User login
External fixators are commonly used as a temporizing treatment for periarticular fractures about the knee. Since its inception with a claw used for patellar fractures by Malgaigne in 1853,1 external fixation has evolved to include pin–crossbar constructs. The stiffness of the construct directly affects the rate at which the frames are likely to fail.2 Most external fixation systems have the option for 2 types of pin–bar connectors, pin-to-bar clamps or multipin clamps. The multipin clamps rely on a cluster of multiple pins to connect the longitudinal supports. These clamps use the “bull horn” extensions to connect the pins to bars (Figure 1). The implant manufacturers recommend the use of 2 longitudinal bars when using these clamps. Conversely, single pin-to-bar clamps permit widely spaced pins but multipin clamps do not. Pin-to-bar clamps also tend to allow the longitudinal cross-bars to be placed closer to bone, improving frame stability.1
In the experience of Dr. Reisman, utilization of pin-to-bar clamps has resulted in improved external fixator construct stiffness compared with those using multipin clamps. He has recognized that, in his own practice, a busy level I trauma center where 4 to 5 spanning knee frames are applied daily, fracture stability is improved with the use of pin-to-bar clamps and often with only a single crossbar, resulting in a simpler, low-cost construct. Despite external fixators used for temporary fixation, frames need to be strong enough to maintain fracture length and stabilize the soft-tissue envelope for days to weeks. It is critical that the frame’s stability allows for patient transfers but controls fracture motion until definitive fixation. Despite having both options available in the external fixator set, there are no biomechanical studies that compare the effect of using pin-to-bar clamps or multipin clamps and bull horns on external fixator stiffness.
In this study, we compared the stiffness of 3 different types of spanning knee external fixator configurations, using multi-pin clamps and 2 crossbars, or pin-to-bar clamps with 1 or 2 crossbars. We compared constructs using 2 systems, 1 with 8-mm–diameter and another with 11-mm–diameter crossbars. We hypothesized that constructs assembled with pin-to-bar clamps would have improved bending stiffness compared with constructs using multipin clamps.
Materials and Methods
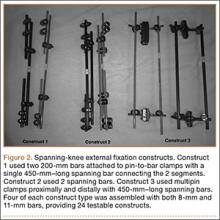
Three constructs were made under the supervision of Dr. Reisman, a trauma fellowship–trained orthopedic surgeon. The first construct (construct 1) used two 200-mm bars attached to pin-to-bar clamps with a single 450-mm–long spanning bar connecting the 2 segments (Figure 2). The second construct (construct 2) used 2 spanning bars with pin-to-bar clamps. The third construct (construct 3) used multipin clamps proximally and distally with two 450-mm–long spanning bars. Therefore, we tested 2 types of constructs using pin-to-bar clamps and 1 construct with multipin clamps. Four of each construct type were assembled with both 8-mm (Stryker) and 11-mm bars (Synthes), providing 24 testable constructs. For this study, we tested previously used and cleaned external fixation pins, bars, and clamps obtained from our trauma center. All equipment was examined thoroughly for any potential damaged parts.
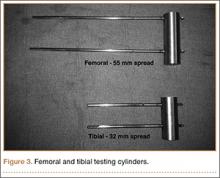
To simulate the femoral and tibial attachments, two 5-mm–diameter pins were drilled into each of 2 steel cylinders and welded in place. The femoral cylinder (8.3×2.5 cm) had a pin distance of 55 mm, and the tibial cylinder (6.4×2.5 cm) had a pin distance of 32 mm (Figure 3). The pins were welded intosteel cylinders to help prevent any loosening or failure at the pin (ie, metal interface isolating stress to the components). Dr. Desai assembled the constructs and placed them on the cylinders with a distance of 25 mm between the fixator construct and the cylinder, with 306 mm between the femoral and tibial cylinders. The pin diameters, pin spread, pin number, and bar-to-cylinder distance were constant throughout testing with these specifications.
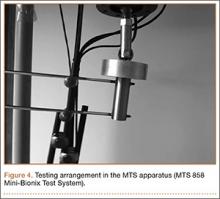
The assembled constructs were tested on a materials testing machine (MTS 858 Mini-Bionix Test System). A compressive force was applied, through a roller, to a flat plate (Figures 4, 5). This allowed the constructs to flex and bend freely without overly stressing the simulated pin-to-bone interface. Using this loading method, we could compare the stiffness of the different assembled constructs. Each assembled construct was tested 4 times sequentially on the MTS machine. There was no pin deformation when the load was applied through the roller to the flat plate, to the cylinder, to the pins, and onto the construct. It was possible to observe that the construct flexed when the load was applied. Load-displacement curves were produced for each test, and the stiffness was calculated from the slope of this curve. Each test was repeated 4 times, and the stiffness was measured from the load-displacement curve each time. The 4 stiffness measurements were averaged for each construct and compared across all constructs, using a Wilcoxon rank sum test for statistical analysis.
Results
Construct Design
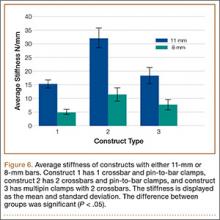
Three different construct designs were evaluated using our testing protocol. The mean stiffness differed across all constructs as seen in Figure 6. Of the constructs using the 11-mm–diameter bars, construct 2 had the highest mean stiffness (32.1 +/- 3.7 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (15.3 +/- 1.5 N/mm; P < .05) and construct 3 (18.4 +/- 2.9 N/mm; P< .05). There was no statistically significant difference in stiffness between construct 1 and construct 3.
Of the constructs using 8-mm–diameter bars, construct 2 had the highest mean stiffness (11.5 +/- 2.4 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (5.0 +/- 0.9 N/mm; P < .05). There was no statistically significant difference in stiffness between construct 2 and construct 3 (7.8 +/- 1.9 N/mm) or between construct 1 and construct 3.
Discussion
Although numerous investigators have examined the biomechanical properties of external fixator systems, the effect of pin-to-bar clamps on frame stiffness is unknown. Biomechanical studies have found that uniplanar constructs with multiple bars can provide adequate strength for temporary fixation.3-9 With multiple options within a particular external fixator set, it is ideal to understand the benefit of using one component instead of another.
The main results from this experiment are: (1) constructs with pin-to-bar clamps and 2 crossbars are stiffer than those using multipin clamps and 2 crossbars; (2) constructs with a single crossbar and pin-to-bar clamps are as stiff as constructs using 2 crossbars and multipin clamps.
Figure 6 shows the average stiffness differences between the 8-mm and 11-mm–diameter bar constructs tested in this study. As expected, each 11-mm diameter–bar construct had a higher average stiffness compared with the 8-mm–diameter bar constructs. Across both the 8-mm and 11-mm–diameter bar constructs, construct 2 had a higher stiffness than that of constructs 1 and 3. Furthermore, there was no difference in the stiffness between constructs 1 and 3.
To improve external fixator stiffness, number of pins and optimization of pin spread can improve the strength of the construct.7 When using pin-to-bar clamps, 1 pin should be as close to the fracture as possible, with the second pin as far from the fracture as possible. 7 Multipin clamps, by design, prevent any optimization of pin spread and require a clustered-pin arrangement.
Bar configuration also plays a critical role in construct stiffness. Bar-to-bone distance should be approximately 2 fingerbreadths from the skin to maximize the stiffness of the construct.4,10-14 Multipin clamps use “bull horn” extensions that tend to elevate the bar away from the skin, increasing the distance between the bar and the bone.
A temporary spanning knee external fixator is commonly used for treating high-energy periarticular tibial or femoral fractures. To hold the fracture in an adequately reduced position, the frame must resist the deforming forces inherent with all fractures. A frame that is not adequately stiff will not hold the fracture in the reduced position, even at the time of initial surgery, which negates one of the benefits of placing the patient in the frame. Hence, adequate stiffness of the spanning-knee fixator is critical to the effectiveness of temporary stabilization before permanent fixation.
The results of this study provide evidence for the superiority of pin-to-bar clamps over multipin clamps in optimizing external fixator construct stiffness. At our institution, we almost exclusively use the single pin-to-bar clamps for spanning-knee external fixation. Based on the results of this study, we often use only a single crossbar. The ability to use a single bar greatly reduces the cost of the construct because crossbars can cost from $100 to $150, depending on the manufacturer.
A recent cost analysis of spanning-knee external fixators showed that construct costs can range from $8,000 to $19,000.15 The lower-cost constructs included 2 crossbars while the more expensive constructs had additional bars and multipin clamps. The authors noted that constructs with larger diameter bars and higher overall stiffness resulted in an improved cost per stiffness ratio. The results of this study support our conclusions regarding bar diameter. Additionally, our results show improved stiffness of constructs with pin-to-bar clamps instead of multipin clamps. By limiting the need for an additional bar, using pin-to-bar clamps and a single large diameter crossbar can create a very cost-efficient and rigidly stable construct.
One criticism of this study is the testing of used equipment. All external fixator manufacturers must evaluate and carefully examine any used equipment prior to the resterilization process and potential release to the practitioner for re-use. Our rationale for using used equipment is based on the assumption that the vast majority of patients do not have their external fixators removed because of failure but because of definitive surgical treatment, and the timing of removal does not necessarily follow a predetermined protocol. For example, timing of definitive surgery is usually set by the patient’s general health status, status of the soft tissues, and surgeon availability. Therefore, this equipment was tested with the presumption that the equipment was in the same state as if the patient continued to wear the frame 1 more day. A study testing unused equipment would be the next step in evaluating external fixators.
Another potential criticism of this study is the use of the same pin spread for constructs using pin-to-bar clamps and those using multipin clamps. We established that, to minimize confounding variables, a constant pin spread was necessary. This also mirrors our more common pin configurations for external fixators with pins placed outside the zone of injury. However, a key determinant of external fixator stability is pin spread, and this is a potential benefit to using pin-to-bar clamps over the multipin clamps that require an exact pin spread. Indeed, our results may have shown a larger difference between constructs using the pin-to-bar clamps compared with the multipin clamps had we maximized the pin spread. Future studies may be able to use a fracture model to compare the pin-to-bar clamps and multipin clamps using pin spread to maximize stability.
Conclusion
This study has shown that using pin-to-bar clamps can create strong, stable constructs for temporary external fixation. In particular, constructs made with a single bar and pin-to-bar clamps can produce easily implantable and less expensive constructs that are stiff enough to withstand deformation and allow patient transfers without excessive displacement of the fracture.
1. Behrens F. A primer of fixator devices and configurations. Clin Orthop Relat Res. 1989;241:5-14.
2. Chao EY, Aro HT, Lewallen DG, Kelly PJ. The effect of rigidity on fracture healing in external fixation. Clin Orthop Relat Res. 1989;241:24-35.
3. Schrøder HA, Weeth RE, Madsen T. Experimental analysis of Hoffman external fixation in various mountings. Arch Orthop Trauma Surg. 1985;104(4):197-200.
4. Kempson GE, Campbell D. The comparative stiffness of external fixation frames. Injury. 1981;12(4):297-304.
5. Giotakis N, Narayan B. Stability with unilateral external fixation in the tibia. Strategies Trauma Limb Reconstr. 2007;2(1):13-20.
6. Briggs BT, Chao EY. The mechanical performance of the standard Hoffmann-Vidal external fixation apparatus. J Bone Joint Surg Am. 1982;64(4):566-573.
7. Hipp JA, Edgerton BC, An KN, Hayes WC. Structural consequences of transcortical holes in long bones loaded in torsion. J Biomech. 1990;23(12):1261-1268.
8. Edgerton BC, An KN, Morrey BF. Torsional strength reduction due to cortical defects in bone. J Orthop Res. 1990;8(6):851-855.
9. Huiskes R, Chao E. Guidelines for external fixation frame rigidity and stresses. J Orthop Res. 1986;4(1):68-75.
10. Pettine KA, Chao EY, Kelly PJ. Analysis of the external fixator pin-bone interface. Clin Orthop Relat Res. 1993;(293):18-27.
11. Halsey D, Fleming B, Pope MH, Krag M, Kristiansen T. External fixator pin design. Clin Orthop Relat Res. 1992;(278):305-312.
12. Huiskes R, Chao EY, Crippen TE. Parametric analyses of pin-bone stresses in external fracture fixation devices. J Orthop Res. 1985;3(3):341-349.
13. Behrens F, Johnson W. Unilateral external fixation methods to increase and reduce frame stiffness. Clin Orthop Relat Res.1989;(241):48-56.
14. Mercer D, Firoozbakhsh K, Prevost M, Mulkey P, DeCoster TA, Schenck R. Stiffness of knee spanning external fixation systems for traumatic knee dislocations: a biomechanical study. J Orthop Trauma. 2010;24(11):693-696.
15. Kim H, Russell JP, Hsieh AH, O’Toole RV. Bar diameter is an important component of knee-spanning external fixator stiffness and cost. Orthopedics. 2014;37(7):e671-e677.
External fixators are commonly used as a temporizing treatment for periarticular fractures about the knee. Since its inception with a claw used for patellar fractures by Malgaigne in 1853,1 external fixation has evolved to include pin–crossbar constructs. The stiffness of the construct directly affects the rate at which the frames are likely to fail.2 Most external fixation systems have the option for 2 types of pin–bar connectors, pin-to-bar clamps or multipin clamps. The multipin clamps rely on a cluster of multiple pins to connect the longitudinal supports. These clamps use the “bull horn” extensions to connect the pins to bars (Figure 1). The implant manufacturers recommend the use of 2 longitudinal bars when using these clamps. Conversely, single pin-to-bar clamps permit widely spaced pins but multipin clamps do not. Pin-to-bar clamps also tend to allow the longitudinal cross-bars to be placed closer to bone, improving frame stability.1
In the experience of Dr. Reisman, utilization of pin-to-bar clamps has resulted in improved external fixator construct stiffness compared with those using multipin clamps. He has recognized that, in his own practice, a busy level I trauma center where 4 to 5 spanning knee frames are applied daily, fracture stability is improved with the use of pin-to-bar clamps and often with only a single crossbar, resulting in a simpler, low-cost construct. Despite external fixators used for temporary fixation, frames need to be strong enough to maintain fracture length and stabilize the soft-tissue envelope for days to weeks. It is critical that the frame’s stability allows for patient transfers but controls fracture motion until definitive fixation. Despite having both options available in the external fixator set, there are no biomechanical studies that compare the effect of using pin-to-bar clamps or multipin clamps and bull horns on external fixator stiffness.
