User login
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
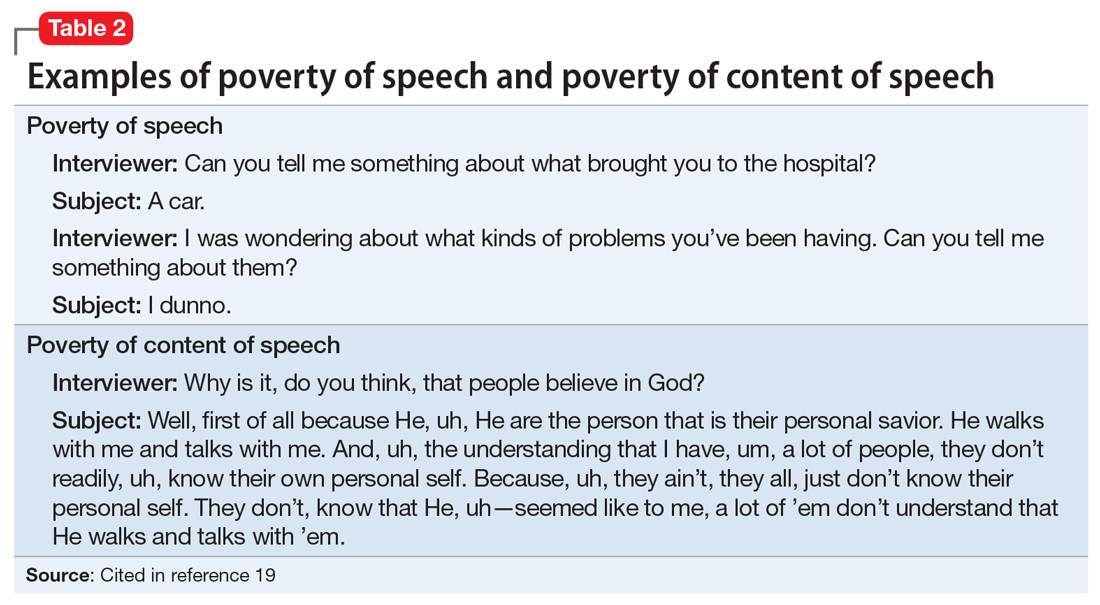
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
Secondary negative symptoms
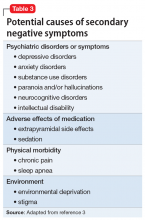
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
Secondary negative symptoms
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
The negative symptoms of schizophrenia have been recognized for 100 years. Characterized by a loss of a function that should be present, negative symptoms include anhedonia, asociality, amotivation, and affective blunting. Individuals with schizophrenia who have a preponderance of negative symptoms (“deficit syndrome”) may comprise a special subset of patients. Compared with positive symptoms, negative symptoms are associated with worse global functioning and worse response to antipsychotic medication. Treatment of negative symptoms is challenging. Secondary negative symptoms—those that simulate or resemble primary negative symptoms but are attributable to another cause, such as major depressive disorder or the adverse effects of antipsychotic medication—need to be ruled out. Emerging evidence suggests that newer antipsychotics with novel mechanisms might be effective in treating negative symptoms. Antidepressants might also play a role.
This article describes types of negative symptoms, their clinical relevance, neuroanatomical and neurotransmission factors associated with negative symptoms, and current and future treatment options.
