User login
Antipsychotics have long been linked with hyperprolactinemia.1 This phenomenon was first considered a drug class effect, but the arrival of clozapine, better deliniation of dopamine receptor subtypes, and identification of the four principal CNS dopamine pathways revealed that hyperprolactinemia was not a universal consequence of antipsychotic use.
We now know that most atypical antipsychotics are less likely to induce hyperprolactinemia than older antipsychotics, but we don’t know why. The most likely explanation is that most of the newer agents block dopamine D2 minimally in the hypothalamic tuberoinfundibular pathway.2 Evidence is emerging that atypical agents elevate serum prolactin levels at least transiently—but usually less than typical antipsychotics—and this effect varies, depending on each compound’s dopamine-binding properties.
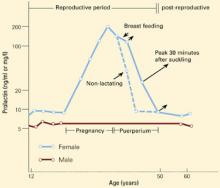
Figure 1 CHANGES IN PROLACTIN LEVELS OVER TIME
Mean serum prolactin concentrations from puberty until menopause. For nursing women, the length of the arrows depicts the increase in serum prolactin concentration associated with each episode of suckling. The Y-axis expresses serum prolactin concentration in both ng/ml and mg/l.
Source: Adapted and reprinted with permission from Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
Prolactin physiology
Prolactin—a large peptide containing 198 amino acids—was the first anterior pituitary gland hormone to be isolated in pure form.3 Despite its molecular weight of approximately 23,000, the hormone easily crosses the blood-brain barrier.4
Similar to other anterior pituitary hormones, prolactin is secreted episodically. Its secretion is inhibited by dopamine release from the hypothalamus and enhanced by different prolactin-releasing factors. Prolactin is the only anterior pituitary hormone that is produced by tuberoinfundibular neurons governed by dopamine.5 Dopamine stimulates lactotrope D2 receptors and inhibits adenylate cyclase, resulting in reduced prolactin synthesis and release.
Serum prolactin concentrations change during various life stages (Figure 1).6 Estrogen’s effects on prolactin gene expression regulate prolactin synthesis, resulting in higher prolactin levels in premenopausal women than in men.
Prolactin secretion
Normally, prolactin is secreted in pulses—approximately 14 in a 24-hour period, with an interpulse interval of about 80 minutes.5 A bimodal daily pattern of secretion is superimposed upon this pattern, with peak levels at night and trough levels at noon. Stress—including surgery and general anesthesia, exercise, and hypoglycemia—may transiently increase prolactin levels.
Endocrine regulation. Estrogen modulates the response of hypothalamic factors that control prolactin production. It stimulates decreased prolactin response to dopamine and increased response to thyrotropic-releasing hormone.
Insulin also stimulates prolactin secretion—probably by inducing hypoglycemia. Serum insulin level changes within physiologic ranges appear to affect prolactin regulation.
Neuroendocrine regulation. The hypothalamus blunts prolactin secretion primarily via dopamine release. This modulation occurs principally within the tuberoinfundibular dopamine pathway. The D2 subtype is the only dopamine receptor in the anterior pituitary gland:
- a decrease in dopamine levels reaching the anterior pituitary gland increases the number of D2 receptors
- to a lesser extent, estrogen decreases the number of D2 receptors.
Dopamine-modulated reductions in action potential discharge from lactotrophs and in calcium flux leads to decreased intracellular calcium and decreased prolactin secretion.5
Most hormones are target-organ agents and are regulated via a feedback loop that includes the peripheral circulation. Prolactin, however, is not considered to have a specific target organ. It is its own inhibiting factor, using an autoregulatory, pituitary-to-hypothalamus short-loop feedback circuit.
For example, prolactin-secreting tumors or drugs that elevate hormone levels lead to an increase in dopamine. In contrast, hypophysectomy decreases dopamine. In this setting, prolactin injections will restore normal dopamine levels. Prolactin-releasing factors include thyrotropic-releasing hormone, vasoactive intestinal peptide, and serotonin.
Prolactin’s actions
Many tissues—including breast, liver, ovary, testis, and prostate—have prolactin receptors. These receptors are stimulated with equal potency by prolactin and growth hormone.
The principal site of prolactin action is the mammary gland, where the hormone initiates and maintains lactation after childbirth. Major stimuli for breast development are estrogen, progesterone, prolactin, and placental mammotropic hormones. Other stimuli include insulin, cortisol, and thyroid hormone.7
Gonadotropin secretion is influenced by prolactin via the hypothalamus. Prolactin-mediated inhibition of luteinizing hormone-releasing hormone secretion impairs gonadotropin release and inhibits gonadal function.
Table 1
COMMON CLINICAL EFFECTS IN PATIENTS WITH HYPERPROLACTINEMIA
| Organ or syndrome | Clinical effects |
|---|---|
| Behavior | Direct effects Secondary effects due to hypogonadism Possible cognitive impairment |
| Bones | Decreased bone mineral density due to testosterone or estrogen deficits |
| Breast | Engorgement Lactation unrelated to breast feeding |
| Cardiovascular system | Possible adverse effects due to low levels of testosterone or estrogen |
| Menstrual function | Absence of ovulation Amenorrhea |
| Sexual function | Reduced libido Reduced arousal Orgasmic dysfunction |
| Source: Adapted and reprinted with permission from Dickson RA, Glazer WM. Neurolepticinduced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86. | |
Diagnosis of hyperprolactinemia
Pathologic hyperprolactinemia is defined as consistently elevated serum prolactin concentration (>20 ng/ml) in the absence of pregnancy or postpartum lactation. Because of the pulsatile nature of prolactin secretion, a definitive diagnosis of hyperprolactinemia requires three serum prolactin levels taken on different mornings.
Clinical presentation. Hyperprolactinemia—the most common hypothalamic-pituitary disturbance—usually presents with clinical features of gonadal dysfunction (Table 1).8 Symptoms and signs related to a brain mass—headache, visual field disturbances, ophthalmoplegia, and reduced visual acuity—may predominate with a large pituitary tumor. The patient may first present to a primary care physician or to a clinical specialist, such as a gynecologist, neurologist, ophthalmologist, pediatrician, psychiatrist, or urologist.
Thirty to 80% of women with hyperprolactinemia develop galactorrhea,9 although some women with galactorrhea have normal prolactin levels. Men with hyperprolactinemia usually have gonadal dysfunction, which unfortunately is often attributed to “psychogenic” causes. Particularly in men, prolactin is implicated in the control of libido.
Causes. Hyperprolactinemia may be caused by any process that inhibits dopamine synthesis, the neurotransmitter’s transport to the anterior pituitary gland, or its action at the lactotrope dopamine receptors ( Table 2).9 In this article, we will limit our discussion to antipsychotic drugs. have long-term effects on bone density. Trabecular bone mass
Estrogen and prolactin. During pregnancy, the rise in estrogen levels probably stimulates an increase in prolactin. Increased prolactin levels are also found in women taking estrogen-containing oral contraceptives, although this effect is very small with low-estrogen formulations.
Table 2
CAUSES OF PATHOLOGIC HYPERPROLACTINEMIA
| Hypothalamic disease | Tumor, infiltrative disease, pseudotumor cerebri, cranial radiation |
| Pituitary disease | Prolactinoma, acromegaly, Cushing’s disease, glycoprotein-producing tumor, other tumors, pituitary stalk section, empty sella, infiltrative disease |
| Medications | Antipsychotics, dopamine receptor blockers, antidepressants, antihypertensives, estrogens, opiates, cimetidine |
| Others | Primary hypothyroidism, chronic renal failure, cirrhosis, neurogenic and idiopathic causes |
| Source: Adapted and reprinted from Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders, 1995:394-405. Copyright 1995, with permission from Elsevier Science. | |
Functions of the pituitary lactotrophs regulated by estrogen include prolactin gene expression, release, storage, and cellular expression.2 Estradiol inhibition of dopamine synthesis in the tuberoinfundibular dopaminergic neurons may contribute to some gender differences in neurocognitive function and to psychiatric conditions’ clinical features.
Hyperprolactinemia and bone density. Besides causing galactorrhea and sexual dysfunction, hyperprolactinemia may has been found to be reduced in young women with amenorrhea secondary to hyperprolactinemia. This trabecular osteopenia is reversible—spinal bone density decreases progressively without treatment and improves when hyperprolactinemia is treated. Menstrual function appears to best predict risk of progressive spinal osteopenia in women with hyperprolactinemia. Estradiol level is a stronger predictor of clinical course than is the prolactin level.10
Antipsychotic drugs and hyperprolactinemia
Among the four principal dopamine pathways in the brain, the tuberoinfundibular pathway is a system of short axons at the base of the hypothalamus that releases dopamine into the portal veins of the pituitary gland. Terminals in the median eminence of the hypothalamus release dopamine that travels down the pituitary stalk in the portal veins.
Typical antipsychotics block dopamine receptors both in the striatum and in the hypothalamus.11 This finding suggests that the older drugs lack specificity of dopamine blockade. Prolactin elevations in patients treated with older antipsychotics may be associated with sexual dysfunction—a common cause of drug noncompliance, particularly in men.12
Antipsychotics and sexual side effects. Patients taking antipsy-chotics often complain—spontaneously or after focused questioning—of sexual side effects caused by drug-induced hyperprolactinemia. Assessing antipsychotic-induced sexual dysfunction may be confounded by the psychoses being treated, patient compliance, and sexuality’s complexities. Antipsychotics are generally believed to reduce desire, cause orgasmic dysfunction, and lead to difficulties during sexual performance.8
Atypical antipsychotics
A recent study designed to assess the effect of three atypical antipsychotics on serum prolactin levels enrolled 18 men with schizophrenia (mean age 32) taking clozapine, 300 to 400 mg/d; risperidone, 1 to 3 mg/d; or olanzapine, 10 to 20 mg/d, for at least 8 weeks.13 The study participants were instructed not to take their antipsychotics the night before the study. Baseline prolactin levels were measured in the morning, the men took the full daily dose of their medications, and prolactin levels were measured every 60 minutes over the next 8 hours and again at 24 hours.
Mean baseline prolactin values of clozapine (9 ng/ml, SD=5) and olanzapine (9 ng/ml, SD=5) were in the normal range (<20 ng/ml), compared with those of risperidone (27 ng/ml, SD=14). Three of the six patients taking risperidone had hyperprolactinemia at baseline. Prolactin values doubled within 6 hours of administration of all three medications. There was no comparable increase in prolactin levels in five control subjects not taking antipsychotics.
The authors concluded that these atypical antipsychotics raise prolactin levels but more transiently than typical antipsychotics. They suggested that the differences among the three drugs may be attributed to each drug’s binding properties to pituitary dopamine D2 receptors. A similar study in four patients with first-episode schizophrenia found serum prolactin levels increased from <10 ng/ml at baseline to peak levels of 80 to 120 ng/ml within 60 to 90 minutes after patients took a full daily dose of quetiapine, 700 to 800 mg/d.14
Risperidone. A study sponsored by Janssen Pharmaceutica15 reviewed the manufacturer’s experience with prolactin and its potential to induce side effects, using data from premarketing studies comparing risperidone with haloperidol. Amenorrhea and galactorrhea were assessed in women; ejaculatory dysfunction, erectile dysfunction, and gynecomastia were assessed in men.
Table 3
HYPERPROLACTINEMIA-RELATED SIDE EFFECTS REPORTED BY PATIENTS TAKING RISPERIDONE AND OLANZAPINE
| Gender and complaint | Taking risperidone (%) | Taking olanzapine (%) | Difference (P-value) |
|---|---|---|---|
| Women | |||
| Galactorrhea | 11 of 47 (23.4%) | 11 of 49 (22.4%) | 1.00 |
| Amenorrhea | 11 of 46 (23.9%) | 9 of 45 (20.0%) | 0.80 |
| Men | |||
| Gynecomastia | 9 of 115 (7.8%) | 4 of 115 (3.5%) | 0.25 |
| Sexual dysfunction | 36 of 115 (31.3%) | 34 of 114 (29.8%) | 0.89 |
| Source: Adapted and reprinted with permission from Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry2001;158:765-74. | |||
Both risperidone and haloperidol were associated with dose-related increases in plasma prolactin concentration in men and women. In women, neither risperidone dosage nor end-point prolactin concentrations were correlated with adverse events. In men:
- adverse events did not correlate with plasma prolactin concentrations
- the incidence of adverse events was dose-related
- the incidence of adverse events associated with risperidone, 4 to 10 mg/d, was not significantly greater than in patients taking placebo.
