artery stenosis, who would benefit from revascularization.5 Specifically, for every 100 patients enrolled in COURAGE, 161 were excluded for having heart failure, 39 were excluded for class IV angina, and 31 were excluded for left main stenosis.
Second, although COURAGE has been described as a trial of PCI vs optimal medical therapy, it was not. Rather, it was a trial of optimal medical therapy with PCI first vs optimal medical therapy with crossover PCI if medical therapy failed.5 The crossover rate was not insubstantial: 16.1% of the patients in the medical therapy group underwent PCI by the end of the first year, increasing to 32.6% at a median of 4.6 years of follow-up.5,7 And patients with more intense and frequent angina and resulting worse quality of life were the ones who required crossover PCI.8
Third, it has been proposed that patients with suspicious cardiac symptoms or abnormal stress test findings can be managed with optimal medical therapy initially, based on the COURAGE findings. However, the COURAGE trial required diagnostic angiography both to confirm underlying coronary artery disease and to exclude left main disease.5 Thus, regardless of one’s position on the role of PCI in stable coronary artery disease, diagnostic investigation by cardiac catheterization or computed tomographic angiography to confirm the presence or absence of coronary artery disease remains mandatory.
Fourth, optimal medical therapy was prescribed by the trial’s protocol, so that one would expect that both treatment groups received similar levels of optimal medical therapy. However, the optimal medical therapy group required more medications to achieve the same outcome as the PCI group.5
Finally, although it has been reported that the COURAGE trial showed no benefit for PCI, in fact, for the outcome of symptom relief, initial PCI was clearly superior to optimal medical therapy beginning at 3 months and extending out to 24 months—a result for which the magnitude of benefit is underestimated due to the occurrence of crossover PCI.9 In particular, women and patients with a high frequency of angina derived improvement in angina-related quality of life from PCI compared with optimal medical therapy.8,10
A MORE NUANCED INTERPRETATION
For these reasons, the role of PCI in stable coronary disease is more nuanced than simply stating that the COURAGE trial results were “negative” for PCI. It is more accurate to say that in selected patients with moderate symptoms of angina and without heart failure or left main artery disease, a PCI-first strategy has no advantage over an optimal medical treatment-first strategy for the risk of death and myocardial infarction but does lead to earlier angina relief and less long-term need for medication. In addition, in up to one-third of cases, an optimal medical treatment-first strategy fails and requires crossover to PCI.5
Dr. Rothberg is correct in highlighting the crucial importance of optimal medical therapy in the management of stable coronary artery disease. In fact, cardiologists strive to prescribe optimal medical treatment for all coronary artery disease patients irrespective of treatment strategy. However, 3 important issues in his analysis need to be highlighted.
Controlling symptoms is important, and we should not underrate it. The patient described in Dr. Rothberg’s article could exercise for only 6 minutes on a Bruce treadmill test, indicating a quite limited functional capacity of only 5.8 metabolic equivalents of the task (METs).11 (A healthy 55-year-old man should be able to achieve 10.5 METs.12) Inability to achieve 6 METs precludes the ability to dance, to ride a bike at a moderate pace, or to go on a hike.13 For many patients, these limitations are serious and important concerns for their lifestyle and quality of life. PCI has been shown to be superior to medical therapy in improving functional capacity, improving it by 20% vs 2% in one trial14 and 26% vs 7% in a second trial.14 Patients undergoing PCI were twice as likely to have a greater than 2-minute increase in exercise capacity.15 Recognizing the importance of symptom control in stable coronary artery disease is patient-centered care.
Patient decision-making is complicated, and we should not assume that patients choose PCI primarily to reduce their risk of death. A randomized trial showed that patients continued to select PCI as initial treatment even when they clearly knew that it would not prevent death or myocardial infarction.16 As noted above, patients may value earlier symptom relief, particularly if their angina is frequent or limiting. In addition, patients strongly desire to minimize medical therapy and may be willing to trade decreased life expectancy to reduce the need to take medications.17 Finally, some patients may want to be able to continue to participate in certain lifestyle activities.
PCI is expensive, but less so over the long run. With a PCI-first strategy, costs are front-loaded, and studies with short-term follow-up show a marked increase in cost. However, long-term follow-up shows that the cost differences diminish dramatically due to high rates of crossover to revascularization and increased medical care in the optimal medical therapy arm. The cumulative lifetime costs in the COURAGE trial with a PCI-first strategy, although statistically significant, were only 10% higher than with the optimal medical treatment-first strategy ($99,820 vs $90,370).18 Therefore, substantial long-term cost-savings by shifting from an initial PCI strategy to initial optimal medical therapy are unlikely to be delivered when measured over the long term.
NEWER TRIALS SUPPORT A BALANCED APPROACH
The most recent studies of the management of stable coronary artery disease support a balanced approach.
The ORBITA trial (Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina), on one hand, showed limited benefit of PCI vs medical therapy in patients with single-vessel coronary artery disease, preserved functional capacity, and mild symptoms.19 There was no significant improvement in exercise capacity or angina frequency, although baseline angina frequency after medical stabilization was quite low.
The FAME 2 trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation), on the other hand, studied patients with positive fractional flow reserve coronary artery disease (ie, using an invasive technique to confirm the hemodynamic significance of the coronary stenosis) and showed markedly better outcomes with PCI than with medical therapy.20 Specifically, the PCI-first group had improved quality of life and dramatically less need for urgent revascularization.
Furthermore, as in the COURAGE trial, the optimal medical therapy group had a high crossover rate to PCI (44.2%), leading to the complete elimination of the early cost advantage of medical therapy by 3 years. The initial costs with PCI vs medical therapy were $9,944 vs $4,439 (P < .001); the 3-year costs were $16,792 vs $16,737 (P = .94).
For these reasons, a balanced approach to recommending PCI first vs optimal medical treatment first remains the best strategy.
TOWARD PATIENT-CENTERED CARE
For the 55-year-old patient in Dr. Rothberg’s article, the first step in making an appropriate decision would be to understand the severity of symptoms relative to the patient’s lifestyle. The second step is to assess the patient’s interest in an invasive procedure such as PCI relative to optimal medical therapy, as the patient may have a strong preference for one option or the other.
Finally, with the understanding that there is no difference in hard end points of myocardial infarction and death, a balanced discussion of the advantages and disadvantages of both PCI and optimal medical therapy would be needed. For PCI, advantages include earlier symptom control and improved quality of the life, particularly if symptoms are severe, with disadvantages of an invasive procedure with its attendant risks. For optimal medical therapy, advantages include improved symptom control and avoidance of an invasive procedure, while disadvantages include increased medication use and a high rate of eventual crossover to PCI. This important discussion integrating both patient and medical perspectives ultimately leads to the best decision for the individual patient.
A patient-centered approach to clinical decision-making mandates inclusion of PCI first as an option in the management of stable coronary artery disease. After confirming the patient has coronary artery disease, patients with heart failure, class IV angina at rest, or left main artery stenosis should be referred for revascularization. In the remaining patients with confirmed coronary artery disease and moderate angina symptoms, either PCI first or optimal medical therapy first is an appropriate initial strategy that considers coronary anatomy, symptom burden, and patient desires.
- Meier B. The first patient to undergo coronary angioplasty—23-year follow-up. N Engl J Med 2001; 344:144–145.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011; 124:2574–2609.
- Fox KAA, Clayton TC, Damman P, et al. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol 2010; 55:2435–2445.
- Katritsis DG, Ioannidis JPA. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation 2005; 111:2906–2912.
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Bangalore S, Gupta N, Généreux P, Guo Y, Pancholy S, Feit F. Trend in percutaneous coronary intervention volume following the COURAGE and BARI-2D trials: insight from over 8.1 million percutaneous coronary interventions. Int J Cardiol 2015; 183:6–10.
- Rothberg MB. PCI for stable angina: a missed opportunity for shared decision-making. Cleve Clin J Med 2018; 85:105–121.
- Spertus JA, Maron DJ, Cohen DJ, et al. Frequency, predictors, and consequences of crossing over to revascularization within 12 months of randomization to optimal medical therapy in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial. Circ Cardiovasc Qual Outcomes 2013; 6:409–418.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Acharjee S, Teo KK, Jacobs AK, et al. Optimal medical therapy with or without percutaneous coronary intervention in women with stable coronary disease: a pre-specified subset analysis of the Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation (COURAGE) trial. Am Heart J 2016; 173:108–117.
- Foster C, Jackson AS, Pollock ML, et al. Generalized equations for predicting functional capacity from treadmill performance. Am Heart J 1984; 107:1229–1234.
- Morris CK, Myers J, Froelicher VF, Kawaguchi T, Ueshima K, Hideg A. Nomogram based on metabolic equivalents and age for assessing aerobic exercise capacity in men. J Am Coll Cardiol 1993; 22:175–182.
- Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 1990; 13:555–565.
- Erne P, Schoenenberger AW, Burckhardt D, et al. Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial. JAMA 2007; 297:1985–1991.
- Strauss WE, Fortin T, Hartigan P, Folland ED, Parisi AF. A comparison of quality of life scores in patients with angina pectoris after angioplasty compared with after medical therapy. Outcomes of a randomized clinical trial. Veterans Affairs Study of Angioplasty Compared to Medical Therapy Investigators. Circulation 1995; 92:1710–1719.
- Coylewright M, Dick S, Zmolek B, et al. PCI choice decision aid for stable coronary artery disease: a randomized trial. Circ Cardiovasc Qual Outcomes 2016; 9:767–776.
- Fontana M, Asaria P, Moraldo M, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation 2014; 129:2539–2546.
- Weintraub WS, Boden WE, Zhang Z, et al. Cost-effectiveness of percutaneous coronary intervention in optimally treated stable coronary patients. Circ Cardiovasc Qual Outcomes 2008; 1:12–20.
- Al-Lamee R, Thompson D, Dehbi H-M, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet November 2, 2017; doi:10.1016/S0140-6736(17)32714-9.
- Fearon WF, Nishi T, Bruyne BD, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: three-year follow-up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation November 2017; doi:10.1161/CIRCULATIONAHA.117.031907.
