User login
Advanced psychiatric illness and dementia create a wide range of barriers to health care. These patients are unable to provide reliable details with respect to their illness or even discuss basic features of their medical history, forcing providers to rely on contributions from caregiver reports and medical records. Confounding the limits on medical information, physical examinations are often abbreviated or completely refused because of the patient’s distrust, discomfort, or delusion. Over time, the involvement of consulting services may amplify the impact of these barriers as the need for diagnostic and therapeutic interventions emerge. Meanwhile, this delay in definitive management opens a window of risk for deterioration, in which patients cannot be relied on to report important clinical changes.
This case report describes a patient with significant cognitive dysfunction who developed a rare and devastating complication of a hematologic disorder. As the case illustrates, transferring a patient from the psychiatric ward to Internal Medicine (IM) can create unique diagnostic and management challenges.
CASE REPORT
A 64-year-old man developed hematochezia after having been hospitalized in a locked psychiatric ward for the preceding 6 months following a suicide attempt. The episode of hematochezia occurred while on anticoagulation treatment with warfarin for chronic lower extremity deep venous thrombosis (DVT), which prompted the IM consultation. The patient’s past medical history was notable for dementia, hypothyroidism, Crohn disease, and primary sclerosing cholangitis.
The IM Consult Service recommended holding anticoagulation therapy and reversing the coagulopathy with vitamin K. The patient’s stool returned hemoccult and toxin positive for Clostridium difficile (C difficile). The hematochezia was attributed to the infection with C difficile in the setting of anticoagulation. Oral metronidazole was started. Hemoglobin remained stable without further episodes of bleeding. Seven days after the episode of hematochezia, the patient experienced worsening generalized pain and new skin findings. He was transferred to the general medical ward for further management.
The patient’s medical records revealed early cognitive decline with recommendations for supervised residential care as early as age 59 years. An extensive neurocognitive assessment indicated a diagnosis of semantic dementia. He also had a history of recurrent DVT with anticoagulation therapy for > 10 years with no prior workup for a hypercoagulable state. A recent baseline mental status report described a childlike demeanor, profound global speech deficits with marked difficulty understanding even basic medical concepts (eg, the need for a peripheral intravenous catheter), and generalized anxiety disorder complicated by hyperesthesia. The patient frequently refused physical examinations and blood draws as a result. He devoted himself to simple puzzles of kittens and puppies.
Vital signs were normal as were the head and neck, pulmonary, cardiac, and abdominal examinations. The patient’s neurocognitive examination was remarkable for his dependence on instrumental activities of daily living, global aphasia, impaired short- and long-term recall, and poor judgment. He scored 21 out of 30 on a recent mini-mental state examination: failure to achieve 3-word recall; disorientation to month, season, hospital, and county; and an inability to write a sentence or identify a pen. Otherwise, he had fluent speech, facial symmetry, intact strength and sensation throughout, and normal reflexes.
A skin examination revealed diffuse tender subcutaneous lesions. The largest lesion was about 5 cm, located in the left anterolateral thigh. Smaller lesions of about 1 cm were noted in the abdominal wall, right thigh, and bilateral upper extremities. An exquisitely tender, well-demarcated 20-cm elliptical lesion with central necrosis and an erythematous border developed in the left axilla the following day (Figure 1A). Pain limited adduction of the left arm.
The initial laboratory evaluation demonstrated a stable hemoglobin level of 11.1 g/dL, a platelet count of 128 k/mL, and no leukocytosis. Electrolytes and renal indexes were normal. D-dimer and fibrin split products were > 10,000 ng/mL and 20 mg/mL, respectively. Fibrinogen level was 351 mg/dL. The prothrombin time and international normalized ratio were 15.1 seconds and 1.4, respectively. The activated partial thromboplastin time (aPTT) was measured at 40 seconds. High sensitivity C-reactive protein was 4.59. Recent head imaging included a brain magnetic resonance imaging (MRI) notable for enlarged sulci and ventricles with temporal predominance. Positron emission tomography (PET) brain imaging was significant for diffuse hypometabolism in bilateral parietal and temporal lobes with preservation of sensorimotor and occipital cortexes. There was no clear radiographic evidence of cerebral embolic phenomenon or focal cerebrovascular events.