Another Janssen-sponsored study compared potential hyperprolactinemia-related side effects of risperidone and olanzapine but did not report prolactin concentrations. The authors found no significant differences between the drugs, based on breast features/menstrual changes in women and chest features/sexual dysfunction in men (Table 3).16
Olanzapine. A study sponsored by Eli Lilly and Co.17 assessed the effects of olanzapine on prolactin concentration in women previously treated with risperidone. The authors enrolled 20 Korean women with schizophrenia treated with risperidone (mean dosage 3.5 mg/d) and complaining of menstrual disturbances, galactorrhea, and/or sexual dysfunction. The mean serum prolactin concentration with risperidone was 132.2 ng/ml.
Over 2 weeks, patients were switched from risperidone to olanzapine (mean dosage 9.1 mg/d). After 8 weeks, the mean serum prolactin concentration was measured at 23.4 ng/ml. The authors noted improved menstrual function and reduced sexual side effects with olanzapine.
Conclusion
The package inserts of all atypical antipsychotics list hyperprolactinemia as a potential risk in patients taking these medications. The clinical significance of hyperprolactinemia associated with antipsychotic use is being explored but requires further elucidation.
Based on our understanding of the long-term course of untreated hyperprolactinemia—derived largely from patients not taking antipsychotics—it seems reasonable to ask patients taking atypical antipsychotics at least once a year about chest/breast complaints and sexual dysfunction. This recommendation would seem particularly relevant in patients taking risperidone at dosages >6 mg/d for sustained periods. In the absence of specific complaints, hyperprolactinemia associated with risperidone should be evaluated case by case, including perhaps endocrinology consultation.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
- Smith S, Wheeler MJ, Murray R, O’Keane V. The effects of antipsychotic-induced hyperprolactinemia on the hypothalamic-pituitary-gonadal axis. J Clin Psychopharmacol 2002;22(2):109-14. Available at: http://www.psychiatry.wustl.edu/Resources/LiteratureList/2002/May/Smith.PDF.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Vieweg reports that he is on the speakers bureau of Janssen Pharmaceutica, Eli Lilly and Co., Pfizer Inc., Wyeth Pharmaceuticals, Forest Pharmaceuticals, and GlaxoSmithKline.
Dr. Fernandez reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Clemens JA, Smalstig EB, Sawyer BD. Antipsychotic drugs stimulate prolactin release. Psychopharmacol. 1974;40:123-7.
2. Petty RG. Prolactin and antipsychotic medications: mechanism of action. Schizophr Res 1999;35(suppl):S67-S73.
3. West ES, Todd WR. The hormones. In: West ES, Todd WR (eds). Textbook of biochemistry. New York: The Macmillan Co., 1961;1315-54.
4. Belchetz PE, Ridley RM, Baker HF. Studies on the accessibility of prolactin and growth hormone to brain: effect of opiate agonists on hormone levels in serial, simultaneous plasma and cerebrospinal fluid samples in the rhesus monkey. Brain Res 1982;239:310-4.
5. Cooke NE. Prolactin: basic physiology. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Company, 1995;368-93.
6. Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
7. Thorner MO, Vance ML, Laws ER, Horvath E, Kovacs K. The anterior pituitary. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR (eds). Williams textbook of endocrinology. Philadelphia: W.B. Saunders Co., 1998;249-340.
8. Dickson RA, Glazer WM. Neuroleptic-induced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86.
9. Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Co., 1995;394-405.
10. Biller BM, Baum HB, Rosenthal DI, Saxe VC, Charpie PM, Kilibanski A. Progressive trabecular osteopenia in women with hyperprolactinemic amenorrhea. J Clin Endocrinol Metab 1992;75:692-7.
11. Baron JC, Martinot JL, Cambon H, et al. Striatal dopamine receptor occupancy during and following withdrawal from neuroleptic treatment: correlative evaluation by positron emission tomography and plasma prolactin levels. Psychopharmacol 1989;99:463-72.
12. Ghadirian AM, Chouinard G, Annable L. Sexual dysfunction and plasma prolactin levels in neuroleptic-treated schizophrenic outpatients. J Nerv Ment Dis 1982;170:463-7.
13. Turrone P, Kapur S, Seeman MV, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry 2002;159:133-5.
14. Alexiadis M, Whitehorn D, Woodley H, Kopala L. Prolactin elevation with quetiapine (letter). Am J Psychiatry 2002;159(Sept):1608-9.
15. Kleinberg DL, Davis JM, De Coster R, Van Baelen B, Brecher M. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
16. Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 2001;158:765-74.
17. Kim K, Pae C, Chae J, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63:408-13.
Antipsychotics have long been linked with hyperprolactinemia.1 This phenomenon was first considered a drug class effect, but the arrival of clozapine, better deliniation of dopamine receptor subtypes, and identification of the four principal CNS dopamine pathways revealed that hyperprolactinemia was not a universal consequence of antipsychotic use.
We now know that most atypical antipsychotics are less likely to induce hyperprolactinemia than older antipsychotics, but we don’t know why. The most likely explanation is that most of the newer agents block dopamine D2 minimally in the hypothalamic tuberoinfundibular pathway.2 Evidence is emerging that atypical agents elevate serum prolactin levels at least transiently—but usually less than typical antipsychotics—and this effect varies, depending on each compound’s dopamine-binding properties.
Figure 1 CHANGES IN PROLACTIN LEVELS OVER TIME
Mean serum prolactin concentrations from puberty until menopause. For nursing women, the length of the arrows depicts the increase in serum prolactin concentration associated with each episode of suckling. The Y-axis expresses serum prolactin concentration in both ng/ml and mg/l.
Source: Adapted and reprinted with permission from Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
Prolactin physiology
Prolactin—a large peptide containing 198 amino acids—was the first anterior pituitary gland hormone to be isolated in pure form.3 Despite its molecular weight of approximately 23,000, the hormone easily crosses the blood-brain barrier.4
Similar to other anterior pituitary hormones, prolactin is secreted episodically. Its secretion is inhibited by dopamine release from the hypothalamus and enhanced by different prolactin-releasing factors. Prolactin is the only anterior pituitary hormone that is produced by tuberoinfundibular neurons governed by dopamine.5 Dopamine stimulates lactotrope D2 receptors and inhibits adenylate cyclase, resulting in reduced prolactin synthesis and release.
Serum prolactin concentrations change during various life stages (Figure 1).6 Estrogen’s effects on prolactin gene expression regulate prolactin synthesis, resulting in higher prolactin levels in premenopausal women than in men.
Prolactin secretion
Normally, prolactin is secreted in pulses—approximately 14 in a 24-hour period, with an interpulse interval of about 80 minutes.5 A bimodal daily pattern of secretion is superimposed upon this pattern, with peak levels at night and trough levels at noon. Stress—including surgery and general anesthesia, exercise, and hypoglycemia—may transiently increase prolactin levels.
Endocrine regulation. Estrogen modulates the response of hypothalamic factors that control prolactin production. It stimulates decreased prolactin response to dopamine and increased response to thyrotropic-releasing hormone.
Insulin also stimulates prolactin secretion—probably by inducing hypoglycemia. Serum insulin level changes within physiologic ranges appear to affect prolactin regulation.
Neuroendocrine regulation. The hypothalamus blunts prolactin secretion primarily via dopamine release. This modulation occurs principally within the tuberoinfundibular dopamine pathway. The D2 subtype is the only dopamine receptor in the anterior pituitary gland:
- a decrease in dopamine levels reaching the anterior pituitary gland increases the number of D2 receptors
- to a lesser extent, estrogen decreases the number of D2 receptors.
Dopamine-modulated reductions in action potential discharge from lactotrophs and in calcium flux leads to decreased intracellular calcium and decreased prolactin secretion.5
Most hormones are target-organ agents and are regulated via a feedback loop that includes the peripheral circulation. Prolactin, however, is not considered to have a specific target organ. It is its own inhibiting factor, using an autoregulatory, pituitary-to-hypothalamus short-loop feedback circuit.
For example, prolactin-secreting tumors or drugs that elevate hormone levels lead to an increase in dopamine. In contrast, hypophysectomy decreases dopamine. In this setting, prolactin injections will restore normal dopamine levels. Prolactin-releasing factors include thyrotropic-releasing hormone, vasoactive intestinal peptide, and serotonin.
Prolactin’s actions
Many tissues—including breast, liver, ovary, testis, and prostate—have prolactin receptors. These receptors are stimulated with equal potency by prolactin and growth hormone.
The principal site of prolactin action is the mammary gland, where the hormone initiates and maintains lactation after childbirth. Major stimuli for breast development are estrogen, progesterone, prolactin, and placental mammotropic hormones. Other stimuli include insulin, cortisol, and thyroid hormone.7
Gonadotropin secretion is influenced by prolactin via the hypothalamus. Prolactin-mediated inhibition of luteinizing hormone-releasing hormone secretion impairs gonadotropin release and inhibits gonadal function.
Table 1
COMMON CLINICAL EFFECTS IN PATIENTS WITH HYPERPROLACTINEMIA
| Organ or syndrome | Clinical effects |
|---|---|
| Behavior | Direct effects Secondary effects due to hypogonadism Possible cognitive impairment |
| Bones | Decreased bone mineral density due to testosterone or estrogen deficits |
| Breast | Engorgement Lactation unrelated to breast feeding |
| Cardiovascular system | Possible adverse effects due to low levels of testosterone or estrogen |
| Menstrual function | Absence of ovulation Amenorrhea |
| Sexual function | Reduced libido Reduced arousal Orgasmic dysfunction |
| Source: Adapted and reprinted with permission from Dickson RA, Glazer WM. Neurolepticinduced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86. | |
Diagnosis of hyperprolactinemia
Pathologic hyperprolactinemia is defined as consistently elevated serum prolactin concentration (>20 ng/ml) in the absence of pregnancy or postpartum lactation. Because of the pulsatile nature of prolactin secretion, a definitive diagnosis of hyperprolactinemia requires three serum prolactin levels taken on different mornings.
Clinical presentation. Hyperprolactinemia—the most common hypothalamic-pituitary disturbance—usually presents with clinical features of gonadal dysfunction (Table 1).8 Symptoms and signs related to a brain mass—headache, visual field disturbances, ophthalmoplegia, and reduced visual acuity—may predominate with a large pituitary tumor. The patient may first present to a primary care physician or to a clinical specialist, such as a gynecologist, neurologist, ophthalmologist, pediatrician, psychiatrist, or urologist.
Thirty to 80% of women with hyperprolactinemia develop galactorrhea,9 although some women with galactorrhea have normal prolactin levels. Men with hyperprolactinemia usually have gonadal dysfunction, which unfortunately is often attributed to “psychogenic” causes. Particularly in men, prolactin is implicated in the control of libido.
Causes. Hyperprolactinemia may be caused by any process that inhibits dopamine synthesis, the neurotransmitter’s transport to the anterior pituitary gland, or its action at the lactotrope dopamine receptors ( Table 2).9 In this article, we will limit our discussion to antipsychotic drugs. have long-term effects on bone density. Trabecular bone mass
Estrogen and prolactin. During pregnancy, the rise in estrogen levels probably stimulates an increase in prolactin. Increased prolactin levels are also found in women taking estrogen-containing oral contraceptives, although this effect is very small with low-estrogen formulations.
Table 2
CAUSES OF PATHOLOGIC HYPERPROLACTINEMIA
| Hypothalamic disease | Tumor, infiltrative disease, pseudotumor cerebri, cranial radiation |
| Pituitary disease | Prolactinoma, acromegaly, Cushing’s disease, glycoprotein-producing tumor, other tumors, pituitary stalk section, empty sella, infiltrative disease |
| Medications | Antipsychotics, dopamine receptor blockers, antidepressants, antihypertensives, estrogens, opiates, cimetidine |
| Others | Primary hypothyroidism, chronic renal failure, cirrhosis, neurogenic and idiopathic causes |
| Source: Adapted and reprinted from Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders, 1995:394-405. Copyright 1995, with permission from Elsevier Science. | |
Functions of the pituitary lactotrophs regulated by estrogen include prolactin gene expression, release, storage, and cellular expression.2 Estradiol inhibition of dopamine synthesis in the tuberoinfundibular dopaminergic neurons may contribute to some gender differences in neurocognitive function and to psychiatric conditions’ clinical features.
Hyperprolactinemia and bone density. Besides causing galactorrhea and sexual dysfunction, hyperprolactinemia may has been found to be reduced in young women with amenorrhea secondary to hyperprolactinemia. This trabecular osteopenia is reversible—spinal bone density decreases progressively without treatment and improves when hyperprolactinemia is treated. Menstrual function appears to best predict risk of progressive spinal osteopenia in women with hyperprolactinemia. Estradiol level is a stronger predictor of clinical course than is the prolactin level.10
Antipsychotic drugs and hyperprolactinemia
Among the four principal dopamine pathways in the brain, the tuberoinfundibular pathway is a system of short axons at the base of the hypothalamus that releases dopamine into the portal veins of the pituitary gland. Terminals in the median eminence of the hypothalamus release dopamine that travels down the pituitary stalk in the portal veins.
Typical antipsychotics block dopamine receptors both in the striatum and in the hypothalamus.11 This finding suggests that the older drugs lack specificity of dopamine blockade. Prolactin elevations in patients treated with older antipsychotics may be associated with sexual dysfunction—a common cause of drug noncompliance, particularly in men.12
Antipsychotics and sexual side effects. Patients taking antipsy-chotics often complain—spontaneously or after focused questioning—of sexual side effects caused by drug-induced hyperprolactinemia. Assessing antipsychotic-induced sexual dysfunction may be confounded by the psychoses being treated, patient compliance, and sexuality’s complexities. Antipsychotics are generally believed to reduce desire, cause orgasmic dysfunction, and lead to difficulties during sexual performance.8
Atypical antipsychotics
A recent study designed to assess the effect of three atypical antipsychotics on serum prolactin levels enrolled 18 men with schizophrenia (mean age 32) taking clozapine, 300 to 400 mg/d; risperidone, 1 to 3 mg/d; or olanzapine, 10 to 20 mg/d, for at least 8 weeks.13 The study participants were instructed not to take their antipsychotics the night before the study. Baseline prolactin levels were measured in the morning, the men took the full daily dose of their medications, and prolactin levels were measured every 60 minutes over the next 8 hours and again at 24 hours.
Mean baseline prolactin values of clozapine (9 ng/ml, SD=5) and olanzapine (9 ng/ml, SD=5) were in the normal range (<20 ng/ml), compared with those of risperidone (27 ng/ml, SD=14). Three of the six patients taking risperidone had hyperprolactinemia at baseline. Prolactin values doubled within 6 hours of administration of all three medications. There was no comparable increase in prolactin levels in five control subjects not taking antipsychotics.
The authors concluded that these atypical antipsychotics raise prolactin levels but more transiently than typical antipsychotics. They suggested that the differences among the three drugs may be attributed to each drug’s binding properties to pituitary dopamine D2 receptors. A similar study in four patients with first-episode schizophrenia found serum prolactin levels increased from <10 ng/ml at baseline to peak levels of 80 to 120 ng/ml within 60 to 90 minutes after patients took a full daily dose of quetiapine, 700 to 800 mg/d.14
Risperidone. A study sponsored by Janssen Pharmaceutica15 reviewed the manufacturer’s experience with prolactin and its potential to induce side effects, using data from premarketing studies comparing risperidone with haloperidol. Amenorrhea and galactorrhea were assessed in women; ejaculatory dysfunction, erectile dysfunction, and gynecomastia were assessed in men.
Table 3
HYPERPROLACTINEMIA-RELATED SIDE EFFECTS REPORTED BY PATIENTS TAKING RISPERIDONE AND OLANZAPINE
| Gender and complaint | Taking risperidone (%) | Taking olanzapine (%) | Difference (P-value) |
|---|---|---|---|
| Women | |||
| Galactorrhea | 11 of 47 (23.4%) | 11 of 49 (22.4%) | 1.00 |
| Amenorrhea | 11 of 46 (23.9%) | 9 of 45 (20.0%) | 0.80 |
| Men | |||
| Gynecomastia | 9 of 115 (7.8%) | 4 of 115 (3.5%) | 0.25 |
| Sexual dysfunction | 36 of 115 (31.3%) | 34 of 114 (29.8%) | 0.89 |
| Source: Adapted and reprinted with permission from Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry2001;158:765-74. | |||
Both risperidone and haloperidol were associated with dose-related increases in plasma prolactin concentration in men and women. In women, neither risperidone dosage nor end-point prolactin concentrations were correlated with adverse events. In men:
- adverse events did not correlate with plasma prolactin concentrations
- the incidence of adverse events was dose-related
- the incidence of adverse events associated with risperidone, 4 to 10 mg/d, was not significantly greater than in patients taking placebo.
Another Janssen-sponsored study compared potential hyperprolactinemia-related side effects of risperidone and olanzapine but did not report prolactin concentrations. The authors found no significant differences between the drugs, based on breast features/menstrual changes in women and chest features/sexual dysfunction in men (Table 3).16
Olanzapine. A study sponsored by Eli Lilly and Co.17 assessed the effects of olanzapine on prolactin concentration in women previously treated with risperidone. The authors enrolled 20 Korean women with schizophrenia treated with risperidone (mean dosage 3.5 mg/d) and complaining of menstrual disturbances, galactorrhea, and/or sexual dysfunction. The mean serum prolactin concentration with risperidone was 132.2 ng/ml.
Over 2 weeks, patients were switched from risperidone to olanzapine (mean dosage 9.1 mg/d). After 8 weeks, the mean serum prolactin concentration was measured at 23.4 ng/ml. The authors noted improved menstrual function and reduced sexual side effects with olanzapine.
Conclusion
The package inserts of all atypical antipsychotics list hyperprolactinemia as a potential risk in patients taking these medications. The clinical significance of hyperprolactinemia associated with antipsychotic use is being explored but requires further elucidation.
Based on our understanding of the long-term course of untreated hyperprolactinemia—derived largely from patients not taking antipsychotics—it seems reasonable to ask patients taking atypical antipsychotics at least once a year about chest/breast complaints and sexual dysfunction. This recommendation would seem particularly relevant in patients taking risperidone at dosages >6 mg/d for sustained periods. In the absence of specific complaints, hyperprolactinemia associated with risperidone should be evaluated case by case, including perhaps endocrinology consultation.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
- Smith S, Wheeler MJ, Murray R, O’Keane V. The effects of antipsychotic-induced hyperprolactinemia on the hypothalamic-pituitary-gonadal axis. J Clin Psychopharmacol 2002;22(2):109-14. Available at: http://www.psychiatry.wustl.edu/Resources/LiteratureList/2002/May/Smith.PDF.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Vieweg reports that he is on the speakers bureau of Janssen Pharmaceutica, Eli Lilly and Co., Pfizer Inc., Wyeth Pharmaceuticals, Forest Pharmaceuticals, and GlaxoSmithKline.
Dr. Fernandez reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Antipsychotics have long been linked with hyperprolactinemia.1 This phenomenon was first considered a drug class effect, but the arrival of clozapine, better deliniation of dopamine receptor subtypes, and identification of the four principal CNS dopamine pathways revealed that hyperprolactinemia was not a universal consequence of antipsychotic use.
We now know that most atypical antipsychotics are less likely to induce hyperprolactinemia than older antipsychotics, but we don’t know why. The most likely explanation is that most of the newer agents block dopamine D2 minimally in the hypothalamic tuberoinfundibular pathway.2 Evidence is emerging that atypical agents elevate serum prolactin levels at least transiently—but usually less than typical antipsychotics—and this effect varies, depending on each compound’s dopamine-binding properties.
Figure 1 CHANGES IN PROLACTIN LEVELS OVER TIME
Mean serum prolactin concentrations from puberty until menopause. For nursing women, the length of the arrows depicts the increase in serum prolactin concentration associated with each episode of suckling. The Y-axis expresses serum prolactin concentration in both ng/ml and mg/l.
Source: Adapted and reprinted with permission from Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
Prolactin physiology
Prolactin—a large peptide containing 198 amino acids—was the first anterior pituitary gland hormone to be isolated in pure form.3 Despite its molecular weight of approximately 23,000, the hormone easily crosses the blood-brain barrier.4
Similar to other anterior pituitary hormones, prolactin is secreted episodically. Its secretion is inhibited by dopamine release from the hypothalamus and enhanced by different prolactin-releasing factors. Prolactin is the only anterior pituitary hormone that is produced by tuberoinfundibular neurons governed by dopamine.5 Dopamine stimulates lactotrope D2 receptors and inhibits adenylate cyclase, resulting in reduced prolactin synthesis and release.
Serum prolactin concentrations change during various life stages (Figure 1).6 Estrogen’s effects on prolactin gene expression regulate prolactin synthesis, resulting in higher prolactin levels in premenopausal women than in men.
Prolactin secretion
Normally, prolactin is secreted in pulses—approximately 14 in a 24-hour period, with an interpulse interval of about 80 minutes.5 A bimodal daily pattern of secretion is superimposed upon this pattern, with peak levels at night and trough levels at noon. Stress—including surgery and general anesthesia, exercise, and hypoglycemia—may transiently increase prolactin levels.
Endocrine regulation. Estrogen modulates the response of hypothalamic factors that control prolactin production. It stimulates decreased prolactin response to dopamine and increased response to thyrotropic-releasing hormone.
Insulin also stimulates prolactin secretion—probably by inducing hypoglycemia. Serum insulin level changes within physiologic ranges appear to affect prolactin regulation.
Neuroendocrine regulation. The hypothalamus blunts prolactin secretion primarily via dopamine release. This modulation occurs principally within the tuberoinfundibular dopamine pathway. The D2 subtype is the only dopamine receptor in the anterior pituitary gland:
- a decrease in dopamine levels reaching the anterior pituitary gland increases the number of D2 receptors
- to a lesser extent, estrogen decreases the number of D2 receptors.
Dopamine-modulated reductions in action potential discharge from lactotrophs and in calcium flux leads to decreased intracellular calcium and decreased prolactin secretion.5
Most hormones are target-organ agents and are regulated via a feedback loop that includes the peripheral circulation. Prolactin, however, is not considered to have a specific target organ. It is its own inhibiting factor, using an autoregulatory, pituitary-to-hypothalamus short-loop feedback circuit.
For example, prolactin-secreting tumors or drugs that elevate hormone levels lead to an increase in dopamine. In contrast, hypophysectomy decreases dopamine. In this setting, prolactin injections will restore normal dopamine levels. Prolactin-releasing factors include thyrotropic-releasing hormone, vasoactive intestinal peptide, and serotonin.
Prolactin’s actions
Many tissues—including breast, liver, ovary, testis, and prostate—have prolactin receptors. These receptors are stimulated with equal potency by prolactin and growth hormone.
The principal site of prolactin action is the mammary gland, where the hormone initiates and maintains lactation after childbirth. Major stimuli for breast development are estrogen, progesterone, prolactin, and placental mammotropic hormones. Other stimuli include insulin, cortisol, and thyroid hormone.7
Gonadotropin secretion is influenced by prolactin via the hypothalamus. Prolactin-mediated inhibition of luteinizing hormone-releasing hormone secretion impairs gonadotropin release and inhibits gonadal function.
Table 1
COMMON CLINICAL EFFECTS IN PATIENTS WITH HYPERPROLACTINEMIA
| Organ or syndrome | Clinical effects |
|---|---|
| Behavior | Direct effects Secondary effects due to hypogonadism Possible cognitive impairment |
| Bones | Decreased bone mineral density due to testosterone or estrogen deficits |
| Breast | Engorgement Lactation unrelated to breast feeding |
| Cardiovascular system | Possible adverse effects due to low levels of testosterone or estrogen |
| Menstrual function | Absence of ovulation Amenorrhea |
| Sexual function | Reduced libido Reduced arousal Orgasmic dysfunction |
| Source: Adapted and reprinted with permission from Dickson RA, Glazer WM. Neurolepticinduced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86. | |
Diagnosis of hyperprolactinemia
Pathologic hyperprolactinemia is defined as consistently elevated serum prolactin concentration (>20 ng/ml) in the absence of pregnancy or postpartum lactation. Because of the pulsatile nature of prolactin secretion, a definitive diagnosis of hyperprolactinemia requires three serum prolactin levels taken on different mornings.
Clinical presentation. Hyperprolactinemia—the most common hypothalamic-pituitary disturbance—usually presents with clinical features of gonadal dysfunction (Table 1).8 Symptoms and signs related to a brain mass—headache, visual field disturbances, ophthalmoplegia, and reduced visual acuity—may predominate with a large pituitary tumor. The patient may first present to a primary care physician or to a clinical specialist, such as a gynecologist, neurologist, ophthalmologist, pediatrician, psychiatrist, or urologist.
Thirty to 80% of women with hyperprolactinemia develop galactorrhea,9 although some women with galactorrhea have normal prolactin levels. Men with hyperprolactinemia usually have gonadal dysfunction, which unfortunately is often attributed to “psychogenic” causes. Particularly in men, prolactin is implicated in the control of libido.
Causes. Hyperprolactinemia may be caused by any process that inhibits dopamine synthesis, the neurotransmitter’s transport to the anterior pituitary gland, or its action at the lactotrope dopamine receptors ( Table 2).9 In this article, we will limit our discussion to antipsychotic drugs. have long-term effects on bone density. Trabecular bone mass
Estrogen and prolactin. During pregnancy, the rise in estrogen levels probably stimulates an increase in prolactin. Increased prolactin levels are also found in women taking estrogen-containing oral contraceptives, although this effect is very small with low-estrogen formulations.
