User login
ANSWER
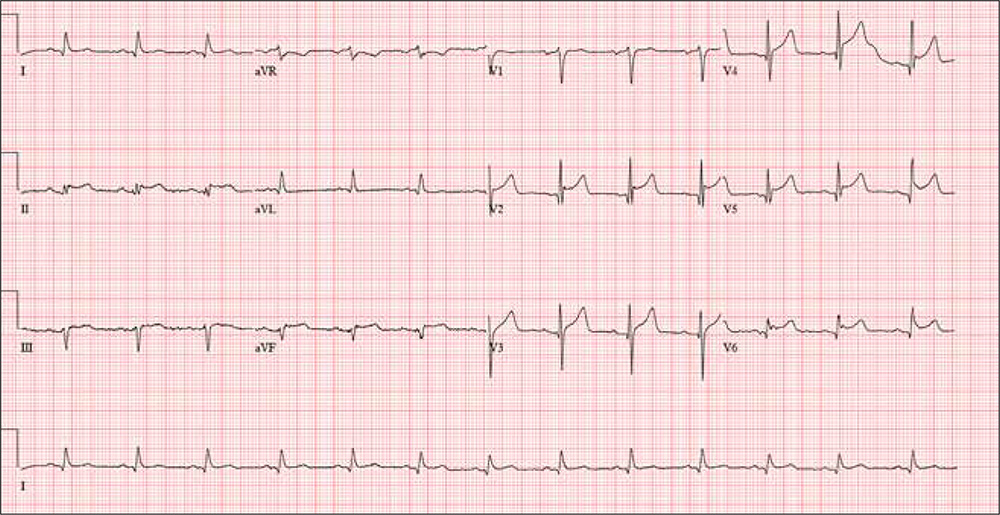
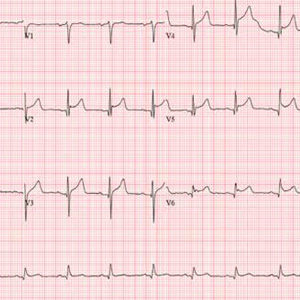
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
ANSWER
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
ANSWER
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
A 61-year-old avid cyclist is training for his third triathlon this year. About a week ago, after completing a 25-mile bike ride, he developed substernal chest discomfort, which he attributed to his longstanding history of GERD and his discontinuation of omeprazole. The discomfort resolved quickly with rest, and he was symptom free until two days ago. At that time, he “just rode through” the discomfort.
Today, however, about five miles into his ride, the discomfort was so severe that he stopped to wait for it to resolve. When it did not, he slowly rode another three miles to the urgent care center to request antacids and a prescription for a proton pump inhibitor.
He describes the problem as a combination of a burning sensation and a dull ache. It does not radiate beyond the substernal area. He denies shortness of breath and is not diaphoretic. He has never had hypertension, angina, dyspnea, syncope, or near-syncope.
His medical history is remarkable only for GERD. As a child, he sustained a nondisplaced fracture of his left clavicle. He has never had a surgical procedure.
The patient, an architect, is married with two adult children. He and his wife split a bottle of wine every other day, and he says he drinks 8 to 10 cups of coffee per day on average. He has never smoked tobacco or used recreational drugs.
Family history is remarkable for type 2 diabetes (father) and hypothyroidism (mother). Both parents are alive and otherwise well. The patient’s one sibling, a brother, died in a private plane accident.
Current medications include ibuprofen and chewable antacids. He took OTC omeprazole daily for about four months, but he recently ran out and hasn’t purchased more. He has a true anaphylactic allergy to sulfa.
Review of systems is unremarkable, other than typical muscle fatigue from cycling.
Vital signs include a blood pressure of 122/64 mm Hg; pulse, 80 beats/min, respiratory rate, 12 breaths/min-1; and temperature, 97.4°F. His height is 74 in and his weight, 184 lb.
The physical exam reveals an otherwise healthy-appearing male in no acute distress. He appears frustrated that he cannot get back out on his bike. There are no pertinent findings on physical exam. The lungs are clear, and the cardiac exam reveals a regular rate and rhythm with no murmurs, gallops, rubs, or extra heart sounds. The abdomen is soft and nontender, and there is no hepatojugular reflux. Peripheral pulses are strong bilaterally, and there are no neurologic focal signs.
The ECG reveals a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; Q axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation?