User login
Tumor of the follicular infundibulum (TFI) was first described by Mehregan and Butler1 in a patient with multiple papules. It typically presents as a solitary lesion that mainly affects the face, neck, and upper trunk, and it generally occurs in elderly patients with a female predilection and occasional vulvar involvement. Sometimes TFI may coexist with an unusual trichilemmal tumor or basal cell carcinoma (BCC) with sebaceous or sweat duct differentiation. Other features of TFI include an eosinophilic cuticle, ductal differentiation, coronoid lamellae, and desmoplasia. Interestingly, approximately one-fourth of reported TFIs were found to be associated with other cutaneous lesions, including BCC, actinic keratosis, desmoplastic malignant melanoma, junctional melanocytic nevus, trichilemmoma, and epidermal inclusion cyst.2 Eruptive forms of TFI are rare, presenting as macules, smooth or slightly keratotic papules, or depressed lesions with a flesh-colored erythematous or hypopigmented appearance. We report the case of a 49-year-old woman with multiple TFIs and some new features.
Case Report
A 49-year-old woman presented with multiple lesions on the arms, shoulders, trunk, buttocks, and legs of more than 3 years’ duration. According to the patient, multiple small, reddish papules gradually appeared on the arms and legs approximately 3 years prior to presentation and were accompanied by considerable pruritus. She sought medical assistance several times at local clinics. A diagnosis of eczema and prurigo was made and oral antihistamines and topical glucocorticoids were administered for more than 2 years. The pruritus was controlled to some degree but recurred after discontinuation of treatment. Five months later, the lesions flared up suddenly and rapidly to the back and buttocks, just around the skin areas treated with cupping glass, a traditional Chinese therapy, for heat syncope. She reported constant itching that kept her awake at night.
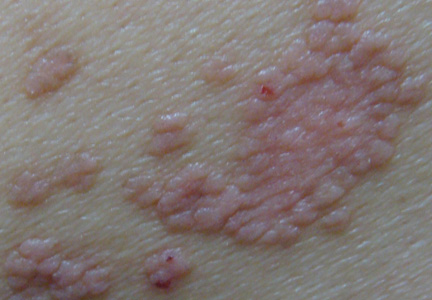
Physical examination revealed hundreds of erythematous maculopapules scattered over the arms, shoulders, trunk, buttocks, and legs. The individual lesions were minimally elevated, irregularly shaped, and slightly scaly, and they were distributed in a relatively symmetrical manner. Some of the lesions coalesced to form small plaques measuring approximately 0.5 to 3 cm in diameter (Figure 1). Interestingly, several annulated lesions with a hypopigmented center and hyperpigmented periphery could be observed at areas treated with cupping glass, showing a typical presentation of the Köbner phenomenon (Figure 2). No obvious association with sun exposure or hair loss was detected. The patient’s medical history was unremarkable and there was no known family history of similar skin lesions.
|
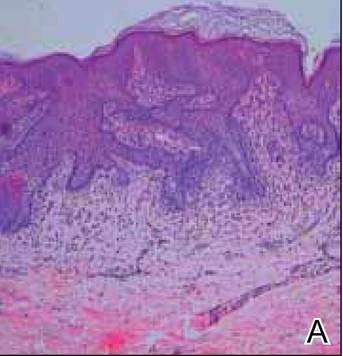
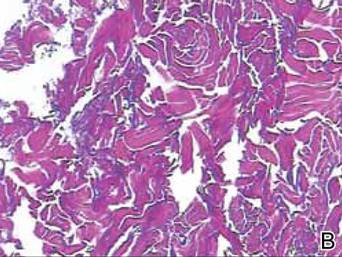
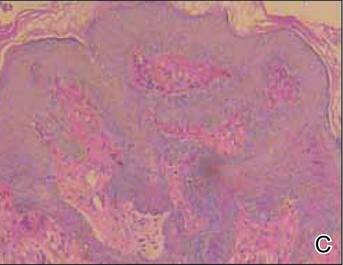
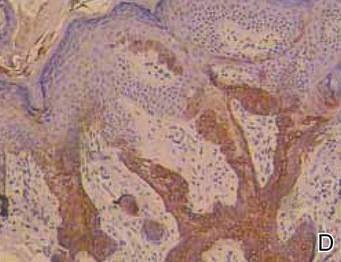
The differential diagnosis included lichen planus, prurigo, and adnexal tumors. Histopathologic examination of biopsies from lesions on the back and around the cupping glass areas revealed a benign platelike proliferation of pale-staining epithelial cells in the papillary dermis connected to the overlying epidermis with a moderate lymphatic cell infiltration (Figure 3A). Weigert staining revealed a network of elastic fibers surrounding the base of the tumor (Figure 3B). The pale epithelial cells were positive on periodic acid–Schiff staining (Figure 3C). Immunohistochemical staining revealed that the proliferation was positive for keratin 17 (Figure 3D).