Enoxaparin treatment was initiated for a suspected hypercoagulable state. Ceftriaxone was administered for a urinary tract infection (UTI). Despite premedication, the bedside biopsy of his necrotic skin lesion was aborted due to severe anxiety and generalized somatic pain. A surgical excisional biopsy was thus obtained under general anesthesia. Enoxaparin was held the night before and the morning of surgery. There were no immediate complications related to the biopsy, and malignancy was not seen on intraoperative frozen sections.
Generalized somatic pain persisted the morning after the surgical biopsy, but the patient remained clinically unchanged. An hour later, he was found unresponsive with no pulse. Despite extensive resuscitative efforts, the patient died.
Postmortem
There was a high index of suspicion for a hemostatic perturbation given the skin findings and recent manipulation of anticoagulation with a prior thrombotic event. The axillary lesion closely resembled warfarin-related skin necrosis. Management included enoxaparin with supportive care, pending definitive pathologic findings.
Postmortem examination confirmed diffuse multiorgan involvement similar to the process seen in the thigh biopsy. Ischemic injury secondary to small vessel microthrombi were evident in the skin, subcutaneous fat, large bowel, urinary bladder, and associated pericystic fat (Figure 1B). Interpretation of the surgical thigh biopsy became available after the patient died. It demonstrated infarcted fat with fat necrosis and hemorrhage (Figure 2).
The results of the laboratory investigations for thrombophilia also came back after the patient died. A potent lupus anticoagulant (LA) was demonstrated. It manifested primarily in the intrinsic pathway as a strongly positive LA-sensitive-aPTT (delta time = 20.5 seconds) assay with a weakly positive dilute Russell’s viper venom time assay. The antigenic specificity of the LA antibodies was not uncovered, as the plasma levels of both IgM and IgG anticardiolipin and anti-Β2-glycoprotein-I antibodies were within the reference range. Factor (F) II and FV genotyping revealed wild-type FV, and the prothrombin gene G20210A was without mutation.
Assays for plasma levels of protein S and antithrombin activity were also normal, which excluded deficiencies in these proteins. The assay for protein C activity was slightly decreased. This may have exacerbated the hemostatic imbalance caused by the LA, as the FVII level had normalized. However, the etiology of the protein C deficiency is not clear. Considerations include (1) a warfarin disequilibrium state due to the discontinuation of oral anticoagulation and institution of vitamin K therapy; (2) an epiphenomenon resulting from active thromboses; or (3) a possible hereditary protein C deficiency.
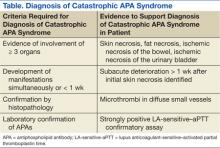
The definitive diagnosis of the catastrophic antiphospholipid antibody (APA) syndrome relies on multiorgan failure in < 1 week, histopathologic evidence of small vessel thrombosis, and a positive LA.1 The study patient fulfilled these criteria (Table).
DISCUSSION
Catastrophic progression of APA syndrome is an infrequent and devastating complication of this autoimmune disorder with a mortality rate of nearly 50%.1 Antiphospholipid antibody syndrome typically presents with thromboses of the larger vessels, and it more commonly affects the venous system. In contrast, diffuse small vessel thromboses underlie the pathogenesis of catastrophic APA syndrome (CAPS).2 This catastrophic progression occurs in < 1 out of 100 patients with the APA syndrome, more frequently in women (69%), and over an age range of 7 decades (mean 38 years).2 A case series analysis identified older age (aged > 36 years), history of systemic lupus erythematous, and broader organ involvement as prognostic indicators of a poor outcome. Better outcomes are associated with thrombocytopenia and anticoagulation treatment. However, gender did not influence mortality.3
Prevention is key to APA management, given the lack of efficacious treatment.2 Preventive measures are focused on avoiding triggers and aggressively treating those triggers that may arise. Possible triggers in this case included cessation of anticoagulation due to hematochezia and in anticipation of surgery, infection (C difficile colitis, suspected necrotic skin wound super infection, and a UTI), and biopsy-related trauma.
