User login
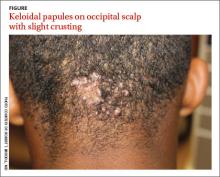
A 15-year-old African American boy with no previous medical problems presented with a 2-month history of hair loss and pruritic papules on the occipital scalp that had developed after a barber shaved the area. Physical examination revealed 2 dozen 1 to 2 mm keloidal papules on the posterior neck and occipital scalp with areas of focal crusting (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acne keloidalis nuchae
Acne keloidalis nuchae is a chronic folliculitis that is characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent, forming firm papules and hairless, keloid-like plaques.1 Seen almost exclusively in young, postpubescent African American males, the condition is often asymptomatic, although some patients complain that the affected area itches. The cause of acne keloidalis nuchae may be associated with an acute pseudofolliculitis secondary to close-shaved curly hair reentering the skin; this leads to a foreign body reaction to hair protein and subsequent fibrosis.2
Differential Dx includes acne vulgaris
Acne keloidalis nuchae is diagnosed based on the appearance and location of the papules and keloid-like plaques as well as the patient’s history. The differential diagnosis includes acne vulgaris, hidradenitis suppurativa, and pseudofolliculitis barbae.
Acne vulgaris is a disorder of the pilosebaceous follicles primarily seen on the face, upper part of the chest, and back. Unlike acne keloidalis, it is characterized by the presence of comedones.1,3
Hidradenitis suppurativa is characterized by secondary inflammation of the apocrine glands, which produces inflamed nodules and abscesses, primarily in the axillae, groin, and anogenital region.1
Pseudofolliculitis barbae looks very similar to the initial presentation of acne keloidalis nuchae, and in fact, the pathophysiologic mechanism is the same. That said, pseudofolliculitis barbae occurs on the beard area and rarely produces keloidal papules.3
Treat with steroids, antibiotics
Treatment of acne keloidalis nuchae is often difficult. Early treatment, however, decreases the potential for developing larger lesions and long-term disfigurement.1
Topical steroid therapy is indicated for mild to moderate acne keloidalis nuchae. Application of tretinoin 0.01% gel once or twice daily for several months has an anti-inflammatory effect and alters keratinocyte differentiation, which may discharge ingrown hairs. Topical and systemic antibiotics minimize infection associated with pseudofolliculitis and have anti-inflammatory effects.1,3 Intralesional steroid injections (triamcinolone acetonide 2.5-5 mg/cc) with 0.1 cc injected into each lesion every 2 to 3 weeks for 3 to 6 injections can reduce inflammation and pruritus and reduce the thickness of keloidal scars.3 (For a how-to video that illustrates intralesional injections, go to http://www.jfponline.com/multimedia/video.html.)
Surgical management is generally reserved for large lesions that do not respond to medical management. Surgical excision with healing by secondary intention has been reported to cause fewer recurrences than surgical excision with primary closure.4 The use of CO2 laser ablation can be considered for advanced cases.5
Teach patients with acne keloidalis nuchae that they can prevent further irritation of the affected area by not wearing head gear that rubs on the involved area. Patients should also refrain from shaving the posterior scalp and neck to prevent the pseudofolliculitis that may be causing this condition.1,3 Electric barber trimmers that leave a short stubble but do not cleanly shave the skin are OK to use.
Our patient’s papules flattened and became asymptomatic over several months of treatment with tretinoin 0.01% gel, doxycycline 100 mg daily, and a series of biweekly intralesion steroid injections. A flat-scarred patch remained.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; rbrodell@umc.edu
1. McMichael A, Sanchez DG, Kelly P. Folliculitis and the follicular occlusion tetrad. In: Bolognia JL, Jorizzo, JL, Rapini RP, et al (eds). Dermatology. 2nd ed. New York, NY: Mosby; 2008: 517-530.
2. Herzberg AJ, Dinehart SM, Kerns BJ, et al. Acne keloidalis. Transverse microscopy, immunohistochemistry, and electron microscopy. Am J Dermatopathol. 1990;12:109-121.
3. Kelly AP. Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin. 2003;21:645-653.
4. Glenn MG, Bennett RG, Kelly AP. Acne keloidalis nuchae: treatment with excision and second-intention healing. J Am Acad Dermatol. 1995;33(2 pt 1):243-246.
5. Kantor GR, Ratz JL, Wheeland RG. Treatment of acne keloidalis nuchae with carbon dioxide laser. J Am Acad Dermatol. 1986;14(2 pt 1):263-267.
A 15-year-old African American boy with no previous medical problems presented with a 2-month history of hair loss and pruritic papules on the occipital scalp that had developed after a barber shaved the area. Physical examination revealed 2 dozen 1 to 2 mm keloidal papules on the posterior neck and occipital scalp with areas of focal crusting (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acne keloidalis nuchae
Acne keloidalis nuchae is a chronic folliculitis that is characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent, forming firm papules and hairless, keloid-like plaques.1 Seen almost exclusively in young, postpubescent African American males, the condition is often asymptomatic, although some patients complain that the affected area itches. The cause of acne keloidalis nuchae may be associated with an acute pseudofolliculitis secondary to close-shaved curly hair reentering the skin; this leads to a foreign body reaction to hair protein and subsequent fibrosis.2
Differential Dx includes acne vulgaris
Acne keloidalis nuchae is diagnosed based on the appearance and location of the papules and keloid-like plaques as well as the patient’s history. The differential diagnosis includes acne vulgaris, hidradenitis suppurativa, and pseudofolliculitis barbae.
Acne vulgaris is a disorder of the pilosebaceous follicles primarily seen on the face, upper part of the chest, and back. Unlike acne keloidalis, it is characterized by the presence of comedones.1,3
Hidradenitis suppurativa is characterized by secondary inflammation of the apocrine glands, which produces inflamed nodules and abscesses, primarily in the axillae, groin, and anogenital region.1
Pseudofolliculitis barbae looks very similar to the initial presentation of acne keloidalis nuchae, and in fact, the pathophysiologic mechanism is the same. That said, pseudofolliculitis barbae occurs on the beard area and rarely produces keloidal papules.3
Treat with steroids, antibiotics
Treatment of acne keloidalis nuchae is often difficult. Early treatment, however, decreases the potential for developing larger lesions and long-term disfigurement.1
Topical steroid therapy is indicated for mild to moderate acne keloidalis nuchae. Application of tretinoin 0.01% gel once or twice daily for several months has an anti-inflammatory effect and alters keratinocyte differentiation, which may discharge ingrown hairs. Topical and systemic antibiotics minimize infection associated with pseudofolliculitis and have anti-inflammatory effects.1,3 Intralesional steroid injections (triamcinolone acetonide 2.5-5 mg/cc) with 0.1 cc injected into each lesion every 2 to 3 weeks for 3 to 6 injections can reduce inflammation and pruritus and reduce the thickness of keloidal scars.3 (For a how-to video that illustrates intralesional injections, go to http://www.jfponline.com/multimedia/video.html.)
Surgical management is generally reserved for large lesions that do not respond to medical management. Surgical excision with healing by secondary intention has been reported to cause fewer recurrences than surgical excision with primary closure.4 The use of CO2 laser ablation can be considered for advanced cases.5
Teach patients with acne keloidalis nuchae that they can prevent further irritation of the affected area by not wearing head gear that rubs on the involved area. Patients should also refrain from shaving the posterior scalp and neck to prevent the pseudofolliculitis that may be causing this condition.1,3 Electric barber trimmers that leave a short stubble but do not cleanly shave the skin are OK to use.
Our patient’s papules flattened and became asymptomatic over several months of treatment with tretinoin 0.01% gel, doxycycline 100 mg daily, and a series of biweekly intralesion steroid injections. A flat-scarred patch remained.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; rbrodell@umc.edu
A 15-year-old African American boy with no previous medical problems presented with a 2-month history of hair loss and pruritic papules on the occipital scalp that had developed after a barber shaved the area. Physical examination revealed 2 dozen 1 to 2 mm keloidal papules on the posterior neck and occipital scalp with areas of focal crusting (FIGURE).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acne keloidalis nuchae
Acne keloidalis nuchae is a chronic folliculitis that is characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent, forming firm papules and hairless, keloid-like plaques.1 Seen almost exclusively in young, postpubescent African American males, the condition is often asymptomatic, although some patients complain that the affected area itches. The cause of acne keloidalis nuchae may be associated with an acute pseudofolliculitis secondary to close-shaved curly hair reentering the skin; this leads to a foreign body reaction to hair protein and subsequent fibrosis.2
Differential Dx includes acne vulgaris
Acne keloidalis nuchae is diagnosed based on the appearance and location of the papules and keloid-like plaques as well as the patient’s history. The differential diagnosis includes acne vulgaris, hidradenitis suppurativa, and pseudofolliculitis barbae.
Acne vulgaris is a disorder of the pilosebaceous follicles primarily seen on the face, upper part of the chest, and back. Unlike acne keloidalis, it is characterized by the presence of comedones.1,3
Hidradenitis suppurativa is characterized by secondary inflammation of the apocrine glands, which produces inflamed nodules and abscesses, primarily in the axillae, groin, and anogenital region.1
Pseudofolliculitis barbae looks very similar to the initial presentation of acne keloidalis nuchae, and in fact, the pathophysiologic mechanism is the same. That said, pseudofolliculitis barbae occurs on the beard area and rarely produces keloidal papules.3
Treat with steroids, antibiotics
Treatment of acne keloidalis nuchae is often difficult. Early treatment, however, decreases the potential for developing larger lesions and long-term disfigurement.1
Topical steroid therapy is indicated for mild to moderate acne keloidalis nuchae. Application of tretinoin 0.01% gel once or twice daily for several months has an anti-inflammatory effect and alters keratinocyte differentiation, which may discharge ingrown hairs. Topical and systemic antibiotics minimize infection associated with pseudofolliculitis and have anti-inflammatory effects.1,3 Intralesional steroid injections (triamcinolone acetonide 2.5-5 mg/cc) with 0.1 cc injected into each lesion every 2 to 3 weeks for 3 to 6 injections can reduce inflammation and pruritus and reduce the thickness of keloidal scars.3 (For a how-to video that illustrates intralesional injections, go to http://www.jfponline.com/multimedia/video.html.)
Surgical management is generally reserved for large lesions that do not respond to medical management. Surgical excision with healing by secondary intention has been reported to cause fewer recurrences than surgical excision with primary closure.4 The use of CO2 laser ablation can be considered for advanced cases.5
Teach patients with acne keloidalis nuchae that they can prevent further irritation of the affected area by not wearing head gear that rubs on the involved area. Patients should also refrain from shaving the posterior scalp and neck to prevent the pseudofolliculitis that may be causing this condition.1,3 Electric barber trimmers that leave a short stubble but do not cleanly shave the skin are OK to use.
Our patient’s papules flattened and became asymptomatic over several months of treatment with tretinoin 0.01% gel, doxycycline 100 mg daily, and a series of biweekly intralesion steroid injections. A flat-scarred patch remained.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; rbrodell@umc.edu
1. McMichael A, Sanchez DG, Kelly P. Folliculitis and the follicular occlusion tetrad. In: Bolognia JL, Jorizzo, JL, Rapini RP, et al (eds). Dermatology. 2nd ed. New York, NY: Mosby; 2008: 517-530.
2. Herzberg AJ, Dinehart SM, Kerns BJ, et al. Acne keloidalis. Transverse microscopy, immunohistochemistry, and electron microscopy. Am J Dermatopathol. 1990;12:109-121.
3. Kelly AP. Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin. 2003;21:645-653.
4. Glenn MG, Bennett RG, Kelly AP. Acne keloidalis nuchae: treatment with excision and second-intention healing. J Am Acad Dermatol. 1995;33(2 pt 1):243-246.
5. Kantor GR, Ratz JL, Wheeland RG. Treatment of acne keloidalis nuchae with carbon dioxide laser. J Am Acad Dermatol. 1986;14(2 pt 1):263-267.
1. McMichael A, Sanchez DG, Kelly P. Folliculitis and the follicular occlusion tetrad. In: Bolognia JL, Jorizzo, JL, Rapini RP, et al (eds). Dermatology. 2nd ed. New York, NY: Mosby; 2008: 517-530.
2. Herzberg AJ, Dinehart SM, Kerns BJ, et al. Acne keloidalis. Transverse microscopy, immunohistochemistry, and electron microscopy. Am J Dermatopathol. 1990;12:109-121.
3. Kelly AP. Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin. 2003;21:645-653.
4. Glenn MG, Bennett RG, Kelly AP. Acne keloidalis nuchae: treatment with excision and second-intention healing. J Am Acad Dermatol. 1995;33(2 pt 1):243-246.
5. Kantor GR, Ratz JL, Wheeland RG. Treatment of acne keloidalis nuchae with carbon dioxide laser. J Am Acad Dermatol. 1986;14(2 pt 1):263-267.