User login
Teresa Marie Schiavo died on March 31, 2005, 15 years after sustaining a cardiac arrest and entering a persistent vegetative state (PVS). Her saga ignited national debates over the rights of the incapacitated, the outcomes of patients in persistent vegetative states, the basic requirements for human life, the distinction between nutrition and other medical treatments, and the involvement of the courts and politicians in our most private affairs. Sadly, Terri’s plight is not unique, and such a tragic predicament poses special challenges for hospitalists. The goals of this article are to review the definition and prognosis of PVS, and to outline the ethical argument for deciding to withdraw or withhold treatment from patients in PVS.
Clinical Features of the Persistent Vegetative State
Comatose patients may experience one of three general outcomes: recovery (partial or complete), death, or a prolonged or irreversible period of unconsciousness. As life support measures improved throughout the 1960s, this latter group represented an increasingly large yet ill-defined subgroup. In an attempt to characterize this population of severely brain-damaged patients who progress from coma to a state of wakefulness without awareness, Jennett and Plum coined the term “vegetative state” in 1972 (1). An estimated 10,000 to 25,000 adults in the United States exist in this manner for at least 1 month and are said to be in a persistent vegetative state.
In 1991, the Multi-Society Task Force on PVS was established and identified several key components of the condition (Table 1) (2). Hospitalists encounter patients who transition into PVS after an acute injury due to head trauma, or following nontraumatic diffuse bilateral cortical insult from prolonged hypoxic-ischemic periods. Less commonly, PVS is diagnosed in the hospital as an end-stage manifestation of a neurodegenerative illness. The cornerstone of PVS is diffuse cortical damage with relative preservation of brainstem and hypothalamic functions. Lacking cortical function, patients in PVS remain unaware of themselves or their environment, and are not thought to suffer. Many autonomic functions remain intact, however. PVS patients exhibit sleep-wake patterns, thermoregulate, maintain stable hemodynamics, respond with reflexive movements, and often live independent of a ventilator.
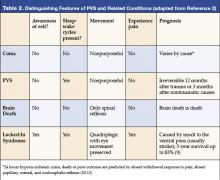
Several conditions have been confused with PVS (2). Coma is often applied inappropriately to patients in PVS. A lack of self-awareness characterizes both conditions; however, comatose patients (eyes closed, unresponsive) do not have recognizable sleep-wake cycles, whereas PVS patients exhibit wakefulness with open eyes. Key points of distinction between PVS, coma, brain death, and the locked-in syndrome are listed in Table 2.
Physical movements have traditionally been a source of confusion in PVS, and Terri Schiavo’s case was no exception. Politicians with medical backgrounds pointed to publicized video footage as evidence of her potential for recovery, or as an indication that a diagnosis of PVS had been made erroneously. In fact, PVS patients frequently exhibit truncal and limb movement, and they may smile, grimace, grunt, moan, or even cry on occasion. Some demonstrate a startle myoclonus and have preserved gag and cough reflexes. However, PVS patients do not exhibit sustained visual pursuit, visual fixation, or reproducible responses to threatening gestures. Because their ability to coordinate swallowing is impaired, most rely on alternative means to oral feeding and hydration for sustenance.
Prognosis in PVS
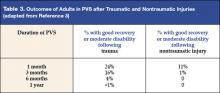
After 1 month has elapsed and a diagnosis of PVS is firmly established, attention focuses on prognosis. The Multi-Society Task Force reviewed the outcomes of 603 adults in PVS from traumatic and nontraumatic causes. Although PVS following trauma has a better prognosis than PVS following nontraumatic injury, the outcomes of both are poor (Table 3). Irreversibility is implied the longer a person remains in a vegetative state (3).
When does PVS become permanent?
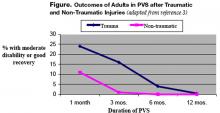
In their comprehensive review, the Task Force defined durations of PVS after which meaningful recovery is near impossible: 12 months following trauma and 3 months after nontraumatic injury (Figure) (3).
Twenty-four percent of patients who entered PVS following trauma improved to a point of moderate disability. However, once the duration of PVS exceeded 12 months, only 7 of 434 patients recovered. In all 7 cases, recovery was noted between 23 and 36 months after traumatic injury, but the patients’ functional status remained quite poor: 5 remained severely disabled, 1 was moderately disabled, and the status of the 7th could not be determined.
PVS following acute nontraumatic injury portends an even worse prognosis. Among 169 PVS patients in this category, 15% regained consciousness, and only 1 patient experienced a good recovery. After 3 months, the probability of recovery was less than 1%.
