User login
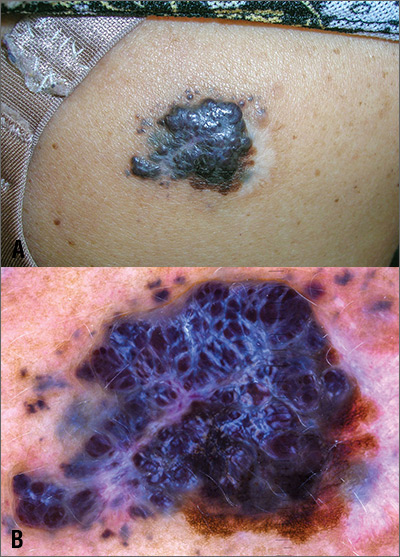
The FP was extremely concerned that this was a large melanoma due the lesion’s chaotic appearance, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the lesion was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was > 6 mm, and it was Enlarging by history.
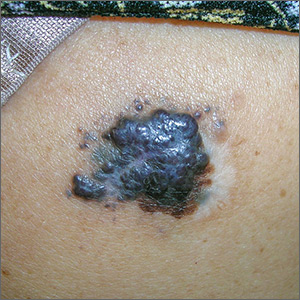
With his dermatoscope attached to his smart phone, the FP looked at the lesion and took a photograph (Figure B). The image revealed a pigment network of the original nevus at 5:00 to 6:00 o’clock and extensions of the tumor due to in-transit metastases. Satellites were visible, especially in the top right and left corners. The FP noted the shiny white lines caused by collagen deposition found in growing tumors. (See “Dermoscopy in family medicine: A primer.”)
The FP knew that the mass needed to be biopsied, but because of its size, the best he could do would be to perform a partial biopsy. So on the day of presentation, the FP performed a 6-mm punch biopsy in the most raised area of the lesion to try and get sufficient depth and breadth for diagnosis and prognosis. (See the Watch & Learn video on “Punch biopsy.”)
The pathology report indicated that the lesion was a nodular melanoma with a Breslow depth of 5.5 mm. This melanoma arose in a nevus, which occurs in about 30% of melanomas. Most melanomas arise de novo.
The FP referred the patient to a surgical oncologist for an excision with 2 cm margins and a sentinel lymph node biopsy. The sentinel node was in the right axilla and was remarkably negative despite the local in-transit metastases/satellites. One year after the original diagnosis was made, there was no evidence of metastatic disease and no new melanomas. The patient follows up with the dermatologist for skin and lymph node surveillance every 3 months.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill;2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP was extremely concerned that this was a large melanoma due the lesion’s chaotic appearance, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the lesion was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was > 6 mm, and it was Enlarging by history.
With his dermatoscope attached to his smart phone, the FP looked at the lesion and took a photograph (Figure B). The image revealed a pigment network of the original nevus at 5:00 to 6:00 o’clock and extensions of the tumor due to in-transit metastases. Satellites were visible, especially in the top right and left corners. The FP noted the shiny white lines caused by collagen deposition found in growing tumors. (See “Dermoscopy in family medicine: A primer.”)
The FP knew that the mass needed to be biopsied, but because of its size, the best he could do would be to perform a partial biopsy. So on the day of presentation, the FP performed a 6-mm punch biopsy in the most raised area of the lesion to try and get sufficient depth and breadth for diagnosis and prognosis. (See the Watch & Learn video on “Punch biopsy.”)
The pathology report indicated that the lesion was a nodular melanoma with a Breslow depth of 5.5 mm. This melanoma arose in a nevus, which occurs in about 30% of melanomas. Most melanomas arise de novo.
The FP referred the patient to a surgical oncologist for an excision with 2 cm margins and a sentinel lymph node biopsy. The sentinel node was in the right axilla and was remarkably negative despite the local in-transit metastases/satellites. One year after the original diagnosis was made, there was no evidence of metastatic disease and no new melanomas. The patient follows up with the dermatologist for skin and lymph node surveillance every 3 months.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill;2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com
The FP was extremely concerned that this was a large melanoma due the lesion’s chaotic appearance, with multiple colors and an irregular border. Going through the ABCDE criteria, he noted that the lesion was Asymmetric, the Border was irregular, the Colors were varied, the Diameter was > 6 mm, and it was Enlarging by history.
With his dermatoscope attached to his smart phone, the FP looked at the lesion and took a photograph (Figure B). The image revealed a pigment network of the original nevus at 5:00 to 6:00 o’clock and extensions of the tumor due to in-transit metastases. Satellites were visible, especially in the top right and left corners. The FP noted the shiny white lines caused by collagen deposition found in growing tumors. (See “Dermoscopy in family medicine: A primer.”)
The FP knew that the mass needed to be biopsied, but because of its size, the best he could do would be to perform a partial biopsy. So on the day of presentation, the FP performed a 6-mm punch biopsy in the most raised area of the lesion to try and get sufficient depth and breadth for diagnosis and prognosis. (See the Watch & Learn video on “Punch biopsy.”)
The pathology report indicated that the lesion was a nodular melanoma with a Breslow depth of 5.5 mm. This melanoma arose in a nevus, which occurs in about 30% of melanomas. Most melanomas arise de novo.
The FP referred the patient to a surgical oncologist for an excision with 2 cm margins and a sentinel lymph node biopsy. The sentinel node was in the right axilla and was remarkably negative despite the local in-transit metastases/satellites. One year after the original diagnosis was made, there was no evidence of metastatic disease and no new melanomas. The patient follows up with the dermatologist for skin and lymph node surveillance every 3 months.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Melanoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas and Synopsis of Family Medicine. 3rd ed. New York, NY: McGraw-Hill;2019:1112-1123.
To learn more about the newest 3rd edition of the Color Atlas and Synopsis of Family Medicine, see: https://www.amazon.com/Color-Atlas-Synopsis-Family-Medicine/dp/1259862046/
You can get the Color Atlas of Family Medicine app by clicking on this link: usatinemedia.com