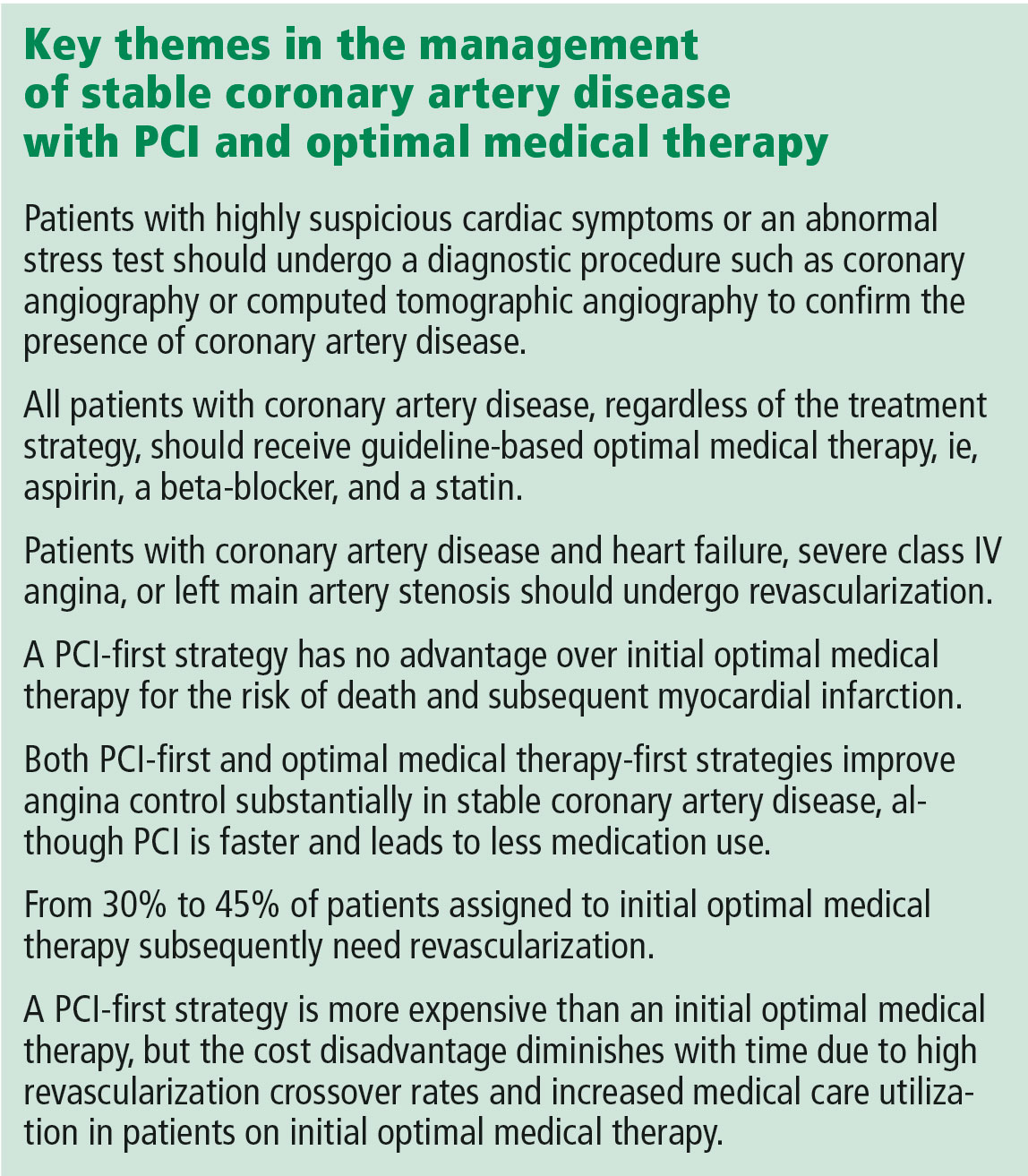
Invented by Andreas Grüntzig in 1977, percutaneous coronary intervention (PCI) has revolutionized the management of coronary artery disease.1 Initially, PCI was more attractive than conventional revascularization with coronary artery bypass grafting because it was less invasive, but as time went on PCI acquired its own evidence base of improved clinical outcomes. In fact, for ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, and cardiogenic shock, there is clear evidence that PCI saves lives in both the short and long term.2,3
But PCI is also used widely in stable coronary artery disease, and in contrast to the clear-cut benefit in the acute conditions noted above, a series of reports culminating in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial has shown that PCI in stable coronary artery disease does not reduce the risk of death or of subsequent myocardial infarction.4,5 Cardiologists have heeded the COURAGE trial findings in their clinical decision-making, and the rate of PCI for stable coronary artery disease dropped by 60% from 2006 to 2011.6
In an article in this issue,7 Dr. Michael Rothberg describes a 55-year-old man who develops new-onset angina and then undergoes a Bruce protocol stress test that is stopped at 6 minutes due to chest pain and ST-segment depression. Dr. Rothberg argues that, based on COURAGE trial data, this patient and other patients with stable coronary artery disease should not be treated with PCI but instead should receive optimal medical therapy.
KEY ISSUES ABOUT THE COURAGE TRIAL
To understand the applicability of the results of the COURAGE trial to patient care, it is important to examine a number of key issues about this trial.
First, COURAGE enrolled a narrow group of patients with stable coronary artery disease and excluded many common patient subgroups, such as those with heart failure, severe anginal symptoms, or left main artery stenosis, who would benefit from revascularization.5 Specifically, for every 100 patients enrolled in COURAGE, 161 were excluded for having heart failure, 39 were excluded for class IV angina, and 31 were excluded for left main stenosis.
Second, although COURAGE has been described as a trial of PCI vs optimal medical therapy, it was not. Rather, it was a trial of optimal medical therapy with PCI first vs optimal medical therapy with crossover PCI if medical therapy failed.5 The crossover rate was not insubstantial: 16.1% of the patients in the medical therapy group underwent PCI by the end of the first year, increasing to 32.6% at a median of 4.6 years of follow-up.5,7 And patients with more intense and frequent angina and resulting worse quality of life were the ones who required crossover PCI.8
Third, it has been proposed that patients with suspicious cardiac symptoms or abnormal stress test findings can be managed with optimal medical therapy initially, based on the COURAGE findings. However, the COURAGE trial required diagnostic angiography both to confirm underlying coronary artery disease and to exclude left main disease.5 Thus, regardless of one’s position on the role of PCI in stable coronary artery disease, diagnostic investigation by cardiac catheterization or computed tomographic angiography to confirm the presence or absence of coronary artery disease remains mandatory.
Fourth, optimal medical therapy was prescribed by the trial’s protocol, so that one would expect that both treatment groups received similar levels of optimal medical therapy. However, the optimal medical therapy group required more medications to achieve the same outcome as the PCI group.5
Finally, although it has been reported that the COURAGE trial showed no benefit for PCI, in fact, for the outcome of symptom relief, initial PCI was clearly superior to optimal medical therapy beginning at 3 months and extending out to 24 months—a result for which the magnitude of benefit is underestimated due to the occurrence of crossover PCI.9 In particular, women and patients with a high frequency of angina derived improvement in angina-related quality of life from PCI compared with optimal medical therapy.8,10
A MORE NUANCED INTERPRETATION
For these reasons, the role of PCI in stable coronary disease is more nuanced than simply stating that the COURAGE trial results were “negative” for PCI. It is more accurate to say that in selected patients with moderate symptoms of angina and without heart failure or left main artery disease, a PCI-first strategy has no advantage over an optimal medical treatment-first strategy for the risk of death and myocardial infarction but does lead to earlier angina relief and less long-term need for medication. In addition, in up to one-third of cases, an optimal medical treatment-first strategy fails and requires crossover to PCI.5
Dr. Rothberg is correct in highlighting the crucial importance of optimal medical therapy in the management of stable coronary artery disease. In fact, cardiologists strive to prescribe optimal medical treatment for all coronary artery disease patients irrespective of treatment strategy. However, 3 important issues in his analysis need to be highlighted.
Controlling symptoms is important, and we should not underrate it. The patient described in Dr. Rothberg’s article could exercise for only 6 minutes on a Bruce treadmill test, indicating a quite limited functional capacity of only 5.8 metabolic equivalents of the task (METs).11 (A healthy 55-year-old man should be able to achieve 10.5 METs.12) Inability to achieve 6 METs precludes the ability to dance, to ride a bike at a moderate pace, or to go on a hike.13 For many patients, these limitations are serious and important concerns for their lifestyle and quality of life. PCI has been shown to be superior to medical therapy in improving functional capacity, improving it by 20% vs 2% in one trial14 and 26% vs 7% in a second trial.14 Patients undergoing PCI were twice as likely to have a greater than 2-minute increase in exercise capacity.15 Recognizing the importance of symptom control in stable coronary artery disease is patient-centered care.
Patient decision-making is complicated, and we should not assume that patients choose PCI primarily to reduce their risk of death. A randomized trial showed that patients continued to select PCI as initial treatment even when they clearly knew that it would not prevent death or myocardial infarction.16 As noted above, patients may value earlier symptom relief, particularly if their angina is frequent or limiting. In addition, patients strongly desire to minimize medical therapy and may be willing to trade decreased life expectancy to reduce the need to take medications.17 Finally, some patients may want to be able to continue to participate in certain lifestyle activities.
PCI is expensive, but less so over the long run. With a PCI-first strategy, costs are front-loaded, and studies with short-term follow-up show a marked increase in cost. However, long-term follow-up shows that the cost differences diminish dramatically due to high rates of crossover to revascularization and increased medical care in the optimal medical therapy arm. The cumulative lifetime costs in the COURAGE trial with a PCI-first strategy, although statistically significant, were only 10% higher than with the optimal medical treatment-first strategy ($99,820 vs $90,370).18 Therefore, substantial long-term cost-savings by shifting from an initial PCI strategy to initial optimal medical therapy are unlikely to be delivered when measured over the long term.
NEWER TRIALS SUPPORT A BALANCED APPROACH
The most recent studies of the management of stable coronary artery disease support a balanced approach.
The ORBITA trial (Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina), on one hand, showed limited benefit of PCI vs medical therapy in patients with single-vessel coronary artery disease, preserved functional capacity, and mild symptoms.19 There was no significant improvement in exercise capacity or angina frequency, although baseline angina frequency after medical stabilization was quite low.