Initial clinical stability in this patient with abrupt decompensation along with pending laboratory and pathology results limited the opportunity for more aggressive therapeutic intervention for CAPS. Moreover, the relative sparing of the cardiopulmonary and renal systems contrasted with the more classical systemic involvement usually seen in CAPS. Second-line therapies for CAPS include plasma exchange and high-dose steroids.2 Third-line therapeutics include immunosuppressive agents, such as cyclophosphamide.2
The rapid decompensation, described on postoperative day 1, after a low-risk surgical biopsy highlights the importance of perioperative care in patients with this autoimmune condition. Following a review of surgical cases, Erkan and colleagues concluded that standard antithrombotic regimens for general and orthopedic surgery are likely to undertreat patients with APA syndrome.4 They recommend the following guidelines in place of standard antithrombotic management: preoperative platelet count > 100 k/µL, higher threshold before proceeding with surgery/interventional procedures, limiting intravascular manipulations, and minimizing periods without anticoagulation therapy.4
A case report of a 31-year-old female undergoing mitral valve replacement complicated postoperatively by CAPS-associated biventricular failure, despite preoperative transition of warfarin to unfractionated heparin, illustrates this significant perioperative risk.5 Evidence-based guidelines recommend holding enoxaparin 24 hours before surgery and 24 hours after invasive procedures in patients requiring bridging anticoagulation therapy.6
Treatment of the patient in this case was complicated by his cognitive impairment. Dementia is a less common but well-documented consequence of APA syndrome. A case review of 28 patients with the APA syndrome and dementia suggests an early onset of cognitive decline with a mean age of 49 years. There may be no clear preceding history of stroke in > 50% of patients.7 Interestingly, dementia followed initial manifestations of disease by an average of 3.5 years, even in some patients receiving anticoagulation therapy.7
A nuclear medicine study of 22 patients with APA syndrome and mild neuropsychiatric symptoms demonstrated a 73% incidence of cerebral hypoperfusion (55% diffuse and 18% local) based on PET imaging despite unremarkable MRI findings.8 Extended periods of hypoperfusion secondary to arterial thromboses in the temporal and parietal lobes may have been the primary etiology for dementia in this case. As such, the coexistence of neurologic abnormalities and a hypercoagulability state warrants a thorough diagnostic workup for similar disorders, despite the higher prevalence of dementia in advanced age.
Unfortunately, this patient’s cognitive disorder prevented a timely and less invasive bedside biopsy and required a surgical biopsy for which anticoagulation therapy was interrupted. A less invasive biopsy and timelier laboratory findings may have avoided triggers, including trauma from the surgical biopsy and interruptions in anticoagulation therapy, which may have contributed to the onset of CAPS.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Asherson RA, Cervera R, Piette J, et al. Catastrophic antiphospholipid syndrome: Clues to the pathogenesis from a series of 80 patients. Medicine (Baltimore). 2001;80(6):355-377.
2. Cervera R, Asherson RA. Multiorgan failure due to rapid occlusive vascular disease in antiphospholipid syndrome: The ‘catastrophic’ antiphospholipid syndrome. APLAR J Rheumatol. 2004;7(3):254-262.
3. Bayraktar UD, Erkan D, Bucciarelli S, Epinosa G, Asherson R; Catastrophic Antiphospholipid Syndrome Project Group. The clinical spectrum of catastrophic antiphospholipid syndrome in the absence and presence of lupus. J Rheumatol. 2007;34(2):346-352.
