User login
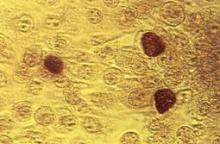
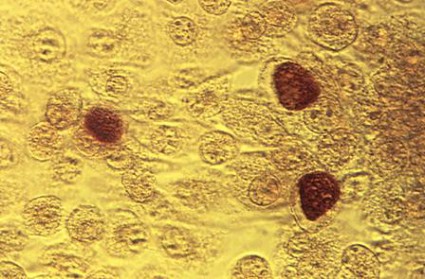
PRAGUE – Recent evidence dictates the need to reassess the roles of doxycycline and azithromycin in treating Chlamydia trachomatis nongonococcal urethritis, according to Dr. Michel Janier.
Current first-line therapy for nongonococcal urethritis (NGU), as recommended by the Centers for Disease Control and Prevention and other major groups, features a choice: a single 1-g dose of azithromycin, or doxycycline at 100 mg b.i.d. for 7 days. Single-dose azithromycin is a popular option, given its convenience and likely better adherence.
But a couple of important head-to-head comparative trials published recently are making waves in the infectious disease world. Doxycycline proved significantly more effective than azithromycin in clearing chlamydial NGU in one study and had a markedly lower C. trachomatis persistence rate 45 days post treatment in the other, said Dr. Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections–Europe.
One study was a phase IIb randomized, double-blind trial involving 305 men with NGU at sexually transmitted disease clinics in four U.S. cities. They were assigned to guideline-recommended treatment with either azithromycin or doxycycline alone or with a single 2-g dose of tinidazole, an antitrichomonal agent, in order to test the hypothesis that adding the second agent would boost cure rates. As it turned out, it did not.
Among the 43% of men with C. trachomatis NGU, the chlamydial clearance rate was 94.8% in the doxycycline arm compared with 77.4% with azithromycin.
While doxycycline outperformed azithromycin in men with C. trachomatis NGU, the converse was true among the 31% of participants with Mycoplasma genitalium NGU. The clearance rate was 30.8% in the doxycycline arm compared with 66.7% in the azithromycin arm (Clin. Infect. Dis. 2011;52:163-70).
The same group of investigators recently analyzed data on post-treatment persistence of NGU in a study involving 293 heterosexual men treated for NGU at STD clinics. Among the 129 men with C. trachomatis NGU, persistent C. trachomatis infection was detected via nucleic acid amplification testing 4 weeks post treatment in 23% of those who received azithromycin compared with just 5% treated with doxycycline (J. Infect. Dis. 2012;206:357-65).
The explanation for the observed higher failure rate with azithromycin compared with doxycycline in treating chlamydial NGU is probably twofold: homotypic resistance of the organism to a single dose of a bacteriostatic antibiotic, coupled with heterotopic resistance stemming from a persistent subpopulation of cells having a reduced growth rate within the larger pathogen load, Dr. Janier said.
He added that while it’s important not to overreact to a couple of studies carried out by a single group, there is intense interest on the part of many infectious disease experts in taking a closer look at the possibility that azithromycin may need to be dethroned as first-line therapy.
The dermatologist also highlighted another recent study that bears on the treatment of uncomplicated C. trachomatis NGU. The double-blind, randomized, double-dummy multicenter trial included 323 men and nonpregnant women with urogenital chlamydia. They were randomized to 7 days of once-daily delayed-release doxycycline (Doryx) at 200 mg or to 100 mg b.i.d. of standard-release doxycycline (Vibramycin).
The primary outcome, microbial cure by nucleic acid amplification testing on day 28, occurred in 95.5% of the delayed-release doxycycline group and a virtually identical 95.2% on Vibramycin. However, the delayed-release formulation was significantly better tolerated, with a 13% nausea rate compared with 21% in the Vibramycin group. Vomiting occurred in 8% of patients on delayed-release doxycycline, a significantly lower rate than the 12% with Vibramycin.
The investigators concluded that delayed-release doxycycline, with its once-daily dosing and better tolerability, could improve treatment adherence (Clin. Infect. Dis. 2012; 55: 82-8).
Dr. Janier reported having no relevant financial disclosures.
PRAGUE – Recent evidence dictates the need to reassess the roles of doxycycline and azithromycin in treating Chlamydia trachomatis nongonococcal urethritis, according to Dr. Michel Janier.
Current first-line therapy for nongonococcal urethritis (NGU), as recommended by the Centers for Disease Control and Prevention and other major groups, features a choice: a single 1-g dose of azithromycin, or doxycycline at 100 mg b.i.d. for 7 days. Single-dose azithromycin is a popular option, given its convenience and likely better adherence.
But a couple of important head-to-head comparative trials published recently are making waves in the infectious disease world. Doxycycline proved significantly more effective than azithromycin in clearing chlamydial NGU in one study and had a markedly lower C. trachomatis persistence rate 45 days post treatment in the other, said Dr. Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections–Europe.
One study was a phase IIb randomized, double-blind trial involving 305 men with NGU at sexually transmitted disease clinics in four U.S. cities. They were assigned to guideline-recommended treatment with either azithromycin or doxycycline alone or with a single 2-g dose of tinidazole, an antitrichomonal agent, in order to test the hypothesis that adding the second agent would boost cure rates. As it turned out, it did not.
Among the 43% of men with C. trachomatis NGU, the chlamydial clearance rate was 94.8% in the doxycycline arm compared with 77.4% with azithromycin.
While doxycycline outperformed azithromycin in men with C. trachomatis NGU, the converse was true among the 31% of participants with Mycoplasma genitalium NGU. The clearance rate was 30.8% in the doxycycline arm compared with 66.7% in the azithromycin arm (Clin. Infect. Dis. 2011;52:163-70).