The FAME 2 trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation), on the other hand, studied patients with positive fractional flow reserve coronary artery disease (ie, using an invasive technique to confirm the hemodynamic significance of the coronary stenosis) and showed markedly better outcomes with PCI than with medical therapy.20 Specifically, the PCI-first group had improved quality of life and dramatically less need for urgent revascularization.
Furthermore, as in the COURAGE trial, the optimal medical therapy group had a high crossover rate to PCI (44.2%), leading to the complete elimination of the early cost advantage of medical therapy by 3 years. The initial costs with PCI vs medical therapy were $9,944 vs $4,439 (P < .001); the 3-year costs were $16,792 vs $16,737 (P = .94).
For these reasons, a balanced approach to recommending PCI first vs optimal medical treatment first remains the best strategy.
TOWARD PATIENT-CENTERED CARE
For the 55-year-old patient in Dr. Rothberg’s article, the first step in making an appropriate decision would be to understand the severity of symptoms relative to the patient’s lifestyle. The second step is to assess the patient’s interest in an invasive procedure such as PCI relative to optimal medical therapy, as the patient may have a strong preference for one option or the other.
Finally, with the understanding that there is no difference in hard end points of myocardial infarction and death, a balanced discussion of the advantages and disadvantages of both PCI and optimal medical therapy would be needed. For PCI, advantages include earlier symptom control and improved quality of the life, particularly if symptoms are severe, with disadvantages of an invasive procedure with its attendant risks. For optimal medical therapy, advantages include improved symptom control and avoidance of an invasive procedure, while disadvantages include increased medication use and a high rate of eventual crossover to PCI. This important discussion integrating both patient and medical perspectives ultimately leads to the best decision for the individual patient.
A patient-centered approach to clinical decision-making mandates inclusion of PCI first as an option in the management of stable coronary artery disease. After confirming the patient has coronary artery disease, patients with heart failure, class IV angina at rest, or left main artery stenosis should be referred for revascularization. In the remaining patients with confirmed coronary artery disease and moderate angina symptoms, either PCI first or optimal medical therapy first is an appropriate initial strategy that considers coronary anatomy, symptom burden, and patient desires.
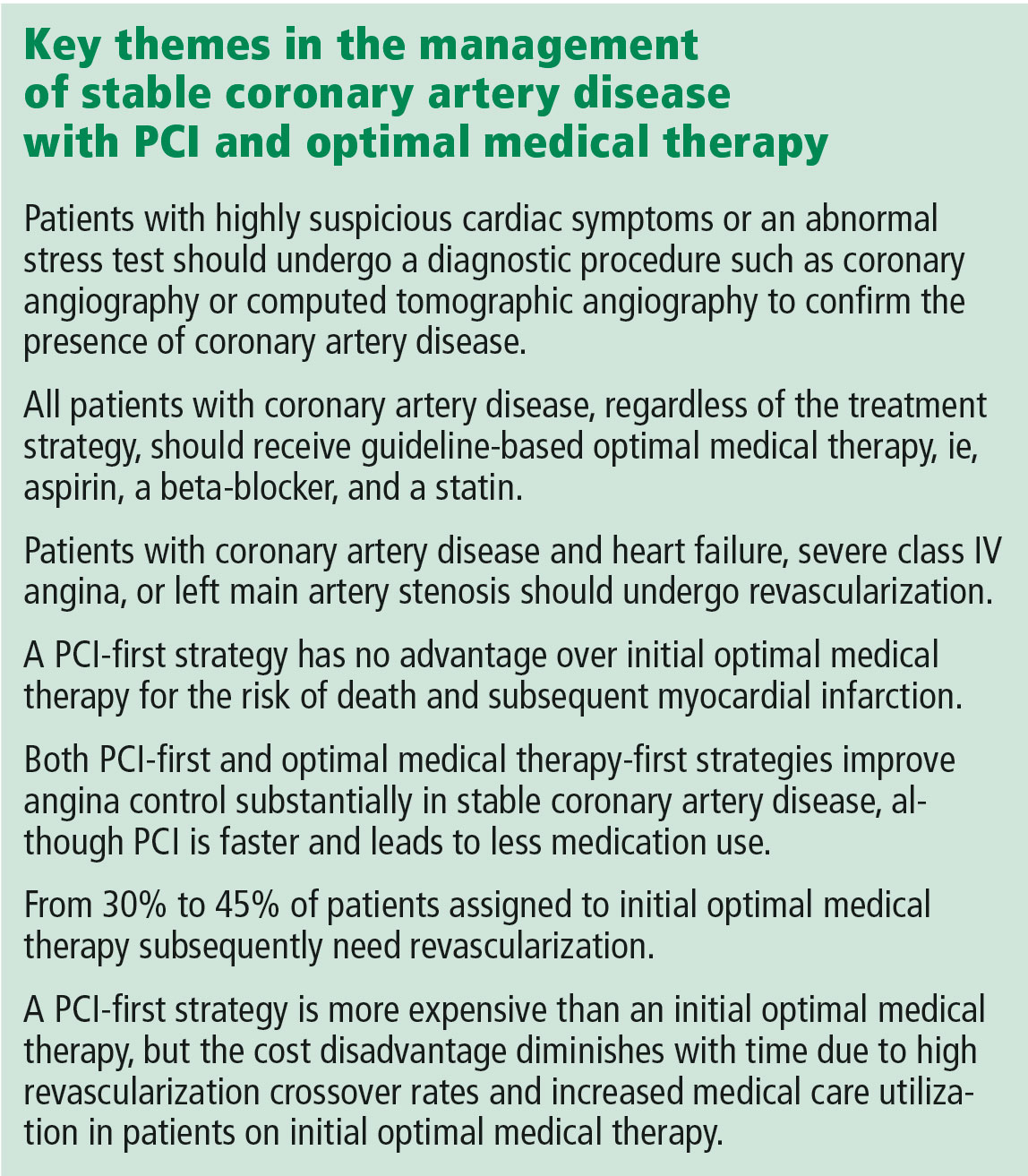
Invented by Andreas Grüntzig in 1977, percutaneous coronary intervention (PCI) has revolutionized the management of coronary artery disease.1 Initially, PCI was more attractive than conventional revascularization with coronary artery bypass grafting because it was less invasive, but as time went on PCI acquired its own evidence base of improved clinical outcomes. In fact, for ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, and cardiogenic shock, there is clear evidence that PCI saves lives in both the short and long term.2,3
But PCI is also used widely in stable coronary artery disease, and in contrast to the clear-cut benefit in the acute conditions noted above, a series of reports culminating in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial has shown that PCI in stable coronary artery disease does not reduce the risk of death or of subsequent myocardial infarction.4,5 Cardiologists have heeded the COURAGE trial findings in their clinical decision-making, and the rate of PCI for stable coronary artery disease dropped by 60% from 2006 to 2011.6
In an article in this issue,7 Dr. Michael Rothberg describes a 55-year-old man who develops new-onset angina and then undergoes a Bruce protocol stress test that is stopped at 6 minutes due to chest pain and ST-segment depression. Dr. Rothberg argues that, based on COURAGE trial data, this patient and other patients with stable coronary artery disease should not be treated with PCI but instead should receive optimal medical therapy.
KEY ISSUES ABOUT THE COURAGE TRIAL
To understand the applicability of the results of the COURAGE trial to patient care, it is important to examine a number of key issues about this trial.
First, COURAGE enrolled a narrow group of patients with stable coronary artery disease and excluded many common patient subgroups, such as those with heart failure, severe anginal symptoms, or left main artery stenosis, who would benefit from revascularization.5 Specifically, for every 100 patients enrolled in COURAGE, 161 were excluded for having heart failure, 39 were excluded for class IV angina, and 31 were excluded for left main stenosis.
Second, although COURAGE has been described as a trial of PCI vs optimal medical therapy, it was not. Rather, it was a trial of optimal medical therapy with PCI first vs optimal medical therapy with crossover PCI if medical therapy failed.5 The crossover rate was not insubstantial: 16.1% of the patients in the medical therapy group underwent PCI by the end of the first year, increasing to 32.6% at a median of 4.6 years of follow-up.5,7 And patients with more intense and frequent angina and resulting worse quality of life were the ones who required crossover PCI.8
Third, it has been proposed that patients with suspicious cardiac symptoms or abnormal stress test findings can be managed with optimal medical therapy initially, based on the COURAGE findings. However, the COURAGE trial required diagnostic angiography both to confirm underlying coronary artery disease and to exclude left main disease.5 Thus, regardless of one’s position on the role of PCI in stable coronary artery disease, diagnostic investigation by cardiac catheterization or computed tomographic angiography to confirm the presence or absence of coronary artery disease remains mandatory.
Fourth, optimal medical therapy was prescribed by the trial’s protocol, so that one would expect that both treatment groups received similar levels of optimal medical therapy. However, the optimal medical therapy group required more medications to achieve the same outcome as the PCI group.5
Finally, although it has been reported that the COURAGE trial showed no benefit for PCI, in fact, for the outcome of symptom relief, initial PCI was clearly superior to optimal medical therapy beginning at 3 months and extending out to 24 months—a result for which the magnitude of benefit is underestimated due to the occurrence of crossover PCI.9 In particular, women and patients with a high frequency of angina derived improvement in angina-related quality of life from PCI compared with optimal medical therapy.8,10
A MORE NUANCED INTERPRETATION
For these reasons, the role of PCI in stable coronary disease is more nuanced than simply stating that the COURAGE trial results were “negative” for PCI. It is more accurate to say that in selected patients with moderate symptoms of angina and without heart failure or left main artery disease, a PCI-first strategy has no advantage over an optimal medical treatment-first strategy for the risk of death and myocardial infarction but does lead to earlier angina relief and less long-term need for medication. In addition, in up to one-third of cases, an optimal medical treatment-first strategy fails and requires crossover to PCI.5
Dr. Rothberg is correct in highlighting the crucial importance of optimal medical therapy in the management of stable coronary artery disease. In fact, cardiologists strive to prescribe optimal medical treatment for all coronary artery disease patients irrespective of treatment strategy. However, 3 important issues in his analysis need to be highlighted.