Modest improvements with antipsychotics
Schizophrenia affects an estimated 1% of the population.1 Antipsychotic medication has been the mainstay of schizophrenia treatment since
All antipsychotics are believed to exert their therapeutic effects by blocking dopamine (D2) receptors and are effective in ameliorating the positive symptoms of schizophrenia, including hallucinations, delusions, bizarre behavior, disordered thinking, and agitation.1 Early research had suggested that SGAs might also reduce the negative symptoms of schizophrenia, perhaps because they also block serotonin 2A receptors, a property thought to broaden their therapeutic profile. Over time, it became clear that neither FGAs nor SGAs conferred an advantage in treating negative symptoms, and that the observed improvements were modest.2-5 However, recent research suggests that several newer antipsychotics might be effective in targeting negative symptoms.2,6,7
History of negative symptoms
In the early 20th century, Swiss psychiatrist Eugen Bleuler coined the term schizophrenia to emphasize the cognitive impairment that occurs in patients with this illness, and which he conceptualized as a fragmenting of the psychic process.8 He believed that certain symptoms were fundamental to the illness, and described affective blunting, disturbance of association (ie, distorted thinking) autism (ie, impaired relationships), and ambivalence (ie, fragmented emotional responses). He viewed hallucinations and delusions as accessory symptoms because they were not unique to schizophrenia but were also found in other disorders (eg, mood disorders). Bleuler’s ideas took root, and generations of psychiatrists were taught his fundamental symptoms (“the 4 A’s”), the forerunner of today’s negative symptoms. Later, other experts chose to emphasize psychotic symptoms as most characteristic of schizophrenia, including Schneider’s “first-rank symptoms,” such as voices conversing or delusions of passivity.9
Negative symptoms were rediscovered in the 1970s and 1980s by psychiatric researchers interested in descriptive phenomenology.10,11 Research confirmed the presence of a positive dimension in schizophrenia characterized by the loss of boundaries between the patient and the real world (eg, hallucinations, delusions), and a negative dimension characterized by the loss of a function that should be present, such as alogia and asociality. These experts carefully described negative symptoms and created scales to measure them, including the Scale for the Assessment of Negative Symptoms (SANS),12 the Positive and Negative Syndrome Scale (PANSS),13 the Brief Negative Symptom Scale (BNSS),14 and the 16-item Negative Symptom Assessment (NSA-16).15 Contemporaneous to this work, a “deficit syndrome” was identified among patients with schizophrenia with prominent negative symptoms. The deficit syndrome is found in 25% to 30% of chronic cases.16 Negative symptoms are very common in patients with schizophrenia (Table 19).8,17
Early editions of the DSM defined schizophrenia mainly on the basis of disturbance of cognition, mood, and behavior, and a retreat from reality. With the publication of DSM-III in 1980, and in subsequent editions, schizophrenia was redefined as a relatively severe psychotic illness in which positive and negative symptoms were present, thereby acknowledging the importance of Bleuler’s fundamental symptoms. In DSM-5, negative symptoms are described as accounting for “a substantial portion of the morbidity associated with schizophrenia but are less prominent in other psychotic disorders.”18
Continue to: Types of negative symptoms
Types of negative symptoms
The following symptoms fall within the negative dimension19:
Alogia refers to the impoverished thinking and cognition that often occur in patients with schizophrenia. The patient’s thinking processes seem empty, turgid, or slow, as inferred from the patient’s speech. The 2 major manifestations of alogia are poverty of speech (nonfluent empty speech) and poverty of content of speech (fluent but empty speech). Examples of each appear in Table 2.19
Affective flattening or blunting manifests as a general impoverishment of emotional expression, reactivity, and feeling. Affective flattening can be assessed through observing a patient’s behavior and responsiveness during the interview.
Avolition-apathy manifests itself as a lack of energy and drive. Patients become inert and are unable to mobilize themselves to initiate or persist in completing many kinds of tasks.
Anhedonia-asociality encompasses the patient’s difficulties in experiencing interest or pleasure. It may express itself as a loss of interest in pleasurable activities, an inability to experience pleasure when participating in activities normally considered pleasurable, or a lack of involvement in social relationships.
Continue to: Attention
Attention is often poor in patients with severe mental illnesses. The patient may have trouble focusing his/her attention or may be able to focus only sporadically and erratically. He/she may ignore attempts to converse with him/her, wander away during an activity or a task, or appear to be inattentive when engaged in formal testing or interviewing.