The same group of investigators recently analyzed data on post-treatment persistence of NGU in a study involving 293 heterosexual men treated for NGU at STD clinics. Among the 129 men with C. trachomatis NGU, persistent C. trachomatis infection was detected via nucleic acid amplification testing 4 weeks post treatment in 23% of those who received azithromycin compared with just 5% treated with doxycycline (J. Infect. Dis. 2012;206:357-65).
The explanation for the observed higher failure rate with azithromycin compared with doxycycline in treating chlamydial NGU is probably twofold: homotypic resistance of the organism to a single dose of a bacteriostatic antibiotic, coupled with heterotopic resistance stemming from a persistent subpopulation of cells having a reduced growth rate within the larger pathogen load, Dr. Janier said.
He added that while it’s important not to overreact to a couple of studies carried out by a single group, there is intense interest on the part of many infectious disease experts in taking a closer look at the possibility that azithromycin may need to be dethroned as first-line therapy.
The dermatologist also highlighted another recent study that bears on the treatment of uncomplicated C. trachomatis NGU. The double-blind, randomized, double-dummy multicenter trial included 323 men and nonpregnant women with urogenital chlamydia. They were randomized to 7 days of once-daily delayed-release doxycycline (Doryx) at 200 mg or to 100 mg b.i.d. of standard-release doxycycline (Vibramycin).
The primary outcome, microbial cure by nucleic acid amplification testing on day 28, occurred in 95.5% of the delayed-release doxycycline group and a virtually identical 95.2% on Vibramycin. However, the delayed-release formulation was significantly better tolerated, with a 13% nausea rate compared with 21% in the Vibramycin group. Vomiting occurred in 8% of patients on delayed-release doxycycline, a significantly lower rate than the 12% with Vibramycin.
The investigators concluded that delayed-release doxycycline, with its once-daily dosing and better tolerability, could improve treatment adherence (Clin. Infect. Dis. 2012; 55: 82-8).
Dr. Janier reported having no relevant financial disclosures.
PRAGUE – Recent evidence dictates the need to reassess the roles of doxycycline and azithromycin in treating Chlamydia trachomatis nongonococcal urethritis, according to Dr. Michel Janier.
Current first-line therapy for nongonococcal urethritis (NGU), as recommended by the Centers for Disease Control and Prevention and other major groups, features a choice: a single 1-g dose of azithromycin, or doxycycline at 100 mg b.i.d. for 7 days. Single-dose azithromycin is a popular option, given its convenience and likely better adherence.
But a couple of important head-to-head comparative trials published recently are making waves in the infectious disease world. Doxycycline proved significantly more effective than azithromycin in clearing chlamydial NGU in one study and had a markedly lower C. trachomatis persistence rate 45 days post treatment in the other, said Dr. Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections–Europe.
One study was a phase IIb randomized, double-blind trial involving 305 men with NGU at sexually transmitted disease clinics in four U.S. cities. They were assigned to guideline-recommended treatment with either azithromycin or doxycycline alone or with a single 2-g dose of tinidazole, an antitrichomonal agent, in order to test the hypothesis that adding the second agent would boost cure rates. As it turned out, it did not.
Among the 43% of men with C. trachomatis NGU, the chlamydial clearance rate was 94.8% in the doxycycline arm compared with 77.4% with azithromycin.
While doxycycline outperformed azithromycin in men with C. trachomatis NGU, the converse was true among the 31% of participants with Mycoplasma genitalium NGU. The clearance rate was 30.8% in the doxycycline arm compared with 66.7% in the azithromycin arm (Clin. Infect. Dis. 2011;52:163-70).
The same group of investigators recently analyzed data on post-treatment persistence of NGU in a study involving 293 heterosexual men treated for NGU at STD clinics. Among the 129 men with C. trachomatis NGU, persistent C. trachomatis infection was detected via nucleic acid amplification testing 4 weeks post treatment in 23% of those who received azithromycin compared with just 5% treated with doxycycline (J. Infect. Dis. 2012;206:357-65).
The explanation for the observed higher failure rate with azithromycin compared with doxycycline in treating chlamydial NGU is probably twofold: homotypic resistance of the organism to a single dose of a bacteriostatic antibiotic, coupled with heterotopic resistance stemming from a persistent subpopulation of cells having a reduced growth rate within the larger pathogen load, Dr. Janier said.
He added that while it’s important not to overreact to a couple of studies carried out by a single group, there is intense interest on the part of many infectious disease experts in taking a closer look at the possibility that azithromycin may need to be dethroned as first-line therapy.
The dermatologist also highlighted another recent study that bears on the treatment of uncomplicated C. trachomatis NGU. The double-blind, randomized, double-dummy multicenter trial included 323 men and nonpregnant women with urogenital chlamydia. They were randomized to 7 days of once-daily delayed-release doxycycline (Doryx) at 200 mg or to 100 mg b.i.d. of standard-release doxycycline (Vibramycin).
The primary outcome, microbial cure by nucleic acid amplification testing on day 28, occurred in 95.5% of the delayed-release doxycycline group and a virtually identical 95.2% on Vibramycin. However, the delayed-release formulation was significantly better tolerated, with a 13% nausea rate compared with 21% in the Vibramycin group. Vomiting occurred in 8% of patients on delayed-release doxycycline, a significantly lower rate than the 12% with Vibramycin.
The investigators concluded that delayed-release doxycycline, with its once-daily dosing and better tolerability, could improve treatment adherence (Clin. Infect. Dis. 2012; 55: 82-8).
Dr. Janier reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY