User login
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
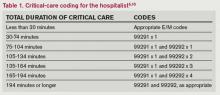
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.