4. Erkan D, Leibowitz E, Berman J, Lockshin MD. Perioperative medical management of antiphospholipid syndrome: Hospital for special surgery experience, review of literature, and recommendations. J Rheumatol. 2002;29(4):843-849.
5. Dornan RIP. Acute postoperative biventricular failure associated with antiphospholipid antibody syndrome. Br J Anaesth. 2004;92(5):748-754.
6. Douketis JD, Berger PD, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(suppl 6):S299-S339.
7. Gómez-Puerta JA, Cervera R, Calvo LM, et al. Dementia associated with the antiphospolipid syndrome: Clinical and radiological characteristics of 30 patients. Rheumatology (Oxford). 2005;44(1):95-99.
8. Kao C-H, Lan J-L, Hsieh J-F, Ho Y-J, ChangLai S-P, Lee J-K, et al. Evaluation of regional cerebral blood flow with 99mTc-HMPAO in primary antiphospholipid antibody syndrome. J Nucl Med. 1999;40:1446-1450.
Advanced psychiatric illness and dementia create a wide range of barriers to health care. These patients are unable to provide reliable details with respect to their illness or even discuss basic features of their medical history, forcing providers to rely on contributions from caregiver reports and medical records. Confounding the limits on medical information, physical examinations are often abbreviated or completely refused because of the patient’s distrust, discomfort, or delusion. Over time, the involvement of consulting services may amplify the impact of these barriers as the need for diagnostic and therapeutic interventions emerge. Meanwhile, this delay in definitive management opens a window of risk for deterioration, in which patients cannot be relied on to report important clinical changes.
This case report describes a patient with significant cognitive dysfunction who developed a rare and devastating complication of a hematologic disorder. As the case illustrates, transferring a patient from the psychiatric ward to Internal Medicine (IM) can create unique diagnostic and management challenges.
CASE REPORT
A 64-year-old man developed hematochezia after having been hospitalized in a locked psychiatric ward for the preceding 6 months following a suicide attempt. The episode of hematochezia occurred while on anticoagulation treatment with warfarin for chronic lower extremity deep venous thrombosis (DVT), which prompted the IM consultation. The patient’s past medical history was notable for dementia, hypothyroidism, Crohn disease, and primary sclerosing cholangitis.
The IM Consult Service recommended holding anticoagulation therapy and reversing the coagulopathy with vitamin K. The patient’s stool returned hemoccult and toxin positive for Clostridium difficile (C difficile). The hematochezia was attributed to the infection with C difficile in the setting of anticoagulation. Oral metronidazole was started. Hemoglobin remained stable without further episodes of bleeding. Seven days after the episode of hematochezia, the patient experienced worsening generalized pain and new skin findings. He was transferred to the general medical ward for further management.
The patient’s medical records revealed early cognitive decline with recommendations for supervised residential care as early as age 59 years. An extensive neurocognitive assessment indicated a diagnosis of semantic dementia. He also had a history of recurrent DVT with anticoagulation therapy for > 10 years with no prior workup for a hypercoagulable state. A recent baseline mental status report described a childlike demeanor, profound global speech deficits with marked difficulty understanding even basic medical concepts (eg, the need for a peripheral intravenous catheter), and generalized anxiety disorder complicated by hyperesthesia. The patient frequently refused physical examinations and blood draws as a result. He devoted himself to simple puzzles of kittens and puppies.
Vital signs were normal as were the head and neck, pulmonary, cardiac, and abdominal examinations. The patient’s neurocognitive examination was remarkable for his dependence on instrumental activities of daily living, global aphasia, impaired short- and long-term recall, and poor judgment. He scored 21 out of 30 on a recent mini-mental state examination: failure to achieve 3-word recall; disorientation to month, season, hospital, and county; and an inability to write a sentence or identify a pen. Otherwise, he had fluent speech, facial symmetry, intact strength and sensation throughout, and normal reflexes.
A skin examination revealed diffuse tender subcutaneous lesions. The largest lesion was about 5 cm, located in the left anterolateral thigh. Smaller lesions of about 1 cm were noted in the abdominal wall, right thigh, and bilateral upper extremities. An exquisitely tender, well-demarcated 20-cm elliptical lesion with central necrosis and an erythematous border developed in the left axilla the following day (Figure 1A). Pain limited adduction of the left arm.
The initial laboratory evaluation demonstrated a stable hemoglobin level of 11.1 g/dL, a platelet count of 128 k/mL, and no leukocytosis. Electrolytes and renal indexes were normal. D-dimer and fibrin split products were > 10,000 ng/mL and 20 mg/mL, respectively. Fibrinogen level was 351 mg/dL. The prothrombin time and international normalized ratio were 15.1 seconds and 1.4, respectively. The activated partial thromboplastin time (aPTT) was measured at 40 seconds. High sensitivity C-reactive protein was 4.59. Recent head imaging included a brain magnetic resonance imaging (MRI) notable for enlarged sulci and ventricles with temporal predominance. Positron emission tomography (PET) brain imaging was significant for diffuse hypometabolism in bilateral parietal and temporal lobes with preservation of sensorimotor and occipital cortexes. There was no clear radiographic evidence of cerebral embolic phenomenon or focal cerebrovascular events.
Enoxaparin treatment was initiated for a suspected hypercoagulable state. Ceftriaxone was administered for a urinary tract infection (UTI). Despite premedication, the bedside biopsy of his necrotic skin lesion was aborted due to severe anxiety and generalized somatic pain. A surgical excisional biopsy was thus obtained under general anesthesia. Enoxaparin was held the night before and the morning of surgery. There were no immediate complications related to the biopsy, and malignancy was not seen on intraoperative frozen sections.
Generalized somatic pain persisted the morning after the surgical biopsy, but the patient remained clinically unchanged. An hour later, he was found unresponsive with no pulse. Despite extensive resuscitative efforts, the patient died.
Postmortem
There was a high index of suspicion for a hemostatic perturbation given the skin findings and recent manipulation of anticoagulation with a prior thrombotic event. The axillary lesion closely resembled warfarin-related skin necrosis. Management included enoxaparin with supportive care, pending definitive pathologic findings.
Postmortem examination confirmed diffuse multiorgan involvement similar to the process seen in the thigh biopsy. Ischemic injury secondary to small vessel microthrombi were evident in the skin, subcutaneous fat, large bowel, urinary bladder, and associated pericystic fat (Figure 1B). Interpretation of the surgical thigh biopsy became available after the patient died. It demonstrated infarcted fat with fat necrosis and hemorrhage (Figure 2).
The results of the laboratory investigations for thrombophilia also came back after the patient died. A potent lupus anticoagulant (LA) was demonstrated. It manifested primarily in the intrinsic pathway as a strongly positive LA-sensitive-aPTT (delta time = 20.5 seconds) assay with a weakly positive dilute Russell’s viper venom time assay. The antigenic specificity of the LA antibodies was not uncovered, as the plasma levels of both IgM and IgG anticardiolipin and anti-Β2-glycoprotein-I antibodies were within the reference range. Factor (F) II and FV genotyping revealed wild-type FV, and the prothrombin gene G20210A was without mutation.
Assays for plasma levels of protein S and antithrombin activity were also normal, which excluded deficiencies in these proteins. The assay for protein C activity was slightly decreased. This may have exacerbated the hemostatic imbalance caused by the LA, as the FVII level had normalized. However, the etiology of the protein C deficiency is not clear. Considerations include (1) a warfarin disequilibrium state due to the discontinuation of oral anticoagulation and institution of vitamin K therapy; (2) an epiphenomenon resulting from active thromboses; or (3) a possible hereditary protein C deficiency.
The definitive diagnosis of the catastrophic antiphospholipid antibody (APA) syndrome relies on multiorgan failure in < 1 week, histopathologic evidence of small vessel thrombosis, and a positive LA.1 The study patient fulfilled these criteria (Table).
