User login
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
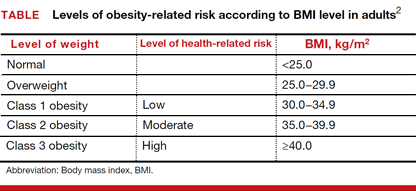
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
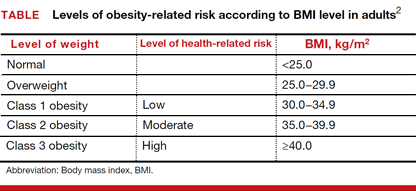
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
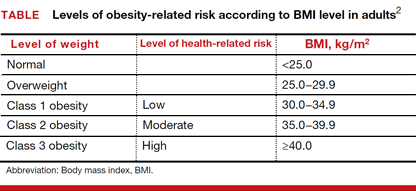
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.