Table 2
CAUSES OF PATHOLOGIC HYPERPROLACTINEMIA
| Hypothalamic disease | Tumor, infiltrative disease, pseudotumor cerebri, cranial radiation |
| Pituitary disease | Prolactinoma, acromegaly, Cushing’s disease, glycoprotein-producing tumor, other tumors, pituitary stalk section, empty sella, infiltrative disease |
| Medications | Antipsychotics, dopamine receptor blockers, antidepressants, antihypertensives, estrogens, opiates, cimetidine |
| Others | Primary hypothyroidism, chronic renal failure, cirrhosis, neurogenic and idiopathic causes |
| Source: Adapted and reprinted from Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders, 1995:394-405. Copyright 1995, with permission from Elsevier Science. | |
Functions of the pituitary lactotrophs regulated by estrogen include prolactin gene expression, release, storage, and cellular expression.2 Estradiol inhibition of dopamine synthesis in the tuberoinfundibular dopaminergic neurons may contribute to some gender differences in neurocognitive function and to psychiatric conditions’ clinical features.
Hyperprolactinemia and bone density. Besides causing galactorrhea and sexual dysfunction, hyperprolactinemia may has been found to be reduced in young women with amenorrhea secondary to hyperprolactinemia. This trabecular osteopenia is reversible—spinal bone density decreases progressively without treatment and improves when hyperprolactinemia is treated. Menstrual function appears to best predict risk of progressive spinal osteopenia in women with hyperprolactinemia. Estradiol level is a stronger predictor of clinical course than is the prolactin level.10
Antipsychotic drugs and hyperprolactinemia
Among the four principal dopamine pathways in the brain, the tuberoinfundibular pathway is a system of short axons at the base of the hypothalamus that releases dopamine into the portal veins of the pituitary gland. Terminals in the median eminence of the hypothalamus release dopamine that travels down the pituitary stalk in the portal veins.
Typical antipsychotics block dopamine receptors both in the striatum and in the hypothalamus.11 This finding suggests that the older drugs lack specificity of dopamine blockade. Prolactin elevations in patients treated with older antipsychotics may be associated with sexual dysfunction—a common cause of drug noncompliance, particularly in men.12
Antipsychotics and sexual side effects. Patients taking antipsy-chotics often complain—spontaneously or after focused questioning—of sexual side effects caused by drug-induced hyperprolactinemia. Assessing antipsychotic-induced sexual dysfunction may be confounded by the psychoses being treated, patient compliance, and sexuality’s complexities. Antipsychotics are generally believed to reduce desire, cause orgasmic dysfunction, and lead to difficulties during sexual performance.8
Atypical antipsychotics
A recent study designed to assess the effect of three atypical antipsychotics on serum prolactin levels enrolled 18 men with schizophrenia (mean age 32) taking clozapine, 300 to 400 mg/d; risperidone, 1 to 3 mg/d; or olanzapine, 10 to 20 mg/d, for at least 8 weeks.13 The study participants were instructed not to take their antipsychotics the night before the study. Baseline prolactin levels were measured in the morning, the men took the full daily dose of their medications, and prolactin levels were measured every 60 minutes over the next 8 hours and again at 24 hours.
Mean baseline prolactin values of clozapine (9 ng/ml, SD=5) and olanzapine (9 ng/ml, SD=5) were in the normal range (<20 ng/ml), compared with those of risperidone (27 ng/ml, SD=14). Three of the six patients taking risperidone had hyperprolactinemia at baseline. Prolactin values doubled within 6 hours of administration of all three medications. There was no comparable increase in prolactin levels in five control subjects not taking antipsychotics.
The authors concluded that these atypical antipsychotics raise prolactin levels but more transiently than typical antipsychotics. They suggested that the differences among the three drugs may be attributed to each drug’s binding properties to pituitary dopamine D2 receptors. A similar study in four patients with first-episode schizophrenia found serum prolactin levels increased from <10 ng/ml at baseline to peak levels of 80 to 120 ng/ml within 60 to 90 minutes after patients took a full daily dose of quetiapine, 700 to 800 mg/d.14
Risperidone. A study sponsored by Janssen Pharmaceutica15 reviewed the manufacturer’s experience with prolactin and its potential to induce side effects, using data from premarketing studies comparing risperidone with haloperidol. Amenorrhea and galactorrhea were assessed in women; ejaculatory dysfunction, erectile dysfunction, and gynecomastia were assessed in men.
Table 3
HYPERPROLACTINEMIA-RELATED SIDE EFFECTS REPORTED BY PATIENTS TAKING RISPERIDONE AND OLANZAPINE
| Gender and complaint | Taking risperidone (%) | Taking olanzapine (%) | Difference (P-value) |
|---|---|---|---|
| Women | |||
| Galactorrhea | 11 of 47 (23.4%) | 11 of 49 (22.4%) | 1.00 |
| Amenorrhea | 11 of 46 (23.9%) | 9 of 45 (20.0%) | 0.80 |
| Men | |||
| Gynecomastia | 9 of 115 (7.8%) | 4 of 115 (3.5%) | 0.25 |
| Sexual dysfunction | 36 of 115 (31.3%) | 34 of 114 (29.8%) | 0.89 |
| Source: Adapted and reprinted with permission from Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry2001;158:765-74. | |||
Both risperidone and haloperidol were associated with dose-related increases in plasma prolactin concentration in men and women. In women, neither risperidone dosage nor end-point prolactin concentrations were correlated with adverse events. In men:
- adverse events did not correlate with plasma prolactin concentrations
- the incidence of adverse events was dose-related
- the incidence of adverse events associated with risperidone, 4 to 10 mg/d, was not significantly greater than in patients taking placebo.
Another Janssen-sponsored study compared potential hyperprolactinemia-related side effects of risperidone and olanzapine but did not report prolactin concentrations. The authors found no significant differences between the drugs, based on breast features/menstrual changes in women and chest features/sexual dysfunction in men (Table 3).16
Olanzapine. A study sponsored by Eli Lilly and Co.17 assessed the effects of olanzapine on prolactin concentration in women previously treated with risperidone. The authors enrolled 20 Korean women with schizophrenia treated with risperidone (mean dosage 3.5 mg/d) and complaining of menstrual disturbances, galactorrhea, and/or sexual dysfunction. The mean serum prolactin concentration with risperidone was 132.2 ng/ml.
Over 2 weeks, patients were switched from risperidone to olanzapine (mean dosage 9.1 mg/d). After 8 weeks, the mean serum prolactin concentration was measured at 23.4 ng/ml. The authors noted improved menstrual function and reduced sexual side effects with olanzapine.
Conclusion
The package inserts of all atypical antipsychotics list hyperprolactinemia as a potential risk in patients taking these medications. The clinical significance of hyperprolactinemia associated with antipsychotic use is being explored but requires further elucidation.
Based on our understanding of the long-term course of untreated hyperprolactinemia—derived largely from patients not taking antipsychotics—it seems reasonable to ask patients taking atypical antipsychotics at least once a year about chest/breast complaints and sexual dysfunction. This recommendation would seem particularly relevant in patients taking risperidone at dosages >6 mg/d for sustained periods. In the absence of specific complaints, hyperprolactinemia associated with risperidone should be evaluated case by case, including perhaps endocrinology consultation.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
- Smith S, Wheeler MJ, Murray R, O’Keane V. The effects of antipsychotic-induced hyperprolactinemia on the hypothalamic-pituitary-gonadal axis. J Clin Psychopharmacol 2002;22(2):109-14. Available at: http://www.psychiatry.wustl.edu/Resources/LiteratureList/2002/May/Smith.PDF.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Vieweg reports that he is on the speakers bureau of Janssen Pharmaceutica, Eli Lilly and Co., Pfizer Inc., Wyeth Pharmaceuticals, Forest Pharmaceuticals, and GlaxoSmithKline.
Dr. Fernandez reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Clemens JA, Smalstig EB, Sawyer BD. Antipsychotic drugs stimulate prolactin release. Psychopharmacol. 1974;40:123-7.
2. Petty RG. Prolactin and antipsychotic medications: mechanism of action. Schizophr Res 1999;35(suppl):S67-S73.
3. West ES, Todd WR. The hormones. In: West ES, Todd WR (eds). Textbook of biochemistry. New York: The Macmillan Co., 1961;1315-54.
4. Belchetz PE, Ridley RM, Baker HF. Studies on the accessibility of prolactin and growth hormone to brain: effect of opiate agonists on hormone levels in serial, simultaneous plasma and cerebrospinal fluid samples in the rhesus monkey. Brain Res 1982;239:310-4.
5. Cooke NE. Prolactin: basic physiology. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Company, 1995;368-93.
6. Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
7. Thorner MO, Vance ML, Laws ER, Horvath E, Kovacs K. The anterior pituitary. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR (eds). Williams textbook of endocrinology. Philadelphia: W.B. Saunders Co., 1998;249-340.
8. Dickson RA, Glazer WM. Neuroleptic-induced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86.
9. Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Co., 1995;394-405.
10. Biller BM, Baum HB, Rosenthal DI, Saxe VC, Charpie PM, Kilibanski A. Progressive trabecular osteopenia in women with hyperprolactinemic amenorrhea. J Clin Endocrinol Metab 1992;75:692-7.
11. Baron JC, Martinot JL, Cambon H, et al. Striatal dopamine receptor occupancy during and following withdrawal from neuroleptic treatment: correlative evaluation by positron emission tomography and plasma prolactin levels. Psychopharmacol 1989;99:463-72.
12. Ghadirian AM, Chouinard G, Annable L. Sexual dysfunction and plasma prolactin levels in neuroleptic-treated schizophrenic outpatients. J Nerv Ment Dis 1982;170:463-7.
13. Turrone P, Kapur S, Seeman MV, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry 2002;159:133-5.
14. Alexiadis M, Whitehorn D, Woodley H, Kopala L. Prolactin elevation with quetiapine (letter). Am J Psychiatry 2002;159(Sept):1608-9.
15. Kleinberg DL, Davis JM, De Coster R, Van Baelen B, Brecher M. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
16. Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 2001;158:765-74.
17. Kim K, Pae C, Chae J, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63:408-13.
1. Clemens JA, Smalstig EB, Sawyer BD. Antipsychotic drugs stimulate prolactin release. Psychopharmacol. 1974;40:123-7.
2. Petty RG. Prolactin and antipsychotic medications: mechanism of action. Schizophr Res 1999;35(suppl):S67-S73.
3. West ES, Todd WR. The hormones. In: West ES, Todd WR (eds). Textbook of biochemistry. New York: The Macmillan Co., 1961;1315-54.
4. Belchetz PE, Ridley RM, Baker HF. Studies on the accessibility of prolactin and growth hormone to brain: effect of opiate agonists on hormone levels in serial, simultaneous plasma and cerebrospinal fluid samples in the rhesus monkey. Brain Res 1982;239:310-4.
5. Cooke NE. Prolactin: basic physiology. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Company, 1995;368-93.
6. Friesen HG. Human prolactin. Ann R Coll Phys Surg Can 1978;11:275-81.
7. Thorner MO, Vance ML, Laws ER, Horvath E, Kovacs K. The anterior pituitary. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR (eds). Williams textbook of endocrinology. Philadelphia: W.B. Saunders Co., 1998;249-340.
8. Dickson RA, Glazer WM. Neuroleptic-induced hyperprolactinemia. Schizophr Res 1999;35(suppl):S75-S86.
9. Vance ML, Thorner MO. Prolactin: hyperprolactinemic syndromes and management. In: DeGroot LJ, Besser M, Burger HG, et al (eds). Endocrinology. Philadelphia: W.B. Saunders Co., 1995;394-405.
10. Biller BM, Baum HB, Rosenthal DI, Saxe VC, Charpie PM, Kilibanski A. Progressive trabecular osteopenia in women with hyperprolactinemic amenorrhea. J Clin Endocrinol Metab 1992;75:692-7.
11. Baron JC, Martinot JL, Cambon H, et al. Striatal dopamine receptor occupancy during and following withdrawal from neuroleptic treatment: correlative evaluation by positron emission tomography and plasma prolactin levels. Psychopharmacol 1989;99:463-72.
12. Ghadirian AM, Chouinard G, Annable L. Sexual dysfunction and plasma prolactin levels in neuroleptic-treated schizophrenic outpatients. J Nerv Ment Dis 1982;170:463-7.
13. Turrone P, Kapur S, Seeman MV, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry 2002;159:133-5.
14. Alexiadis M, Whitehorn D, Woodley H, Kopala L. Prolactin elevation with quetiapine (letter). Am J Psychiatry 2002;159(Sept):1608-9.
15. Kleinberg DL, Davis JM, De Coster R, Van Baelen B, Brecher M. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
16. Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 2001;158:765-74.
17. Kim K, Pae C, Chae J, et al. Effects of olanzapine on prolactin levels of female patients with schizophrenia treated with risperidone. J Clin Psychiatry 2002;63:408-13.