These striking clinical and histological findings suggested the lesions were multiple TFIs. Treatment with tretinoin ointment 0.1% twice daily for 2 months was ineffective. The patient refused treatment with either oral acitretin or dapsone or invasive techniques such as lasers and cryotherapy. She has been on careful follow-up for the last 2 years with new lesions appearing intermittently.
Comment
The etiology of TFI still is unknown but may be related to environmental factors or genetic changes. Tumors of the follicular infundibulum generally are classified as solitary, eruptive, associated with other lesions of Cowden disease, associated with a single tumor, or TFI-like epidermal changes.3 The eruptive form has seldom been reported to date. Eruptive TFIs are nonspecific, ranging in number from several to more than 100. Clinical characteristics and distribution of the lesions can vary from patient to patient, but the lesions tend to be quite monomorphous, even in cases with more than 100 lesions.4 Histopathologic features usually are typical and distinctive, allowing its definite diagnosis. To confirm the diagnosis, the immunohistochemical profile may be useful to characterize its follicular origin, which is positive for keratin 17. Tumors of the follicular infundibulum usually are benign; however, in one patient with more than 100 lesions, there was documented transformation into BCC.5 Due to the potential for malignant transformation as well as its occurrence within the spectrum of lesions associated with Cowden disease,6,7 long-term supervision of TFI is strongly recommended, as was the case with our patient.
A remarkable feature in our case was the patient’s severe pruritus, as most reported cases have been asymptomatic. The increased association with other cutaneous lesions,2 the Köbner phenomenon, and the underlying inflammatory cell infiltration of the tumors in our case strongly suggested that eruptive TFI may represent a kind of cutaneous reaction.
|
Conclusion
The clinical findings of severe pruritus and the Köbner phenomenon in our patient further expand the constellation of the clinical presentation of the eruptive variant of TFI.
1. Mehregan AH, Butler JD. A tumor of follicular infundibulum. report of a case. Arch Dermatol. 1961;83:924-927.
2. Abbas O, Mahalingam M. Tumor of the follicular infundibulum: an epidermal reaction pattern? Am J Dermatopathol. 2009;31:626633.
3. Cribier B, Grosshans E. Tumor of the follicular infundibulum: a clinicopathologic study. J Am Acad Dermatol. 1995;33:979-984.
4. Sartorelli AC, Leite FE, Friedman IV, et al. Vitiligoid hypopigmented macules and tumor of the follicular infundibulum [in Portuguese]. An Bras Dermatol. 2009;84:68-70.
5. Schnitzler L, Civatte J, Robin F, et al. Multiple tumors of the follicular infundibulum with basocellular degeneration. apropos of a case [in French]. Ann Dermatol Venereol. 1987;114:551-556.
6. Starink TM, Meijer CJ, Brownstein MH. The cutaneous pathology of Cowden’s disease: new findings. J Cutan Pathol. 1985;12:83-93.
7. Weyers W, Hörster S, Diaz-Cascajo C. Tumor of follicular infundibulum is basal cell carcinoma. Am J Dermatopathol. 2009;31:634-641.
