User login
ANSWER
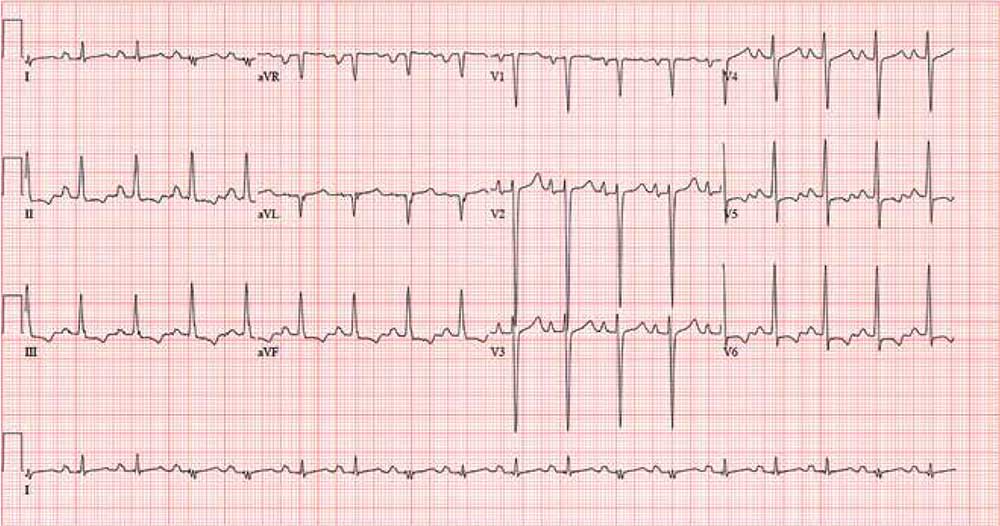
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
ANSWER
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
ANSWER
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
A 34-year-old man with a history of malignant hypertension is brought to the emergency department via ACLS ambulance with substernal chest pain and a field blood pressure of 228/136 mm Hg. According to the paramedics, the patient’s symptoms include dyspnea, emotional lability, agitation, and violent behavior requiring physical restraints.
The patient is known at your institution (and many others in the area) for his frequent admissions and poor compliance with medications. Today, the patient’s agitation and paranoia prevent you from obtaining a clear history of the present illness. You do learn that he recently started working in a meth lab, where he has had free access to illicit substances.
His toxicology screen is positive for methamphetamines, cocaine, and phencyclidine. Additional lab tests indicate elevated serial troponin levels, diagnostic of non-ST-segment elevation myocardial infarction (NSTEMI), and an elevated B-type natriuretic peptide level, compatible with congestive
A review of his electronic medical record reveals allergies to sulfa and erythromycin. His medication list includes carvedilol (6.25 mg bid), furosemide (40 mg/d), and lisinopril (20 mg bid), with multiple references to noncompliance. You also note that he has had several skin and soft-tissue infections requiring both oral and IV antibiotic therapy.
The patient’s vital signs on arrival include a blood pressure of 210/140 mm Hg; pulse, 110 beats/min; respiratory rate, 20 breaths/min-1; and temperature, 38.2°C. His weight is 147 lb and his height, 69 in.
Physical exam reveals a man who appears agitated, restless, and psychotic. His skin is remarkable for multiple excoriated lesions on both upper and lower extremities. Recent needle tracks are present in both antecubital fossae.
The HEENT exam is remarkable for enlarged pupils and exophthalmos. Punctate lesions are seen on the nasal septum, and the teeth are in poor repair with multiple caries. The neck is supple, with a palpable thyroid and no evidence of jugular venous distention.
Pulmonary sounds reveal coarse rhonchi in both bases, with no evidence of wheezing. The cardiac exam reveals tachycardia with a regular rate and no extra heart sounds or murmurs. Peripheral pulses are strong and equal bilaterally. The abdominal exam is remarkable for diffuse tenderness to palpation without focal pain, as well as a firm liver edge 2 cm below the right costal margin. The neurologic exam is remarkable for agitation, paranoia, and psychosis. There are no focal cranial nerve defects.
Workup—including chest and abdominal CT, echocardiogram, and ECG—is ordered. The ECG reveals a ventricular rate of 105 beats/min; PR interval, 170 ms; QRS duration, 96 ms; QT/QTc interval, 362/478 ms; P axis, 54°; R axis, 81°; and T axis, –59°. What is your interpretation?