Based on the dismal outcomes after several months, how do we account for the occasional media reports of recovery after many years in vegetative states? The Task Force reviewed all such accounts and identified 5 patients with verified recovery after prolonged PVS, ranging in age from 18 to 61; all but 1 remained severely disabled. Following nontraumatic anoxic injury, the longest duration of PVS prior to regaining consciousness was 22 months (3). Given the prevalence of PVS, late recovery after PVS appears to be exceptionally rare. Following her anoxic injury, Terri Schiavo remained in PVS for 15 years—well beyond the 3-month cut-off for potential reversibility.
The Ethical Basis for Withdrawing Support in Patients with PVS
Life-sustaining treatment (LST) is most commonly withdrawn or withheld when this is known to be the patient’s preference either because of advance directives or through a surrogate representing the best interests of the patient. Conflicts arise when physicians recommend withdrawal of LST over the objections of surrogates. Faced with this dilemma, physicians caring for patients in PVS may cede to the wishes of the family. Alternatively, they may pursue withdrawal of LST based on 1 of the following 3 arguments:
- The perceived futility of ongoing LST;
- The presumption that patients in PVS have very poor quality of life and would opt for withdrawal if they could communicate their wishes; and
- The belief that patients in PVS no longer possess the minimal requirements for human existence and therefore have no interests to advance.
Is life-sustaining treatment futile for patients in PVS?
In its narrowest sense, futility implies the inability to achieve a particular physiologic goal because the treatment has no pathophysiologic basis, because the treatment has already been tried and failed in a patient, or because maximal therapy is failing (4). Invoking futility as a reason to withhold or withdraw care unilaterally in PVS is problematic. Because patients in PVS can remain alive for months to years with supportive measures, interventions (such as antibiotics or nutrition) are not futile, because the goal of prolonging life can be achieved, though at a markedly diminished level of quality.
Does PVS imply a presumption to withdraw LST?
Because futility cannot be invoked, some experts argue that PVS represents such a dismal quality of life that LST cannot be consistent with a patient’s best interests. While society generally errs on the side of prolonging the lives of incapacitated patients whose preferences are unknown, some ethicists argue that it should be presumed patients in PVS would not desire LST unless they have expressly stated preferences to the contrary. Public opinion polls support this notion, because the majority of people surveyed would not want LST if they were in PVS (5). This flexible position respects the divergent beliefs of the minority, permitting previously competent patients to continue LST when they choose.
Physicians who invoke this line of reasoning to override a surrogate’s decision explore relatively uncharted legal terrain. In the 1991 case of Helga Wanglie, an 87-year-old woman in a vegetative state, her husband wished to continue LST. Objecting to ongoing LST, her treating physicians attempted to remove the husband as legal guardian, but were rebuked (6). Without addressing the presumed desires of adults in PVS, the courts uphold the legal standing of surrogate decision-makers as long as they are acting in the patient’s best interests. On the other hand, a Massachusetts jury found that physicians were not guilty of malpractice when they entered a do-not-resuscitate order for a 71-year-old comatose woman without surrogate permission (5).
Do patients in PVS meet the minimal criteria for human existence?
A third ethical argument for withdrawing and withholding treatment in vegetative patients is unique to PVS. This line of reasoning challenges our assumptions about “patient interests” and resurrects the philosophical debate over the essence of human life. By virtue of being in PVS without hope for recovery, these patients have lost the minimal requirements of being human and have no hope of regaining them. In this view, prolonging mere biologic life is pointless because essential human qualities cannot be restored. This applies to patients in PVS for such duration that the probability of regaining consciousness is exceptionally rare (i.e., 12 months after trauma, or 3 months after nontraumatic injury). In such cases because no patient interests can be served and no medical goals are obtainable, no duty exists to provide life-sustaining treatment (7).
Physicians who choose to invoke this last argument should be aware of its uncertain legal and moral acceptance. Legally, the ethical argument that patients in PVS have no interests to advance has not been challenged directly in the courts. Groups rejecting the notion that patients in PVS lack minimal requirements for human life were galvanized by Terri Schiavo’s plight. Although public opinion polls determined that a clear majority would want their guardian to remove the feeding tube if they were in Terri’s predicament, a vocal minority was opposed (5). Politicians such as Congressman Tom DeLay entered the fray, declaring the removal of Terri’s feeding tube an “act of medical terrorism.” This right-to-life movement found an ally in the Roman Catholic Church when Pope John Paul II avowed that patients in PVS do, in fact, meet minimal criteria for human life and as such deserve nutrition and hydration (8). His opinion has yet to be adopted as doctrine, and political and moral consensus have not been achieved.