Tumor of the follicular infundibulum (TFI) was first described by Mehregan and Butler1 in a patient with multiple papules. It typically presents as a solitary lesion that mainly affects the face, neck, and upper trunk, and it generally occurs in elderly patients with a female predilection and occasional vulvar involvement. Sometimes TFI may coexist with an unusual trichilemmal tumor or basal cell carcinoma (BCC) with sebaceous or sweat duct differentiation. Other features of TFI include an eosinophilic cuticle, ductal differentiation, coronoid lamellae, and desmoplasia. Interestingly, approximately one-fourth of reported TFIs were found to be associated with other cutaneous lesions, including BCC, actinic keratosis, desmoplastic malignant melanoma, junctional melanocytic nevus, trichilemmoma, and epidermal inclusion cyst.2 Eruptive forms of TFI are rare, presenting as macules, smooth or slightly keratotic papules, or depressed lesions with a flesh-colored erythematous or hypopigmented appearance. We report the case of a 49-year-old woman with multiple TFIs and some new features.
Case Report
A 49-year-old woman presented with multiple lesions on the arms, shoulders, trunk, buttocks, and legs of more than 3 years’ duration. According to the patient, multiple small, reddish papules gradually appeared on the arms and legs approximately 3 years prior to presentation and were accompanied by considerable pruritus. She sought medical assistance several times at local clinics. A diagnosis of eczema and prurigo was made and oral antihistamines and topical glucocorticoids were administered for more than 2 years. The pruritus was controlled to some degree but recurred after discontinuation of treatment. Five months later, the lesions flared up suddenly and rapidly to the back and buttocks, just around the skin areas treated with cupping glass, a traditional Chinese therapy, for heat syncope. She reported constant itching that kept her awake at night.
Physical examination revealed hundreds of erythematous maculopapules scattered over the arms, shoulders, trunk, buttocks, and legs. The individual lesions were minimally elevated, irregularly shaped, and slightly scaly, and they were distributed in a relatively symmetrical manner. Some of the lesions coalesced to form small plaques measuring approximately 0.5 to 3 cm in diameter (Figure 1). Interestingly, several annulated lesions with a hypopigmented center and hyperpigmented periphery could be observed at areas treated with cupping glass, showing a typical presentation of the Köbner phenomenon (Figure 2). No obvious association with sun exposure or hair loss was detected. The patient’s medical history was unremarkable and there was no known family history of similar skin lesions.
|
The differential diagnosis included lichen planus, prurigo, and adnexal tumors. Histopathologic examination of biopsies from lesions on the back and around the cupping glass areas revealed a benign platelike proliferation of pale-staining epithelial cells in the papillary dermis connected to the overlying epidermis with a moderate lymphatic cell infiltration (Figure 3A). Weigert staining revealed a network of elastic fibers surrounding the base of the tumor (Figure 3B). The pale epithelial cells were positive on periodic acid–Schiff staining (Figure 3C). Immunohistochemical staining revealed that the proliferation was positive for keratin 17 (Figure 3D).
These striking clinical and histological findings suggested the lesions were multiple TFIs. Treatment with tretinoin ointment 0.1% twice daily for 2 months was ineffective. The patient refused treatment with either oral acitretin or dapsone or invasive techniques such as lasers and cryotherapy. She has been on careful follow-up for the last 2 years with new lesions appearing intermittently.
Comment
The etiology of TFI still is unknown but may be related to environmental factors or genetic changes. Tumors of the follicular infundibulum generally are classified as solitary, eruptive, associated with other lesions of Cowden disease, associated with a single tumor, or TFI-like epidermal changes.3 The eruptive form has seldom been reported to date. Eruptive TFIs are nonspecific, ranging in number from several to more than 100. Clinical characteristics and distribution of the lesions can vary from patient to patient, but the lesions tend to be quite monomorphous, even in cases with more than 100 lesions.4 Histopathologic features usually are typical and distinctive, allowing its definite diagnosis. To confirm the diagnosis, the immunohistochemical profile may be useful to characterize its follicular origin, which is positive for keratin 17. Tumors of the follicular infundibulum usually are benign; however, in one patient with more than 100 lesions, there was documented transformation into BCC.5 Due to the potential for malignant transformation as well as its occurrence within the spectrum of lesions associated with Cowden disease,6,7 long-term supervision of TFI is strongly recommended, as was the case with our patient.
A remarkable feature in our case was the patient’s severe pruritus, as most reported cases have been asymptomatic. The increased association with other cutaneous lesions,2 the Köbner phenomenon, and the underlying inflammatory cell infiltration of the tumors in our case strongly suggested that eruptive TFI may represent a kind of cutaneous reaction.
|
Conclusion
The clinical findings of severe pruritus and the Köbner phenomenon in our patient further expand the constellation of the clinical presentation of the eruptive variant of TFI.
Tumor of the follicular infundibulum (TFI) was first described by Mehregan and Butler1 in a patient with multiple papules. It typically presents as a solitary lesion that mainly affects the face, neck, and upper trunk, and it generally occurs in elderly patients with a female predilection and occasional vulvar involvement. Sometimes TFI may coexist with an unusual trichilemmal tumor or basal cell carcinoma (BCC) with sebaceous or sweat duct differentiation. Other features of TFI include an eosinophilic cuticle, ductal differentiation, coronoid lamellae, and desmoplasia. Interestingly, approximately one-fourth of reported TFIs were found to be associated with other cutaneous lesions, including BCC, actinic keratosis, desmoplastic malignant melanoma, junctional melanocytic nevus, trichilemmoma, and epidermal inclusion cyst.2 Eruptive forms of TFI are rare, presenting as macules, smooth or slightly keratotic papules, or depressed lesions with a flesh-colored erythematous or hypopigmented appearance. We report the case of a 49-year-old woman with multiple TFIs and some new features.
Case Report
A 49-year-old woman presented with multiple lesions on the arms, shoulders, trunk, buttocks, and legs of more than 3 years’ duration. According to the patient, multiple small, reddish papules gradually appeared on the arms and legs approximately 3 years prior to presentation and were accompanied by considerable pruritus. She sought medical assistance several times at local clinics. A diagnosis of eczema and prurigo was made and oral antihistamines and topical glucocorticoids were administered for more than 2 years. The pruritus was controlled to some degree but recurred after discontinuation of treatment. Five months later, the lesions flared up suddenly and rapidly to the back and buttocks, just around the skin areas treated with cupping glass, a traditional Chinese therapy, for heat syncope. She reported constant itching that kept her awake at night.
Physical examination revealed hundreds of erythematous maculopapules scattered over the arms, shoulders, trunk, buttocks, and legs. The individual lesions were minimally elevated, irregularly shaped, and slightly scaly, and they were distributed in a relatively symmetrical manner. Some of the lesions coalesced to form small plaques measuring approximately 0.5 to 3 cm in diameter (Figure 1). Interestingly, several annulated lesions with a hypopigmented center and hyperpigmented periphery could be observed at areas treated with cupping glass, showing a typical presentation of the Köbner phenomenon (Figure 2). No obvious association with sun exposure or hair loss was detected. The patient’s medical history was unremarkable and there was no known family history of similar skin lesions.
|
The differential diagnosis included lichen planus, prurigo, and adnexal tumors. Histopathologic examination of biopsies from lesions on the back and around the cupping glass areas revealed a benign platelike proliferation of pale-staining epithelial cells in the papillary dermis connected to the overlying epidermis with a moderate lymphatic cell infiltration (Figure 3A). Weigert staining revealed a network of elastic fibers surrounding the base of the tumor (Figure 3B). The pale epithelial cells were positive on periodic acid–Schiff staining (Figure 3C). Immunohistochemical staining revealed that the proliferation was positive for keratin 17 (Figure 3D).
These striking clinical and histological findings suggested the lesions were multiple TFIs. Treatment with tretinoin ointment 0.1% twice daily for 2 months was ineffective. The patient refused treatment with either oral acitretin or dapsone or invasive techniques such as lasers and cryotherapy. She has been on careful follow-up for the last 2 years with new lesions appearing intermittently.
