User login
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
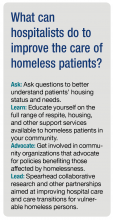
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.
Despite programs to end homelessness, it remains a substantial and growing problem in many cities in the United States.1,2 In 2016, there were an estimated 10,550 homeless people living in my home state of Colorado, a 6% increase from the prior year.2 A recent point-estimate study found that there were more than 5,000 homeless individuals in the Denver metropolitan area on a single night in January 2017.3 Because of the relative scarcity of housing, a growing number of cities like Denver now utilize a practice known as vulnerability indexing to prioritize homeless persons at high risk of mortality from medical conditions for placement in permanent supportive housing.4
Although hospitalists like myself frequently care for vulnerable homeless patients in the hospital, most have little formal training in how best to care for and advocate for these individuals beyond treating their acute medical need, and little direct contact with community organizations with expertise in doing so. Instead, we have learned informally through experience. Hospital providers are often frustrated by the perceived lack of services and support available to these patients, and there is substantial variability in the extent to which providers engage patients and community partners during and after hospitalization. Despite the growing practice of vulnerability indexing in the community, hospital-based providers do not routinely assess vulnerability with respect to housing. Previous research indicates that housing status is assessed in only a minority of homeless patients during their hospital stay.12 Thus, hospitalization often represents a missed opportunity to identify vulnerability and utilize it to connect patients with housing and other resources.
Addressing the significant known health disparities faced by homeless persons is one of the greatest health equity challenges of our time.13 We need better ways of understanding, identifying, and addressing vulnerability among homeless patients who are hospitalized, paired with improved integration with local community organizations. This will require moving beyond the idea that homelessness is the social worker’s job to one of shared responsibility and advocacy.
Collaborative research and other partnerships that engage both community organizations and individuals affected by homelessness are crucial to further understand the specific needs, barriers, challenges, and opportunities for improving hospital care and care transitions in this population. As well-respected community members and systems thinkers who witness these inequities on a daily basis, hospitalists are well positioned to help lead this work.
Dr. Stella is a hospitalist at Denver Health and Hospital Authority, and an associate professor of medicine at the University of Colorado. She is a member of The Hospitalist editorial advisory board.
References
1. Ending Chronic Homelessness. (Aug 2017). U.S. Interagency Council on Homelessness. Available at: https://www.usich.gov/goals/chronicsness. Accessed: Oct 21, 2017.
2. 2016 Annual Homeless Assessment Report (AHAR) to Congress. (Nov 2016). U.S. Department of Housing and Urban Development Office of Community Planning and Development, Part 1. Available at: https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Accessed: Oct 21, 2017.
3. 2017 Point-In-Time Report, Seven-County Metro Denver Region. Metro Denver Homeless Initiative. Available at: http://www.mdhi.org/2017_pit. Accessed Oct 22, 2017.
4. Henwood BF et al. Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health. 2015;15:1209.
5. Weinstein LC et al. Moving from street to home: Health status of entrants to a Housing First program. J Prim Care Community Health. 2011;2:11–5.
6. Kushel MB et al. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200-6.
7. Kushel MB et al. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92(5):778-84.
8. Baggett TP et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013 Feb 11;173(3):189–95.
9. Johnson et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015 Aug;34(8):1312-9.
10. Durfee J et al. The impact of tailored intervention services on charges and mortality for adult super-utilizers. Healthc (Amst). 2017 Aug 25. pii: S2213-0764(17)30057-X. doi: 10.1016/j.hjdsi.2017.08.004. [Epub ahead of print]
11. Rinehart DJ et al. Identifying subgroups of adult super utilizers in an urban safety-net system using latent class analysis: Implications for clinical practice. Med Care. 2016 Sep 14. doi: 10.1097/MLR.0000000000000628. [Epub ahead of print]
12. Greysen RS et al. Understanding transitions of care from hospital to homeless shelter: A mixed-methods, community-based participatory approach. J Gen Intern Med. 2012;27(11):1484-91.
13. National Health Care for the Homeless Council. (Oct 2012). Improving Care Transitions for People Experiencing Homelessness. (Lead author: Sabrina Edgington, policy and program specialist.) Available at: www.nhchc.org/wp-content/uploads/2012/12/Policy_Brief_Care_Transitions.pdf. Accessed Oct 21, 2017.
14. Koh HK et al. Improving healthcare for homeless people. JAMA. 2016;316(24):2586-7.