Conclusions
PVS is diagnosed 1 month after a patient enters a state of wakefulness without awareness. Movements are common in these patients, but they are not purposeful or reproducible in response to stimuli. Once PVS has exceeded durations of 3 months following nontraumatic injury or 12 months following trauma, the probability of meaningful recovery is exceptionally rare.
Armed with the above knowledge, what practical recourse exists to hospitalists caring for patients in PVS whose hope for regaining consciousness is exceedingly remote? First, inquire about advance directives that may direct care in such circumstances. If advance directives are not present, identify the surrogate decision maker, keeping in mind the state-to-state legal variations in the surrogate hierarchy. If the appropriate surrogate wishes to continue care and the treating physician objects, attempt to achieve a consensus. Time to adjust to the devastating plight and repeated nonjudgmental discussions focusing on the patient’s wishes often lead surrogates to accept withdrawal, or at least to establish limits on care (e.g., do-not-resuscitate order, withholding antibiotics and nutrition). Involvement of hospital ethics committees, primary care physicians, social workers, and religious or cultural ombudsmen may facilitate this process. Barring a mutually acceptable solution or progress in this direction, physicians may decide to cede to the wishes of the surrogates or, as a last recourse, involve the judicial system to achieve resolution.
References
- Jennett B. Plum F. Persistent vegetative state after brain damage: a syndrome in search of a name. Lancet. 1972; 1:734-7.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—first of two parts. NEJM. 1994; 330:1499-1508.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—second of two parts. NEJM. 1994; 330: 1572-9.
- Lo B. Resolving Ethical Dilemmas. A Guide for Clinicians. 2nd ed. Philadelphia, Pa: Lippincott Williams and Wilkins; p. 73.
- Eisenberg D. Lessons of the Schiavo battle. Time. April 4, 2005. pp. 26-27.
- Cantor NL. Can health care providers obtain judicial intervention against surrogates who demand “medically inappropriate” life support for incompetent patients? Crit Care Med. 1996; 24:883-87.
- Jonsen AR, Siegler M, and Winslade WJ. Clinical Ethics. A practical approach to ethical decisions in clinical practice. 5th ed. McGraw-Hill; p. 129.
- Address of Pope John Paul II to the participants in the international congress on “life-sustaining treatments and vegetative state: scientific advances and ethical dilemmas.” 20 March, 2004 available at: www.vatican.va/holy_father/john_paul_ii/speeches/2004/march/documents/hf_jp-ii_spe_20040320_congress-fiamc_en.html, Last accessed on May 11, 2005.
- Doble JE, Haig AJ, Anderson C, Katz R. Impairment, activity, participation, life satisfaction and survival in persons with locked-in syndrome for over a decade. J Head Trauma Rehabil. 2003;18:435-44.
- Booth CM, Boone RH, Tomlinson J, and Detsky AS. Is this patient dead, vegetative or severely impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004; 291:870-9.
- Levy DE, Caronna JJ, et al. Predicting coma from hypoxic-schemic coma. JAMA. 1985; 253:1420-6.
- Zandbergen EG, de Haan RJ, et al. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet. 1998; 352:1808-12.
Teresa Marie Schiavo died on March 31, 2005, 15 years after sustaining a cardiac arrest and entering a persistent vegetative state (PVS). Her saga ignited national debates over the rights of the incapacitated, the outcomes of patients in persistent vegetative states, the basic requirements for human life, the distinction between nutrition and other medical treatments, and the involvement of the courts and politicians in our most private affairs. Sadly, Terri’s plight is not unique, and such a tragic predicament poses special challenges for hospitalists. The goals of this article are to review the definition and prognosis of PVS, and to outline the ethical argument for deciding to withdraw or withhold treatment from patients in PVS.
Clinical Features of the Persistent Vegetative State
Comatose patients may experience one of three general outcomes: recovery (partial or complete), death, or a prolonged or irreversible period of unconsciousness. As life support measures improved throughout the 1960s, this latter group represented an increasingly large yet ill-defined subgroup. In an attempt to characterize this population of severely brain-damaged patients who progress from coma to a state of wakefulness without awareness, Jennett and Plum coined the term “vegetative state” in 1972 (1). An estimated 10,000 to 25,000 adults in the United States exist in this manner for at least 1 month and are said to be in a persistent vegetative state.