In this study, we compared the stiffness of 3 different types of spanning knee external fixator configurations, using multi-pin clamps and 2 crossbars, or pin-to-bar clamps with 1 or 2 crossbars. We compared constructs using 2 systems, 1 with 8-mm–diameter and another with 11-mm–diameter crossbars. We hypothesized that constructs assembled with pin-to-bar clamps would have improved bending stiffness compared with constructs using multipin clamps.
Materials and Methods
Three constructs were made under the supervision of Dr. Reisman, a trauma fellowship–trained orthopedic surgeon. The first construct (construct 1) used two 200-mm bars attached to pin-to-bar clamps with a single 450-mm–long spanning bar connecting the 2 segments (Figure 2). The second construct (construct 2) used 2 spanning bars with pin-to-bar clamps. The third construct (construct 3) used multipin clamps proximally and distally with two 450-mm–long spanning bars. Therefore, we tested 2 types of constructs using pin-to-bar clamps and 1 construct with multipin clamps. Four of each construct type were assembled with both 8-mm (Stryker) and 11-mm bars (Synthes), providing 24 testable constructs. For this study, we tested previously used and cleaned external fixation pins, bars, and clamps obtained from our trauma center. All equipment was examined thoroughly for any potential damaged parts.
To simulate the femoral and tibial attachments, two 5-mm–diameter pins were drilled into each of 2 steel cylinders and welded in place. The femoral cylinder (8.3×2.5 cm) had a pin distance of 55 mm, and the tibial cylinder (6.4×2.5 cm) had a pin distance of 32 mm (Figure 3). The pins were welded intosteel cylinders to help prevent any loosening or failure at the pin (ie, metal interface isolating stress to the components). Dr. Desai assembled the constructs and placed them on the cylinders with a distance of 25 mm between the fixator construct and the cylinder, with 306 mm between the femoral and tibial cylinders. The pin diameters, pin spread, pin number, and bar-to-cylinder distance were constant throughout testing with these specifications.
The assembled constructs were tested on a materials testing machine (MTS 858 Mini-Bionix Test System). A compressive force was applied, through a roller, to a flat plate (Figures 4, 5). This allowed the constructs to flex and bend freely without overly stressing the simulated pin-to-bone interface. Using this loading method, we could compare the stiffness of the different assembled constructs. Each assembled construct was tested 4 times sequentially on the MTS machine. There was no pin deformation when the load was applied through the roller to the flat plate, to the cylinder, to the pins, and onto the construct. It was possible to observe that the construct flexed when the load was applied. Load-displacement curves were produced for each test, and the stiffness was calculated from the slope of this curve. Each test was repeated 4 times, and the stiffness was measured from the load-displacement curve each time. The 4 stiffness measurements were averaged for each construct and compared across all constructs, using a Wilcoxon rank sum test for statistical analysis.
Results
Construct Design
Three different construct designs were evaluated using our testing protocol. The mean stiffness differed across all constructs as seen in Figure 6. Of the constructs using the 11-mm–diameter bars, construct 2 had the highest mean stiffness (32.1 +/- 3.7 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (15.3 +/- 1.5 N/mm; P < .05) and construct 3 (18.4 +/- 2.9 N/mm; P< .05). There was no statistically significant difference in stiffness between construct 1 and construct 3.
Of the constructs using 8-mm–diameter bars, construct 2 had the highest mean stiffness (11.5 +/- 2.4 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (5.0 +/- 0.9 N/mm; P < .05). There was no statistically significant difference in stiffness between construct 2 and construct 3 (7.8 +/- 1.9 N/mm) or between construct 1 and construct 3.
Discussion
Although numerous investigators have examined the biomechanical properties of external fixator systems, the effect of pin-to-bar clamps on frame stiffness is unknown. Biomechanical studies have found that uniplanar constructs with multiple bars can provide adequate strength for temporary fixation.3-9 With multiple options within a particular external fixator set, it is ideal to understand the benefit of using one component instead of another.
The main results from this experiment are: (1) constructs with pin-to-bar clamps and 2 crossbars are stiffer than those using multipin clamps and 2 crossbars; (2) constructs with a single crossbar and pin-to-bar clamps are as stiff as constructs using 2 crossbars and multipin clamps.
Figure 6 shows the average stiffness differences between the 8-mm and 11-mm–diameter bar constructs tested in this study. As expected, each 11-mm diameter–bar construct had a higher average stiffness compared with the 8-mm–diameter bar constructs. Across both the 8-mm and 11-mm–diameter bar constructs, construct 2 had a higher stiffness than that of constructs 1 and 3. Furthermore, there was no difference in the stiffness between constructs 1 and 3.
To improve external fixator stiffness, number of pins and optimization of pin spread can improve the strength of the construct.7 When using pin-to-bar clamps, 1 pin should be as close to the fracture as possible, with the second pin as far from the fracture as possible. 7 Multipin clamps, by design, prevent any optimization of pin spread and require a clustered-pin arrangement.
Bar configuration also plays a critical role in construct stiffness. Bar-to-bone distance should be approximately 2 fingerbreadths from the skin to maximize the stiffness of the construct.4,10-14 Multipin clamps use “bull horn” extensions that tend to elevate the bar away from the skin, increasing the distance between the bar and the bone.
A temporary spanning knee external fixator is commonly used for treating high-energy periarticular tibial or femoral fractures. To hold the fracture in an adequately reduced position, the frame must resist the deforming forces inherent with all fractures. A frame that is not adequately stiff will not hold the fracture in the reduced position, even at the time of initial surgery, which negates one of the benefits of placing the patient in the frame. Hence, adequate stiffness of the spanning-knee fixator is critical to the effectiveness of temporary stabilization before permanent fixation.
The results of this study provide evidence for the superiority of pin-to-bar clamps over multipin clamps in optimizing external fixator construct stiffness. At our institution, we almost exclusively use the single pin-to-bar clamps for spanning-knee external fixation. Based on the results of this study, we often use only a single crossbar. The ability to use a single bar greatly reduces the cost of the construct because crossbars can cost from $100 to $150, depending on the manufacturer.
A recent cost analysis of spanning-knee external fixators showed that construct costs can range from $8,000 to $19,000.15 The lower-cost constructs included 2 crossbars while the more expensive constructs had additional bars and multipin clamps. The authors noted that constructs with larger diameter bars and higher overall stiffness resulted in an improved cost per stiffness ratio. The results of this study support our conclusions regarding bar diameter. Additionally, our results show improved stiffness of constructs with pin-to-bar clamps instead of multipin clamps. By limiting the need for an additional bar, using pin-to-bar clamps and a single large diameter crossbar can create a very cost-efficient and rigidly stable construct.
One criticism of this study is the testing of used equipment. All external fixator manufacturers must evaluate and carefully examine any used equipment prior to the resterilization process and potential release to the practitioner for re-use. Our rationale for using used equipment is based on the assumption that the vast majority of patients do not have their external fixators removed because of failure but because of definitive surgical treatment, and the timing of removal does not necessarily follow a predetermined protocol. For example, timing of definitive surgery is usually set by the patient’s general health status, status of the soft tissues, and surgeon availability. Therefore, this equipment was tested with the presumption that the equipment was in the same state as if the patient continued to wear the frame 1 more day. A study testing unused equipment would be the next step in evaluating external fixators.
Another potential criticism of this study is the use of the same pin spread for constructs using pin-to-bar clamps and those using multipin clamps. We established that, to minimize confounding variables, a constant pin spread was necessary. This also mirrors our more common pin configurations for external fixators with pins placed outside the zone of injury. However, a key determinant of external fixator stability is pin spread, and this is a potential benefit to using pin-to-bar clamps over the multipin clamps that require an exact pin spread. Indeed, our results may have shown a larger difference between constructs using the pin-to-bar clamps compared with the multipin clamps had we maximized the pin spread. Future studies may be able to use a fracture model to compare the pin-to-bar clamps and multipin clamps using pin spread to maximize stability.
Conclusion
This study has shown that using pin-to-bar clamps can create strong, stable constructs for temporary external fixation. In particular, constructs made with a single bar and pin-to-bar clamps can produce easily implantable and less expensive constructs that are stiff enough to withstand deformation and allow patient transfers without excessive displacement of the fracture.
External fixators are commonly used as a temporizing treatment for periarticular fractures about the knee. Since its inception with a claw used for patellar fractures by Malgaigne in 1853,1 external fixation has evolved to include pin–crossbar constructs. The stiffness of the construct directly affects the rate at which the frames are likely to fail.2 Most external fixation systems have the option for 2 types of pin–bar connectors, pin-to-bar clamps or multipin clamps. The multipin clamps rely on a cluster of multiple pins to connect the longitudinal supports. These clamps use the “bull horn” extensions to connect the pins to bars (Figure 1). The implant manufacturers recommend the use of 2 longitudinal bars when using these clamps. Conversely, single pin-to-bar clamps permit widely spaced pins but multipin clamps do not. Pin-to-bar clamps also tend to allow the longitudinal cross-bars to be placed closer to bone, improving frame stability.1
In the experience of Dr. Reisman, utilization of pin-to-bar clamps has resulted in improved external fixator construct stiffness compared with those using multipin clamps. He has recognized that, in his own practice, a busy level I trauma center where 4 to 5 spanning knee frames are applied daily, fracture stability is improved with the use of pin-to-bar clamps and often with only a single crossbar, resulting in a simpler, low-cost construct. Despite external fixators used for temporary fixation, frames need to be strong enough to maintain fracture length and stabilize the soft-tissue envelope for days to weeks. It is critical that the frame’s stability allows for patient transfers but controls fracture motion until definitive fixation. Despite having both options available in the external fixator set, there are no biomechanical studies that compare the effect of using pin-to-bar clamps or multipin clamps and bull horns on external fixator stiffness.
In this study, we compared the stiffness of 3 different types of spanning knee external fixator configurations, using multi-pin clamps and 2 crossbars, or pin-to-bar clamps with 1 or 2 crossbars. We compared constructs using 2 systems, 1 with 8-mm–diameter and another with 11-mm–diameter crossbars. We hypothesized that constructs assembled with pin-to-bar clamps would have improved bending stiffness compared with constructs using multipin clamps.
Materials and Methods
Three constructs were made under the supervision of Dr. Reisman, a trauma fellowship–trained orthopedic surgeon. The first construct (construct 1) used two 200-mm bars attached to pin-to-bar clamps with a single 450-mm–long spanning bar connecting the 2 segments (Figure 2). The second construct (construct 2) used 2 spanning bars with pin-to-bar clamps. The third construct (construct 3) used multipin clamps proximally and distally with two 450-mm–long spanning bars. Therefore, we tested 2 types of constructs using pin-to-bar clamps and 1 construct with multipin clamps. Four of each construct type were assembled with both 8-mm (Stryker) and 11-mm bars (Synthes), providing 24 testable constructs. For this study, we tested previously used and cleaned external fixation pins, bars, and clamps obtained from our trauma center. All equipment was examined thoroughly for any potential damaged parts.
To simulate the femoral and tibial attachments, two 5-mm–diameter pins were drilled into each of 2 steel cylinders and welded in place. The femoral cylinder (8.3×2.5 cm) had a pin distance of 55 mm, and the tibial cylinder (6.4×2.5 cm) had a pin distance of 32 mm (Figure 3). The pins were welded intosteel cylinders to help prevent any loosening or failure at the pin (ie, metal interface isolating stress to the components). Dr. Desai assembled the constructs and placed them on the cylinders with a distance of 25 mm between the fixator construct and the cylinder, with 306 mm between the femoral and tibial cylinders. The pin diameters, pin spread, pin number, and bar-to-cylinder distance were constant throughout testing with these specifications.
The assembled constructs were tested on a materials testing machine (MTS 858 Mini-Bionix Test System). A compressive force was applied, through a roller, to a flat plate (Figures 4, 5). This allowed the constructs to flex and bend freely without overly stressing the simulated pin-to-bone interface. Using this loading method, we could compare the stiffness of the different assembled constructs. Each assembled construct was tested 4 times sequentially on the MTS machine. There was no pin deformation when the load was applied through the roller to the flat plate, to the cylinder, to the pins, and onto the construct. It was possible to observe that the construct flexed when the load was applied. Load-displacement curves were produced for each test, and the stiffness was calculated from the slope of this curve. Each test was repeated 4 times, and the stiffness was measured from the load-displacement curve each time. The 4 stiffness measurements were averaged for each construct and compared across all constructs, using a Wilcoxon rank sum test for statistical analysis.
Results
Construct Design
Three different construct designs were evaluated using our testing protocol. The mean stiffness differed across all constructs as seen in Figure 6. Of the constructs using the 11-mm–diameter bars, construct 2 had the highest mean stiffness (32.1 +/- 3.7 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (15.3 +/- 1.5 N/mm; P < .05) and construct 3 (18.4 +/- 2.9 N/mm; P< .05). There was no statistically significant difference in stiffness between construct 1 and construct 3.
Of the constructs using 8-mm–diameter bars, construct 2 had the highest mean stiffness (11.5 +/- 2.4 N/mm), and this stiffness was significantly greater than the mean stiffness for construct 1 (5.0 +/- 0.9 N/mm; P < .05). There was no statistically significant difference in stiffness between construct 2 and construct 3 (7.8 +/- 1.9 N/mm) or between construct 1 and construct 3.
Discussion
Although numerous investigators have examined the biomechanical properties of external fixator systems, the effect of pin-to-bar clamps on frame stiffness is unknown. Biomechanical studies have found that uniplanar constructs with multiple bars can provide adequate strength for temporary fixation.3-9 With multiple options within a particular external fixator set, it is ideal to understand the benefit of using one component instead of another.
The main results from this experiment are: (1) constructs with pin-to-bar clamps and 2 crossbars are stiffer than those using multipin clamps and 2 crossbars; (2) constructs with a single crossbar and pin-to-bar clamps are as stiff as constructs using 2 crossbars and multipin clamps.
Figure 6 shows the average stiffness differences between the 8-mm and 11-mm–diameter bar constructs tested in this study. As expected, each 11-mm diameter–bar construct had a higher average stiffness compared with the 8-mm–diameter bar constructs. Across both the 8-mm and 11-mm–diameter bar constructs, construct 2 had a higher stiffness than that of constructs 1 and 3. Furthermore, there was no difference in the stiffness between constructs 1 and 3.
To improve external fixator stiffness, number of pins and optimization of pin spread can improve the strength of the construct.7 When using pin-to-bar clamps, 1 pin should be as close to the fracture as possible, with the second pin as far from the fracture as possible. 7 Multipin clamps, by design, prevent any optimization of pin spread and require a clustered-pin arrangement.
Bar configuration also plays a critical role in construct stiffness. Bar-to-bone distance should be approximately 2 fingerbreadths from the skin to maximize the stiffness of the construct.4,10-14 Multipin clamps use “bull horn” extensions that tend to elevate the bar away from the skin, increasing the distance between the bar and the bone.
A temporary spanning knee external fixator is commonly used for treating high-energy periarticular tibial or femoral fractures. To hold the fracture in an adequately reduced position, the frame must resist the deforming forces inherent with all fractures. A frame that is not adequately stiff will not hold the fracture in the reduced position, even at the time of initial surgery, which negates one of the benefits of placing the patient in the frame. Hence, adequate stiffness of the spanning-knee fixator is critical to the effectiveness of temporary stabilization before permanent fixation.
The results of this study provide evidence for the superiority of pin-to-bar clamps over multipin clamps in optimizing external fixator construct stiffness. At our institution, we almost exclusively use the single pin-to-bar clamps for spanning-knee external fixation. Based on the results of this study, we often use only a single crossbar. The ability to use a single bar greatly reduces the cost of the construct because crossbars can cost from $100 to $150, depending on the manufacturer.
A recent cost analysis of spanning-knee external fixators showed that construct costs can range from $8,000 to $19,000.15 The lower-cost constructs included 2 crossbars while the more expensive constructs had additional bars and multipin clamps. The authors noted that constructs with larger diameter bars and higher overall stiffness resulted in an improved cost per stiffness ratio. The results of this study support our conclusions regarding bar diameter. Additionally, our results show improved stiffness of constructs with pin-to-bar clamps instead of multipin clamps. By limiting the need for an additional bar, using pin-to-bar clamps and a single large diameter crossbar can create a very cost-efficient and rigidly stable construct.
One criticism of this study is the testing of used equipment. All external fixator manufacturers must evaluate and carefully examine any used equipment prior to the resterilization process and potential release to the practitioner for re-use. Our rationale for using used equipment is based on the assumption that the vast majority of patients do not have their external fixators removed because of failure but because of definitive surgical treatment, and the timing of removal does not necessarily follow a predetermined protocol. For example, timing of definitive surgery is usually set by the patient’s general health status, status of the soft tissues, and surgeon availability. Therefore, this equipment was tested with the presumption that the equipment was in the same state as if the patient continued to wear the frame 1 more day. A study testing unused equipment would be the next step in evaluating external fixators.
Another potential criticism of this study is the use of the same pin spread for constructs using pin-to-bar clamps and those using multipin clamps. We established that, to minimize confounding variables, a constant pin spread was necessary. This also mirrors our more common pin configurations for external fixators with pins placed outside the zone of injury. However, a key determinant of external fixator stability is pin spread, and this is a potential benefit to using pin-to-bar clamps over the multipin clamps that require an exact pin spread. Indeed, our results may have shown a larger difference between constructs using the pin-to-bar clamps compared with the multipin clamps had we maximized the pin spread. Future studies may be able to use a fracture model to compare the pin-to-bar clamps and multipin clamps using pin spread to maximize stability.
Conclusion
This study has shown that using pin-to-bar clamps can create strong, stable constructs for temporary external fixation. In particular, constructs made with a single bar and pin-to-bar clamps can produce easily implantable and less expensive constructs that are stiff enough to withstand deformation and allow patient transfers without excessive displacement of the fracture.
1. Behrens F. A primer of fixator devices and configurations. Clin Orthop Relat Res. 1989;241:5-14.
2. Chao EY, Aro HT, Lewallen DG, Kelly PJ. The effect of rigidity on fracture healing in external fixation. Clin Orthop Relat Res. 1989;241:24-35.