Comment
The etiology of TFI still is unknown but may be related to environmental factors or genetic changes. Tumors of the follicular infundibulum generally are classified as solitary, eruptive, associated with other lesions of Cowden disease, associated with a single tumor, or TFI-like epidermal changes.3 The eruptive form has seldom been reported to date. Eruptive TFIs are nonspecific, ranging in number from several to more than 100. Clinical characteristics and distribution of the lesions can vary from patient to patient, but the lesions tend to be quite monomorphous, even in cases with more than 100 lesions.4 Histopathologic features usually are typical and distinctive, allowing its definite diagnosis. To confirm the diagnosis, the immunohistochemical profile may be useful to characterize its follicular origin, which is positive for keratin 17. Tumors of the follicular infundibulum usually are benign; however, in one patient with more than 100 lesions, there was documented transformation into BCC.5 Due to the potential for malignant transformation as well as its occurrence within the spectrum of lesions associated with Cowden disease,6,7 long-term supervision of TFI is strongly recommended, as was the case with our patient.
A remarkable feature in our case was the patient’s severe pruritus, as most reported cases have been asymptomatic. The increased association with other cutaneous lesions,2 the Köbner phenomenon, and the underlying inflammatory cell infiltration of the tumors in our case strongly suggested that eruptive TFI may represent a kind of cutaneous reaction.
|
Conclusion
The clinical findings of severe pruritus and the Köbner phenomenon in our patient further expand the constellation of the clinical presentation of the eruptive variant of TFI.
1. Mehregan AH, Butler JD. A tumor of follicular infundibulum. report of a case. Arch Dermatol. 1961;83:924-927.
2. Abbas O, Mahalingam M. Tumor of the follicular infundibulum: an epidermal reaction pattern? Am J Dermatopathol. 2009;31:626633.
3. Cribier B, Grosshans E. Tumor of the follicular infundibulum: a clinicopathologic study. J Am Acad Dermatol. 1995;33:979-984.
4. Sartorelli AC, Leite FE, Friedman IV, et al. Vitiligoid hypopigmented macules and tumor of the follicular infundibulum [in Portuguese]. An Bras Dermatol. 2009;84:68-70.
5. Schnitzler L, Civatte J, Robin F, et al. Multiple tumors of the follicular infundibulum with basocellular degeneration. apropos of a case [in French]. Ann Dermatol Venereol. 1987;114:551-556.
6. Starink TM, Meijer CJ, Brownstein MH. The cutaneous pathology of Cowden’s disease: new findings. J Cutan Pathol. 1985;12:83-93.
7. Weyers W, Hörster S, Diaz-Cascajo C. Tumor of follicular infundibulum is basal cell carcinoma. Am J Dermatopathol. 2009;31:634-641.
1. Mehregan AH, Butler JD. A tumor of follicular infundibulum. report of a case. Arch Dermatol. 1961;83:924-927.
2. Abbas O, Mahalingam M. Tumor of the follicular infundibulum: an epidermal reaction pattern? Am J Dermatopathol. 2009;31:626633.
3. Cribier B, Grosshans E. Tumor of the follicular infundibulum: a clinicopathologic study. J Am Acad Dermatol. 1995;33:979-984.
4. Sartorelli AC, Leite FE, Friedman IV, et al. Vitiligoid hypopigmented macules and tumor of the follicular infundibulum [in Portuguese]. An Bras Dermatol. 2009;84:68-70.
5. Schnitzler L, Civatte J, Robin F, et al. Multiple tumors of the follicular infundibulum with basocellular degeneration. apropos of a case [in French]. Ann Dermatol Venereol. 1987;114:551-556.
6. Starink TM, Meijer CJ, Brownstein MH. The cutaneous pathology of Cowden’s disease: new findings. J Cutan Pathol. 1985;12:83-93.
7. Weyers W, Hörster S, Diaz-Cascajo C. Tumor of follicular infundibulum is basal cell carcinoma. Am J Dermatopathol. 2009;31:634-641.
Practice Points
- Multiple tumors of the follicular infundibulum (TFIs) sometimes may have the potential for malignant transformation; therefore, long-term supervision of TFI is strongly recommended.
- Eruptive forms of TFI are rare. In our patient, severe pruritus, the Köbner phenomenon, and the underlying inflammatory cell infiltration of the tumors strongly suggested that eruptive TFI may represent a kind of cutaneous reaction.