User login
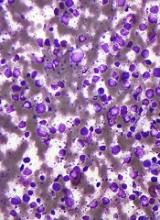
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()