Clinical relevance of negative symptoms
According to DSM-5, “Negative symptoms are more closely related to prognosis than are positive symptoms and tend to be the most persistent.”18 Research has shown that, compared with positive symptoms, negative symptoms are associated with greater impairment in overall functioning, social interaction, interpersonal relationships, economic functioning, and recreational activities.1,3,5 Negative symptoms also are associated with poorer response to medication and a positive family history of schizophrenia. Research shows that negative symptoms are persistent over time, and, in fact, become more prominent as the patient ages, whereas positive symptoms become less prominent.20
Secondary negative symptoms
Potential secondary causes of negative symptoms should be ruled out before concluding that the negative symptoms are due to schizophrenia.3 What might appear to be a negative symptom of schizophrenia, such as poor motivation or flattened affect, could be due to the presence of major depressive disorder. Such symptoms might resolve with treatment. Alternatively, a patient could have developed pseudoparkinsonism from antipsychotic medication and display unchanging facial expression and decreased spontaneous movements. These symptoms could resolve by adding
The neuroanatomy of negative symptoms
Although the neuroanatomical basis of negative symptoms has not been determined, neuroimaging studies have provided important clues.3 Structural brain imaging has consistently shown that negative symptoms in patients with schizophrenia correlate with decreased prefrontal white matter volume, anterior cingulate volume, insular cortex volume, left temporal cortex volume, and ventricular enlargement. Interestingly, volume loss starts before the appearance of negative symptoms.21,22 Functional imaging has shown that negative symptoms correlate with reduced cerebral blood perfusion in frontal, prefrontal, posterior cingulate, thalamus, parietal, and striatal regions.21,22 These findings may help explain the apathy, failure to initiate activities, and impaired social relatedness in patients with schizophrenia.
Neurotransmission and negative symptoms
Some experts have hypothesized that lowered cortical dopamine transmission in mesocortical pathways could give rise to negative symptoms, whereas excess transmission in subcortical structures leads to positive symptoms.23 There is also evidence for a noradrenalin deficiency based on the finding that low levels of cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol (MHPG), a noradrenaline metabolite, correlates with greater negative symptom severity.24 The presence of a serotonin deficiency has been proposed based on evidence that negative symptoms might be mitigated by serotonergic agents.25 More recently, some experts have posited that the dopamine D3 receptor might be involved in the etiology of negative symptoms. The dopamine D3 receptor activity is expressed in brain regions thought to control reward, emotions, and motivation.2 Newer medications with novel mechanisms suggest that other neurotransmitter pathways could be involved.6,7
Continue to: Treatment options
Treatment options
Treating negative symptoms remains challenging and there are no clear answers. When they were introduced in the 1990s, SGAs were initially thought to be superior to FGAs in targeting negative symptoms. Subsequent research, including recent reviews and meta-analyses, has shown that SGAs are not superior to FGAs in treating negative symptoms, and the effect of either medication class on negative symptoms is modest.2-5 One exception is amisulpride (not available in the United States), which is known to antagonize D2 and D3 receptors. A meta-analysis of the efficacy of antipsychotics in schizophrenia showed that amisulpride was significantly more effective than placebo in treating negative symptoms in 590 patients who received the medication.26 The authors suggested that amisulpride was effective due to its binding to presynaptic receptors in the frontal cortex, thereby enhancing dopamine transmission in this region.
Cariprazine, which acts as a partial agonist at the D2 and D3 receptors, with a 10-fold affinity for the D3 receptor, also has shown promise in treating negative symptoms.2 In a clinical trial of 460 patients with predominant negative symptoms, treatment with cariprazine led to a greater reduction in negative symptoms than
Other promising agentsinclude
Antidepressants also could be effective in reducing negative symptoms.3 A meta-analysis of randomized controlled trials evaluating the use of antidepressants as adjuncts to antipsychotic medications showed that adding an antidepressant was effective in reducing negative symptoms.29 The mechanism by which an antidepressant might cause a reduction in negative symptoms is uncertain, and it is possible that the antidepressant might treat depressive symptoms that are causing or contributing to the negative symptoms.