Controlling symptoms is important, and we should not underrate it. The patient described in Dr. Rothberg’s article could exercise for only 6 minutes on a Bruce treadmill test, indicating a quite limited functional capacity of only 5.8 metabolic equivalents of the task (METs).11 (A healthy 55-year-old man should be able to achieve 10.5 METs.12) Inability to achieve 6 METs precludes the ability to dance, to ride a bike at a moderate pace, or to go on a hike.13 For many patients, these limitations are serious and important concerns for their lifestyle and quality of life. PCI has been shown to be superior to medical therapy in improving functional capacity, improving it by 20% vs 2% in one trial14 and 26% vs 7% in a second trial.14 Patients undergoing PCI were twice as likely to have a greater than 2-minute increase in exercise capacity.15 Recognizing the importance of symptom control in stable coronary artery disease is patient-centered care.
Patient decision-making is complicated, and we should not assume that patients choose PCI primarily to reduce their risk of death. A randomized trial showed that patients continued to select PCI as initial treatment even when they clearly knew that it would not prevent death or myocardial infarction.16 As noted above, patients may value earlier symptom relief, particularly if their angina is frequent or limiting. In addition, patients strongly desire to minimize medical therapy and may be willing to trade decreased life expectancy to reduce the need to take medications.17 Finally, some patients may want to be able to continue to participate in certain lifestyle activities.
PCI is expensive, but less so over the long run. With a PCI-first strategy, costs are front-loaded, and studies with short-term follow-up show a marked increase in cost. However, long-term follow-up shows that the cost differences diminish dramatically due to high rates of crossover to revascularization and increased medical care in the optimal medical therapy arm. The cumulative lifetime costs in the COURAGE trial with a PCI-first strategy, although statistically significant, were only 10% higher than with the optimal medical treatment-first strategy ($99,820 vs $90,370).18 Therefore, substantial long-term cost-savings by shifting from an initial PCI strategy to initial optimal medical therapy are unlikely to be delivered when measured over the long term.
NEWER TRIALS SUPPORT A BALANCED APPROACH
The most recent studies of the management of stable coronary artery disease support a balanced approach.
The ORBITA trial (Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina), on one hand, showed limited benefit of PCI vs medical therapy in patients with single-vessel coronary artery disease, preserved functional capacity, and mild symptoms.19 There was no significant improvement in exercise capacity or angina frequency, although baseline angina frequency after medical stabilization was quite low.
The FAME 2 trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation), on the other hand, studied patients with positive fractional flow reserve coronary artery disease (ie, using an invasive technique to confirm the hemodynamic significance of the coronary stenosis) and showed markedly better outcomes with PCI than with medical therapy.20 Specifically, the PCI-first group had improved quality of life and dramatically less need for urgent revascularization.
Furthermore, as in the COURAGE trial, the optimal medical therapy group had a high crossover rate to PCI (44.2%), leading to the complete elimination of the early cost advantage of medical therapy by 3 years. The initial costs with PCI vs medical therapy were $9,944 vs $4,439 (P < .001); the 3-year costs were $16,792 vs $16,737 (P = .94).
For these reasons, a balanced approach to recommending PCI first vs optimal medical treatment first remains the best strategy.
TOWARD PATIENT-CENTERED CARE
For the 55-year-old patient in Dr. Rothberg’s article, the first step in making an appropriate decision would be to understand the severity of symptoms relative to the patient’s lifestyle. The second step is to assess the patient’s interest in an invasive procedure such as PCI relative to optimal medical therapy, as the patient may have a strong preference for one option or the other.
Finally, with the understanding that there is no difference in hard end points of myocardial infarction and death, a balanced discussion of the advantages and disadvantages of both PCI and optimal medical therapy would be needed. For PCI, advantages include earlier symptom control and improved quality of the life, particularly if symptoms are severe, with disadvantages of an invasive procedure with its attendant risks. For optimal medical therapy, advantages include improved symptom control and avoidance of an invasive procedure, while disadvantages include increased medication use and a high rate of eventual crossover to PCI. This important discussion integrating both patient and medical perspectives ultimately leads to the best decision for the individual patient.
A patient-centered approach to clinical decision-making mandates inclusion of PCI first as an option in the management of stable coronary artery disease. After confirming the patient has coronary artery disease, patients with heart failure, class IV angina at rest, or left main artery stenosis should be referred for revascularization. In the remaining patients with confirmed coronary artery disease and moderate angina symptoms, either PCI first or optimal medical therapy first is an appropriate initial strategy that considers coronary anatomy, symptom burden, and patient desires.
- Meier B. The first patient to undergo coronary angioplasty—23-year follow-up. N Engl J Med 2001; 344:144–145.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011; 124:2574–2609.
- Fox KAA, Clayton TC, Damman P, et al. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol 2010; 55:2435–2445.
- Katritsis DG, Ioannidis JPA. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation 2005; 111:2906–2912.
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Bangalore S, Gupta N, Généreux P, Guo Y, Pancholy S, Feit F. Trend in percutaneous coronary intervention volume following the COURAGE and BARI-2D trials: insight from over 8.1 million percutaneous coronary interventions. Int J Cardiol 2015; 183:6–10.
- Rothberg MB. PCI for stable angina: a missed opportunity for shared decision-making. Cleve Clin J Med 2018; 85:105–121.
- Spertus JA, Maron DJ, Cohen DJ, et al. Frequency, predictors, and consequences of crossing over to revascularization within 12 months of randomization to optimal medical therapy in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial. Circ Cardiovasc Qual Outcomes 2013; 6:409–418.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Acharjee S, Teo KK, Jacobs AK, et al. Optimal medical therapy with or without percutaneous coronary intervention in women with stable coronary disease: a pre-specified subset analysis of the Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation (COURAGE) trial. Am Heart J 2016; 173:108–117.
- Foster C, Jackson AS, Pollock ML, et al. Generalized equations for predicting functional capacity from treadmill performance. Am Heart J 1984; 107:1229–1234.
- Morris CK, Myers J, Froelicher VF, Kawaguchi T, Ueshima K, Hideg A. Nomogram based on metabolic equivalents and age for assessing aerobic exercise capacity in men. J Am Coll Cardiol 1993; 22:175–182.
- Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 1990; 13:555–565.
- Erne P, Schoenenberger AW, Burckhardt D, et al. Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial. JAMA 2007; 297:1985–1991.
- Strauss WE, Fortin T, Hartigan P, Folland ED, Parisi AF. A comparison of quality of life scores in patients with angina pectoris after angioplasty compared with after medical therapy. Outcomes of a randomized clinical trial. Veterans Affairs Study of Angioplasty Compared to Medical Therapy Investigators. Circulation 1995; 92:1710–1719.
- Coylewright M, Dick S, Zmolek B, et al. PCI choice decision aid for stable coronary artery disease: a randomized trial. Circ Cardiovasc Qual Outcomes 2016; 9:767–776.
- Fontana M, Asaria P, Moraldo M, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation 2014; 129:2539–2546.
- Weintraub WS, Boden WE, Zhang Z, et al. Cost-effectiveness of percutaneous coronary intervention in optimally treated stable coronary patients. Circ Cardiovasc Qual Outcomes 2008; 1:12–20.
- Al-Lamee R, Thompson D, Dehbi H-M, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet November 2, 2017; doi:10.1016/S0140-6736(17)32714-9.
- Fearon WF, Nishi T, Bruyne BD, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: three-year follow-up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation November 2017; doi:10.1161/CIRCULATIONAHA.117.031907.
- Meier B. The first patient to undergo coronary angioplasty—23-year follow-up. N Engl J Med 2001; 344:144–145.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011; 124:2574–2609.
- Fox KAA, Clayton TC, Damman P, et al. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol 2010; 55:2435–2445.
- Katritsis DG, Ioannidis JPA. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation 2005; 111:2906–2912.
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Bangalore S, Gupta N, Généreux P, Guo Y, Pancholy S, Feit F. Trend in percutaneous coronary intervention volume following the COURAGE and BARI-2D trials: insight from over 8.1 million percutaneous coronary interventions. Int J Cardiol 2015; 183:6–10.
- Rothberg MB. PCI for stable angina: a missed opportunity for shared decision-making. Cleve Clin J Med 2018; 85:105–121.
- Spertus JA, Maron DJ, Cohen DJ, et al. Frequency, predictors, and consequences of crossing over to revascularization within 12 months of randomization to optimal medical therapy in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial. Circ Cardiovasc Qual Outcomes 2013; 6:409–418.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Acharjee S, Teo KK, Jacobs AK, et al. Optimal medical therapy with or without percutaneous coronary intervention in women with stable coronary disease: a pre-specified subset analysis of the Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation (COURAGE) trial. Am Heart J 2016; 173:108–117.
- Foster C, Jackson AS, Pollock ML, et al. Generalized equations for predicting functional capacity from treadmill performance. Am Heart J 1984; 107:1229–1234.
- Morris CK, Myers J, Froelicher VF, Kawaguchi T, Ueshima K, Hideg A. Nomogram based on metabolic equivalents and age for assessing aerobic exercise capacity in men. J Am Coll Cardiol 1993; 22:175–182.
- Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 1990; 13:555–565.
- Erne P, Schoenenberger AW, Burckhardt D, et al. Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial. JAMA 2007; 297:1985–1991.
- Strauss WE, Fortin T, Hartigan P, Folland ED, Parisi AF. A comparison of quality of life scores in patients with angina pectoris after angioplasty compared with after medical therapy. Outcomes of a randomized clinical trial. Veterans Affairs Study of Angioplasty Compared to Medical Therapy Investigators. Circulation 1995; 92:1710–1719.
- Coylewright M, Dick S, Zmolek B, et al. PCI choice decision aid for stable coronary artery disease: a randomized trial. Circ Cardiovasc Qual Outcomes 2016; 9:767–776.
- Fontana M, Asaria P, Moraldo M, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation 2014; 129:2539–2546.
- Weintraub WS, Boden WE, Zhang Z, et al. Cost-effectiveness of percutaneous coronary intervention in optimally treated stable coronary patients. Circ Cardiovasc Qual Outcomes 2008; 1:12–20.
- Al-Lamee R, Thompson D, Dehbi H-M, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet November 2, 2017; doi:10.1016/S0140-6736(17)32714-9.
- Fearon WF, Nishi T, Bruyne BD, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: three-year follow-up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation November 2017; doi:10.1161/CIRCULATIONAHA.117.031907.