3. Schrøder HA, Weeth RE, Madsen T. Experimental analysis of Hoffman external fixation in various mountings. Arch Orthop Trauma Surg. 1985;104(4):197-200.
4. Kempson GE, Campbell D. The comparative stiffness of external fixation frames. Injury. 1981;12(4):297-304.
5. Giotakis N, Narayan B. Stability with unilateral external fixation in the tibia. Strategies Trauma Limb Reconstr. 2007;2(1):13-20.
6. Briggs BT, Chao EY. The mechanical performance of the standard Hoffmann-Vidal external fixation apparatus. J Bone Joint Surg Am. 1982;64(4):566-573.
7. Hipp JA, Edgerton BC, An KN, Hayes WC. Structural consequences of transcortical holes in long bones loaded in torsion. J Biomech. 1990;23(12):1261-1268.
8. Edgerton BC, An KN, Morrey BF. Torsional strength reduction due to cortical defects in bone. J Orthop Res. 1990;8(6):851-855.
9. Huiskes R, Chao E. Guidelines for external fixation frame rigidity and stresses. J Orthop Res. 1986;4(1):68-75.
10. Pettine KA, Chao EY, Kelly PJ. Analysis of the external fixator pin-bone interface. Clin Orthop Relat Res. 1993;(293):18-27.
11. Halsey D, Fleming B, Pope MH, Krag M, Kristiansen T. External fixator pin design. Clin Orthop Relat Res. 1992;(278):305-312.
12. Huiskes R, Chao EY, Crippen TE. Parametric analyses of pin-bone stresses in external fracture fixation devices. J Orthop Res. 1985;3(3):341-349.
13. Behrens F, Johnson W. Unilateral external fixation methods to increase and reduce frame stiffness. Clin Orthop Relat Res.1989;(241):48-56.
14. Mercer D, Firoozbakhsh K, Prevost M, Mulkey P, DeCoster TA, Schenck R. Stiffness of knee spanning external fixation systems for traumatic knee dislocations: a biomechanical study. J Orthop Trauma. 2010;24(11):693-696.
15. Kim H, Russell JP, Hsieh AH, O’Toole RV. Bar diameter is an important component of knee-spanning external fixator stiffness and cost. Orthopedics. 2014;37(7):e671-e677.
1. Behrens F. A primer of fixator devices and configurations. Clin Orthop Relat Res. 1989;241:5-14.
2. Chao EY, Aro HT, Lewallen DG, Kelly PJ. The effect of rigidity on fracture healing in external fixation. Clin Orthop Relat Res. 1989;241:24-35.
3. Schrøder HA, Weeth RE, Madsen T. Experimental analysis of Hoffman external fixation in various mountings. Arch Orthop Trauma Surg. 1985;104(4):197-200.
4. Kempson GE, Campbell D. The comparative stiffness of external fixation frames. Injury. 1981;12(4):297-304.
5. Giotakis N, Narayan B. Stability with unilateral external fixation in the tibia. Strategies Trauma Limb Reconstr. 2007;2(1):13-20.
6. Briggs BT, Chao EY. The mechanical performance of the standard Hoffmann-Vidal external fixation apparatus. J Bone Joint Surg Am. 1982;64(4):566-573.
7. Hipp JA, Edgerton BC, An KN, Hayes WC. Structural consequences of transcortical holes in long bones loaded in torsion. J Biomech. 1990;23(12):1261-1268.
8. Edgerton BC, An KN, Morrey BF. Torsional strength reduction due to cortical defects in bone. J Orthop Res. 1990;8(6):851-855.
9. Huiskes R, Chao E. Guidelines for external fixation frame rigidity and stresses. J Orthop Res. 1986;4(1):68-75.
10. Pettine KA, Chao EY, Kelly PJ. Analysis of the external fixator pin-bone interface. Clin Orthop Relat Res. 1993;(293):18-27.
11. Halsey D, Fleming B, Pope MH, Krag M, Kristiansen T. External fixator pin design. Clin Orthop Relat Res. 1992;(278):305-312.
12. Huiskes R, Chao EY, Crippen TE. Parametric analyses of pin-bone stresses in external fracture fixation devices. J Orthop Res. 1985;3(3):341-349.
13. Behrens F, Johnson W. Unilateral external fixation methods to increase and reduce frame stiffness. Clin Orthop Relat Res.1989;(241):48-56.
14. Mercer D, Firoozbakhsh K, Prevost M, Mulkey P, DeCoster TA, Schenck R. Stiffness of knee spanning external fixation systems for traumatic knee dislocations: a biomechanical study. J Orthop Trauma. 2010;24(11):693-696.
15. Kim H, Russell JP, Hsieh AH, O’Toole RV. Bar diameter is an important component of knee-spanning external fixator stiffness and cost. Orthopedics. 2014;37(7):e671-e677.