In 1991, the Multi-Society Task Force on PVS was established and identified several key components of the condition (Table 1) (2). Hospitalists encounter patients who transition into PVS after an acute injury due to head trauma, or following nontraumatic diffuse bilateral cortical insult from prolonged hypoxic-ischemic periods. Less commonly, PVS is diagnosed in the hospital as an end-stage manifestation of a neurodegenerative illness. The cornerstone of PVS is diffuse cortical damage with relative preservation of brainstem and hypothalamic functions. Lacking cortical function, patients in PVS remain unaware of themselves or their environment, and are not thought to suffer. Many autonomic functions remain intact, however. PVS patients exhibit sleep-wake patterns, thermoregulate, maintain stable hemodynamics, respond with reflexive movements, and often live independent of a ventilator.
Several conditions have been confused with PVS (2). Coma is often applied inappropriately to patients in PVS. A lack of self-awareness characterizes both conditions; however, comatose patients (eyes closed, unresponsive) do not have recognizable sleep-wake cycles, whereas PVS patients exhibit wakefulness with open eyes. Key points of distinction between PVS, coma, brain death, and the locked-in syndrome are listed in Table 2.
Physical movements have traditionally been a source of confusion in PVS, and Terri Schiavo’s case was no exception. Politicians with medical backgrounds pointed to publicized video footage as evidence of her potential for recovery, or as an indication that a diagnosis of PVS had been made erroneously. In fact, PVS patients frequently exhibit truncal and limb movement, and they may smile, grimace, grunt, moan, or even cry on occasion. Some demonstrate a startle myoclonus and have preserved gag and cough reflexes. However, PVS patients do not exhibit sustained visual pursuit, visual fixation, or reproducible responses to threatening gestures. Because their ability to coordinate swallowing is impaired, most rely on alternative means to oral feeding and hydration for sustenance.
Prognosis in PVS
After 1 month has elapsed and a diagnosis of PVS is firmly established, attention focuses on prognosis. The Multi-Society Task Force reviewed the outcomes of 603 adults in PVS from traumatic and nontraumatic causes. Although PVS following trauma has a better prognosis than PVS following nontraumatic injury, the outcomes of both are poor (Table 3). Irreversibility is implied the longer a person remains in a vegetative state (3).
When does PVS become permanent?
In their comprehensive review, the Task Force defined durations of PVS after which meaningful recovery is near impossible: 12 months following trauma and 3 months after nontraumatic injury (Figure) (3).
Twenty-four percent of patients who entered PVS following trauma improved to a point of moderate disability. However, once the duration of PVS exceeded 12 months, only 7 of 434 patients recovered. In all 7 cases, recovery was noted between 23 and 36 months after traumatic injury, but the patients’ functional status remained quite poor: 5 remained severely disabled, 1 was moderately disabled, and the status of the 7th could not be determined.
PVS following acute nontraumatic injury portends an even worse prognosis. Among 169 PVS patients in this category, 15% regained consciousness, and only 1 patient experienced a good recovery. After 3 months, the probability of recovery was less than 1%.
Based on the dismal outcomes after several months, how do we account for the occasional media reports of recovery after many years in vegetative states? The Task Force reviewed all such accounts and identified 5 patients with verified recovery after prolonged PVS, ranging in age from 18 to 61; all but 1 remained severely disabled. Following nontraumatic anoxic injury, the longest duration of PVS prior to regaining consciousness was 22 months (3). Given the prevalence of PVS, late recovery after PVS appears to be exceptionally rare. Following her anoxic injury, Terri Schiavo remained in PVS for 15 years—well beyond the 3-month cut-off for potential reversibility.
The Ethical Basis for Withdrawing Support in Patients with PVS
Life-sustaining treatment (LST) is most commonly withdrawn or withheld when this is known to be the patient’s preference either because of advance directives or through a surrogate representing the best interests of the patient. Conflicts arise when physicians recommend withdrawal of LST over the objections of surrogates. Faced with this dilemma, physicians caring for patients in PVS may cede to the wishes of the family. Alternatively, they may pursue withdrawal of LST based on 1 of the following 3 arguments:
- The perceived futility of ongoing LST;
- The presumption that patients in PVS have very poor quality of life and would opt for withdrawal if they could communicate their wishes; and
- The belief that patients in PVS no longer possess the minimal requirements for human existence and therefore have no interests to advance.
Is life-sustaining treatment futile for patients in PVS?