Bottom Line
Negative symptoms in patients with schizophrenia are associated with a worse functional outcome and poorer response to antipsychotic medication than positive symptoms. First- and second-generation antipsychotics are largely ineffective in consistently treating negative symptoms. Antipsychotic medications that target the D3 receptor might be more effective. Roluperidone, which targets serotonin 2A and sigma receptors, and SEP-363856, which targets TAAR1 and serotonin 1A receptors, are being studied for their effects on negative symptoms.
Continue to: Related Resources
Related Resources
- Galderisi S, Färden A, Kaiser S. Dissecting negative symptoms of schizophrenia: History, assessment, pathophysiological mechanisms and treatment. Schizophr Res. 2017;186:1-2.
- Rabinowitz J. Treating negative symptoms of schizophrenia. Current Psychiatry. 2018;17(12):19-23.
Drug Brand Names
Benztropine • Cogentin
Cariprazine • Vraylar
Chlorpromazine • Promapar, Thorazine
Risperidone • Risperdal
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.
1. Owen MJ, Sawa A, Mortensen PD. Schizophrenia. Lancet. 2016;388(10039):86-97.
2. Cerviri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525-1535.
3. Mitra S, Mahintamani T, Kavoor AR, et al. Negative symptoms in schizophrenia. Ind Psychiatr J. 2016;25(2):135-144.
4. Fusa-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892-899.
5. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms: an update. Curr Treat Options Psych. 2016;3:133-150.
6. Harvey PD, Saoud JB, Luthringer R, et al. Effects of roluperidone (MIN-101) on two dimensions of negative symptoms factor score: reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352-356.
7. Dedic N, Jones PG, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Psychopharmacol Exp Ther. 2019;371(1):1-14.
8. Bleuler E. Dementia praecox or the group of schizophrenia. New York, New York: International Universities Press; 1950.
9. Andreasen NC. The diagnosis of schizophrenia. Schizophr Bull. 1987;13(1):9-22.
10. Andreasen NC. Thought, language, and communication disorders I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36(12):1315-1321.
11. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280(6207):66-68.
12. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789-794.
13. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
14. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305.
15. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item Negative Symptoms Assessment. J Psychiatr Res. 1993;27(3):253-258.
16. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578-583.
17. Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS Study. J Clin Psychiatry. 2010;71(3):280-286.
18. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
19. Black DW, Andreasen NC. Interviewing and assessment. In: Introductory textbook of psychiatry, 7th ed. Black DW, Andreasen NC, eds. Washington, DC: American Psychiatric Publishing; 2020:15-53.
20. Pfohl B, Winokur G. The micropsychopathology of hebephrenic/catatonic schizophrenia. J Nerv Ment Dis. 1983;171(5):296-300.
21. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12(1):53-69.
22. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, et al. A review of schizophrenia, melancholic depression and Parkinson’s disease. Brain Res Bull. 2006;70(4-6):312-321.
23. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: making sense of it all. Curr Psychiatry Rep. 2007;9(4):329-336.
24. Yoshimura R, Hori H, Katsuki A, et al. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF, and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia. Ann Gen Psychiatry. 2016;15:1.
25. Moller HJ. Management of negative symptoms of schizophrenia: new treatment options. CNS Drugs. 2003;17(11):793-823.
26. Leucht S. Amisulpride: a selective dopamine antagonist and atypical antipsychotic: results of a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2004;7(suppl 1):S15-S20. doi: 10.1017/S1461145704004109.
27. Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomized, double-blind, controlled trial. Lancet. 2017;389(10074):1103-1113.
28. Neill JC, Grayson, Kiss B, et al. Effects of cariprazine, a novel antipsychotic, on cognitive deficit and negative symptoms in a rodent model of schizophrenia symptomatology. Eur Neuropsychopharmacol. 2016;26(1):3-14.
29. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9):876-886.