In its narrowest sense, futility implies the inability to achieve a particular physiologic goal because the treatment has no pathophysiologic basis, because the treatment has already been tried and failed in a patient, or because maximal therapy is failing (4). Invoking futility as a reason to withhold or withdraw care unilaterally in PVS is problematic. Because patients in PVS can remain alive for months to years with supportive measures, interventions (such as antibiotics or nutrition) are not futile, because the goal of prolonging life can be achieved, though at a markedly diminished level of quality.
Does PVS imply a presumption to withdraw LST?
Because futility cannot be invoked, some experts argue that PVS represents such a dismal quality of life that LST cannot be consistent with a patient’s best interests. While society generally errs on the side of prolonging the lives of incapacitated patients whose preferences are unknown, some ethicists argue that it should be presumed patients in PVS would not desire LST unless they have expressly stated preferences to the contrary. Public opinion polls support this notion, because the majority of people surveyed would not want LST if they were in PVS (5). This flexible position respects the divergent beliefs of the minority, permitting previously competent patients to continue LST when they choose.
Physicians who invoke this line of reasoning to override a surrogate’s decision explore relatively uncharted legal terrain. In the 1991 case of Helga Wanglie, an 87-year-old woman in a vegetative state, her husband wished to continue LST. Objecting to ongoing LST, her treating physicians attempted to remove the husband as legal guardian, but were rebuked (6). Without addressing the presumed desires of adults in PVS, the courts uphold the legal standing of surrogate decision-makers as long as they are acting in the patient’s best interests. On the other hand, a Massachusetts jury found that physicians were not guilty of malpractice when they entered a do-not-resuscitate order for a 71-year-old comatose woman without surrogate permission (5).
Do patients in PVS meet the minimal criteria for human existence?
A third ethical argument for withdrawing and withholding treatment in vegetative patients is unique to PVS. This line of reasoning challenges our assumptions about “patient interests” and resurrects the philosophical debate over the essence of human life. By virtue of being in PVS without hope for recovery, these patients have lost the minimal requirements of being human and have no hope of regaining them. In this view, prolonging mere biologic life is pointless because essential human qualities cannot be restored. This applies to patients in PVS for such duration that the probability of regaining consciousness is exceptionally rare (i.e., 12 months after trauma, or 3 months after nontraumatic injury). In such cases because no patient interests can be served and no medical goals are obtainable, no duty exists to provide life-sustaining treatment (7).
Physicians who choose to invoke this last argument should be aware of its uncertain legal and moral acceptance. Legally, the ethical argument that patients in PVS have no interests to advance has not been challenged directly in the courts. Groups rejecting the notion that patients in PVS lack minimal requirements for human life were galvanized by Terri Schiavo’s plight. Although public opinion polls determined that a clear majority would want their guardian to remove the feeding tube if they were in Terri’s predicament, a vocal minority was opposed (5). Politicians such as Congressman Tom DeLay entered the fray, declaring the removal of Terri’s feeding tube an “act of medical terrorism.” This right-to-life movement found an ally in the Roman Catholic Church when Pope John Paul II avowed that patients in PVS do, in fact, meet minimal criteria for human life and as such deserve nutrition and hydration (8). His opinion has yet to be adopted as doctrine, and political and moral consensus have not been achieved.
Conclusions
PVS is diagnosed 1 month after a patient enters a state of wakefulness without awareness. Movements are common in these patients, but they are not purposeful or reproducible in response to stimuli. Once PVS has exceeded durations of 3 months following nontraumatic injury or 12 months following trauma, the probability of meaningful recovery is exceptionally rare.
Armed with the above knowledge, what practical recourse exists to hospitalists caring for patients in PVS whose hope for regaining consciousness is exceedingly remote? First, inquire about advance directives that may direct care in such circumstances. If advance directives are not present, identify the surrogate decision maker, keeping in mind the state-to-state legal variations in the surrogate hierarchy. If the appropriate surrogate wishes to continue care and the treating physician objects, attempt to achieve a consensus. Time to adjust to the devastating plight and repeated nonjudgmental discussions focusing on the patient’s wishes often lead surrogates to accept withdrawal, or at least to establish limits on care (e.g., do-not-resuscitate order, withholding antibiotics and nutrition). Involvement of hospital ethics committees, primary care physicians, social workers, and religious or cultural ombudsmen may facilitate this process. Barring a mutually acceptable solution or progress in this direction, physicians may decide to cede to the wishes of the surrogates or, as a last recourse, involve the judicial system to achieve resolution.
References
- Jennett B. Plum F. Persistent vegetative state after brain damage: a syndrome in search of a name. Lancet. 1972; 1:734-7.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—first of two parts. NEJM. 1994; 330:1499-1508.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—second of two parts. NEJM. 1994; 330: 1572-9.
- Lo B. Resolving Ethical Dilemmas. A Guide for Clinicians. 2nd ed. Philadelphia, Pa: Lippincott Williams and Wilkins; p. 73.
- Eisenberg D. Lessons of the Schiavo battle. Time. April 4, 2005. pp. 26-27.
- Cantor NL. Can health care providers obtain judicial intervention against surrogates who demand “medically inappropriate” life support for incompetent patients? Crit Care Med. 1996; 24:883-87.
- Jonsen AR, Siegler M, and Winslade WJ. Clinical Ethics. A practical approach to ethical decisions in clinical practice. 5th ed. McGraw-Hill; p. 129.
- Address of Pope John Paul II to the participants in the international congress on “life-sustaining treatments and vegetative state: scientific advances and ethical dilemmas.” 20 March, 2004 available at: www.vatican.va/holy_father/john_paul_ii/speeches/2004/march/documents/hf_jp-ii_spe_20040320_congress-fiamc_en.html, Last accessed on May 11, 2005.
- Doble JE, Haig AJ, Anderson C, Katz R. Impairment, activity, participation, life satisfaction and survival in persons with locked-in syndrome for over a decade. J Head Trauma Rehabil. 2003;18:435-44.
- Booth CM, Boone RH, Tomlinson J, and Detsky AS. Is this patient dead, vegetative or severely impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004; 291:870-9.
- Levy DE, Caronna JJ, et al. Predicting coma from hypoxic-schemic coma. JAMA. 1985; 253:1420-6.
- Zandbergen EG, de Haan RJ, et al. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet. 1998; 352:1808-12.
Teresa Marie Schiavo died on March 31, 2005, 15 years after sustaining a cardiac arrest and entering a persistent vegetative state (PVS). Her saga ignited national debates over the rights of the incapacitated, the outcomes of patients in persistent vegetative states, the basic requirements for human life, the distinction between nutrition and other medical treatments, and the involvement of the courts and politicians in our most private affairs. Sadly, Terri’s plight is not unique, and such a tragic predicament poses special challenges for hospitalists. The goals of this article are to review the definition and prognosis of PVS, and to outline the ethical argument for deciding to withdraw or withhold treatment from patients in PVS.
Clinical Features of the Persistent Vegetative State
Comatose patients may experience one of three general outcomes: recovery (partial or complete), death, or a prolonged or irreversible period of unconsciousness. As life support measures improved throughout the 1960s, this latter group represented an increasingly large yet ill-defined subgroup. In an attempt to characterize this population of severely brain-damaged patients who progress from coma to a state of wakefulness without awareness, Jennett and Plum coined the term “vegetative state” in 1972 (1). An estimated 10,000 to 25,000 adults in the United States exist in this manner for at least 1 month and are said to be in a persistent vegetative state.
In 1991, the Multi-Society Task Force on PVS was established and identified several key components of the condition (Table 1) (2). Hospitalists encounter patients who transition into PVS after an acute injury due to head trauma, or following nontraumatic diffuse bilateral cortical insult from prolonged hypoxic-ischemic periods. Less commonly, PVS is diagnosed in the hospital as an end-stage manifestation of a neurodegenerative illness. The cornerstone of PVS is diffuse cortical damage with relative preservation of brainstem and hypothalamic functions. Lacking cortical function, patients in PVS remain unaware of themselves or their environment, and are not thought to suffer. Many autonomic functions remain intact, however. PVS patients exhibit sleep-wake patterns, thermoregulate, maintain stable hemodynamics, respond with reflexive movements, and often live independent of a ventilator.
Several conditions have been confused with PVS (2). Coma is often applied inappropriately to patients in PVS. A lack of self-awareness characterizes both conditions; however, comatose patients (eyes closed, unresponsive) do not have recognizable sleep-wake cycles, whereas PVS patients exhibit wakefulness with open eyes. Key points of distinction between PVS, coma, brain death, and the locked-in syndrome are listed in Table 2.
Physical movements have traditionally been a source of confusion in PVS, and Terri Schiavo’s case was no exception. Politicians with medical backgrounds pointed to publicized video footage as evidence of her potential for recovery, or as an indication that a diagnosis of PVS had been made erroneously. In fact, PVS patients frequently exhibit truncal and limb movement, and they may smile, grimace, grunt, moan, or even cry on occasion. Some demonstrate a startle myoclonus and have preserved gag and cough reflexes. However, PVS patients do not exhibit sustained visual pursuit, visual fixation, or reproducible responses to threatening gestures. Because their ability to coordinate swallowing is impaired, most rely on alternative means to oral feeding and hydration for sustenance.
Prognosis in PVS
After 1 month has elapsed and a diagnosis of PVS is firmly established, attention focuses on prognosis. The Multi-Society Task Force reviewed the outcomes of 603 adults in PVS from traumatic and nontraumatic causes. Although PVS following trauma has a better prognosis than PVS following nontraumatic injury, the outcomes of both are poor (Table 3). Irreversibility is implied the longer a person remains in a vegetative state (3).
When does PVS become permanent?
In their comprehensive review, the Task Force defined durations of PVS after which meaningful recovery is near impossible: 12 months following trauma and 3 months after nontraumatic injury (Figure) (3).
Twenty-four percent of patients who entered PVS following trauma improved to a point of moderate disability. However, once the duration of PVS exceeded 12 months, only 7 of 434 patients recovered. In all 7 cases, recovery was noted between 23 and 36 months after traumatic injury, but the patients’ functional status remained quite poor: 5 remained severely disabled, 1 was moderately disabled, and the status of the 7th could not be determined.
PVS following acute nontraumatic injury portends an even worse prognosis. Among 169 PVS patients in this category, 15% regained consciousness, and only 1 patient experienced a good recovery. After 3 months, the probability of recovery was less than 1%.
Based on the dismal outcomes after several months, how do we account for the occasional media reports of recovery after many years in vegetative states? The Task Force reviewed all such accounts and identified 5 patients with verified recovery after prolonged PVS, ranging in age from 18 to 61; all but 1 remained severely disabled. Following nontraumatic anoxic injury, the longest duration of PVS prior to regaining consciousness was 22 months (3). Given the prevalence of PVS, late recovery after PVS appears to be exceptionally rare. Following her anoxic injury, Terri Schiavo remained in PVS for 15 years—well beyond the 3-month cut-off for potential reversibility.
The Ethical Basis for Withdrawing Support in Patients with PVS
Life-sustaining treatment (LST) is most commonly withdrawn or withheld when this is known to be the patient’s preference either because of advance directives or through a surrogate representing the best interests of the patient. Conflicts arise when physicians recommend withdrawal of LST over the objections of surrogates. Faced with this dilemma, physicians caring for patients in PVS may cede to the wishes of the family. Alternatively, they may pursue withdrawal of LST based on 1 of the following 3 arguments:
- The perceived futility of ongoing LST;
- The presumption that patients in PVS have very poor quality of life and would opt for withdrawal if they could communicate their wishes; and
- The belief that patients in PVS no longer possess the minimal requirements for human existence and therefore have no interests to advance.
Is life-sustaining treatment futile for patients in PVS?
In its narrowest sense, futility implies the inability to achieve a particular physiologic goal because the treatment has no pathophysiologic basis, because the treatment has already been tried and failed in a patient, or because maximal therapy is failing (4). Invoking futility as a reason to withhold or withdraw care unilaterally in PVS is problematic. Because patients in PVS can remain alive for months to years with supportive measures, interventions (such as antibiotics or nutrition) are not futile, because the goal of prolonging life can be achieved, though at a markedly diminished level of quality.
Does PVS imply a presumption to withdraw LST?
Because futility cannot be invoked, some experts argue that PVS represents such a dismal quality of life that LST cannot be consistent with a patient’s best interests. While society generally errs on the side of prolonging the lives of incapacitated patients whose preferences are unknown, some ethicists argue that it should be presumed patients in PVS would not desire LST unless they have expressly stated preferences to the contrary. Public opinion polls support this notion, because the majority of people surveyed would not want LST if they were in PVS (5). This flexible position respects the divergent beliefs of the minority, permitting previously competent patients to continue LST when they choose.
Physicians who invoke this line of reasoning to override a surrogate’s decision explore relatively uncharted legal terrain. In the 1991 case of Helga Wanglie, an 87-year-old woman in a vegetative state, her husband wished to continue LST. Objecting to ongoing LST, her treating physicians attempted to remove the husband as legal guardian, but were rebuked (6). Without addressing the presumed desires of adults in PVS, the courts uphold the legal standing of surrogate decision-makers as long as they are acting in the patient’s best interests. On the other hand, a Massachusetts jury found that physicians were not guilty of malpractice when they entered a do-not-resuscitate order for a 71-year-old comatose woman without surrogate permission (5).
Do patients in PVS meet the minimal criteria for human existence?
A third ethical argument for withdrawing and withholding treatment in vegetative patients is unique to PVS. This line of reasoning challenges our assumptions about “patient interests” and resurrects the philosophical debate over the essence of human life. By virtue of being in PVS without hope for recovery, these patients have lost the minimal requirements of being human and have no hope of regaining them. In this view, prolonging mere biologic life is pointless because essential human qualities cannot be restored. This applies to patients in PVS for such duration that the probability of regaining consciousness is exceptionally rare (i.e., 12 months after trauma, or 3 months after nontraumatic injury). In such cases because no patient interests can be served and no medical goals are obtainable, no duty exists to provide life-sustaining treatment (7).
Physicians who choose to invoke this last argument should be aware of its uncertain legal and moral acceptance. Legally, the ethical argument that patients in PVS have no interests to advance has not been challenged directly in the courts. Groups rejecting the notion that patients in PVS lack minimal requirements for human life were galvanized by Terri Schiavo’s plight. Although public opinion polls determined that a clear majority would want their guardian to remove the feeding tube if they were in Terri’s predicament, a vocal minority was opposed (5). Politicians such as Congressman Tom DeLay entered the fray, declaring the removal of Terri’s feeding tube an “act of medical terrorism.” This right-to-life movement found an ally in the Roman Catholic Church when Pope John Paul II avowed that patients in PVS do, in fact, meet minimal criteria for human life and as such deserve nutrition and hydration (8). His opinion has yet to be adopted as doctrine, and political and moral consensus have not been achieved.
Conclusions
PVS is diagnosed 1 month after a patient enters a state of wakefulness without awareness. Movements are common in these patients, but they are not purposeful or reproducible in response to stimuli. Once PVS has exceeded durations of 3 months following nontraumatic injury or 12 months following trauma, the probability of meaningful recovery is exceptionally rare.
Armed with the above knowledge, what practical recourse exists to hospitalists caring for patients in PVS whose hope for regaining consciousness is exceedingly remote? First, inquire about advance directives that may direct care in such circumstances. If advance directives are not present, identify the surrogate decision maker, keeping in mind the state-to-state legal variations in the surrogate hierarchy. If the appropriate surrogate wishes to continue care and the treating physician objects, attempt to achieve a consensus. Time to adjust to the devastating plight and repeated nonjudgmental discussions focusing on the patient’s wishes often lead surrogates to accept withdrawal, or at least to establish limits on care (e.g., do-not-resuscitate order, withholding antibiotics and nutrition). Involvement of hospital ethics committees, primary care physicians, social workers, and religious or cultural ombudsmen may facilitate this process. Barring a mutually acceptable solution or progress in this direction, physicians may decide to cede to the wishes of the surrogates or, as a last recourse, involve the judicial system to achieve resolution.
References
- Jennett B. Plum F. Persistent vegetative state after brain damage: a syndrome in search of a name. Lancet. 1972; 1:734-7.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—first of two parts. NEJM. 1994; 330:1499-1508.
- The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state—second of two parts. NEJM. 1994; 330: 1572-9.
- Lo B. Resolving Ethical Dilemmas. A Guide for Clinicians. 2nd ed. Philadelphia, Pa: Lippincott Williams and Wilkins; p. 73.
- Eisenberg D. Lessons of the Schiavo battle. Time. April 4, 2005. pp. 26-27.
- Cantor NL. Can health care providers obtain judicial intervention against surrogates who demand “medically inappropriate” life support for incompetent patients? Crit Care Med. 1996; 24:883-87.
- Jonsen AR, Siegler M, and Winslade WJ. Clinical Ethics. A practical approach to ethical decisions in clinical practice. 5th ed. McGraw-Hill; p. 129.
- Address of Pope John Paul II to the participants in the international congress on “life-sustaining treatments and vegetative state: scientific advances and ethical dilemmas.” 20 March, 2004 available at: www.vatican.va/holy_father/john_paul_ii/speeches/2004/march/documents/hf_jp-ii_spe_20040320_congress-fiamc_en.html, Last accessed on May 11, 2005.
- Doble JE, Haig AJ, Anderson C, Katz R. Impairment, activity, participation, life satisfaction and survival in persons with locked-in syndrome for over a decade. J Head Trauma Rehabil. 2003;18:435-44.
- Booth CM, Boone RH, Tomlinson J, and Detsky AS. Is this patient dead, vegetative or severely impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004; 291:870-9.
- Levy DE, Caronna JJ, et al. Predicting coma from hypoxic-schemic coma. JAMA. 1985; 253:1420-6.
- Zandbergen EG, de Haan RJ, et al. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet. 1998; 352:1808-12.