DISCUSSION
Catastrophic progression of APA syndrome is an infrequent and devastating complication of this autoimmune disorder with a mortality rate of nearly 50%.1 Antiphospholipid antibody syndrome typically presents with thromboses of the larger vessels, and it more commonly affects the venous system. In contrast, diffuse small vessel thromboses underlie the pathogenesis of catastrophic APA syndrome (CAPS).2 This catastrophic progression occurs in < 1 out of 100 patients with the APA syndrome, more frequently in women (69%), and over an age range of 7 decades (mean 38 years).2 A case series analysis identified older age (aged > 36 years), history of systemic lupus erythematous, and broader organ involvement as prognostic indicators of a poor outcome. Better outcomes are associated with thrombocytopenia and anticoagulation treatment. However, gender did not influence mortality.3
Prevention is key to APA management, given the lack of efficacious treatment.2 Preventive measures are focused on avoiding triggers and aggressively treating those triggers that may arise. Possible triggers in this case included cessation of anticoagulation due to hematochezia and in anticipation of surgery, infection (C difficile colitis, suspected necrotic skin wound super infection, and a UTI), and biopsy-related trauma.
Initial clinical stability in this patient with abrupt decompensation along with pending laboratory and pathology results limited the opportunity for more aggressive therapeutic intervention for CAPS. Moreover, the relative sparing of the cardiopulmonary and renal systems contrasted with the more classical systemic involvement usually seen in CAPS. Second-line therapies for CAPS include plasma exchange and high-dose steroids.2 Third-line therapeutics include immunosuppressive agents, such as cyclophosphamide.2
The rapid decompensation, described on postoperative day 1, after a low-risk surgical biopsy highlights the importance of perioperative care in patients with this autoimmune condition. Following a review of surgical cases, Erkan and colleagues concluded that standard antithrombotic regimens for general and orthopedic surgery are likely to undertreat patients with APA syndrome.4 They recommend the following guidelines in place of standard antithrombotic management: preoperative platelet count > 100 k/µL, higher threshold before proceeding with surgery/interventional procedures, limiting intravascular manipulations, and minimizing periods without anticoagulation therapy.4
A case report of a 31-year-old female undergoing mitral valve replacement complicated postoperatively by CAPS-associated biventricular failure, despite preoperative transition of warfarin to unfractionated heparin, illustrates this significant perioperative risk.5 Evidence-based guidelines recommend holding enoxaparin 24 hours before surgery and 24 hours after invasive procedures in patients requiring bridging anticoagulation therapy.6
Treatment of the patient in this case was complicated by his cognitive impairment. Dementia is a less common but well-documented consequence of APA syndrome. A case review of 28 patients with the APA syndrome and dementia suggests an early onset of cognitive decline with a mean age of 49 years. There may be no clear preceding history of stroke in > 50% of patients.7 Interestingly, dementia followed initial manifestations of disease by an average of 3.5 years, even in some patients receiving anticoagulation therapy.7
A nuclear medicine study of 22 patients with APA syndrome and mild neuropsychiatric symptoms demonstrated a 73% incidence of cerebral hypoperfusion (55% diffuse and 18% local) based on PET imaging despite unremarkable MRI findings.8 Extended periods of hypoperfusion secondary to arterial thromboses in the temporal and parietal lobes may have been the primary etiology for dementia in this case. As such, the coexistence of neurologic abnormalities and a hypercoagulability state warrants a thorough diagnostic workup for similar disorders, despite the higher prevalence of dementia in advanced age.
Unfortunately, this patient’s cognitive disorder prevented a timely and less invasive bedside biopsy and required a surgical biopsy for which anticoagulation therapy was interrupted. A less invasive biopsy and timelier laboratory findings may have avoided triggers, including trauma from the surgical biopsy and interruptions in anticoagulation therapy, which may have contributed to the onset of CAPS.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Advanced psychiatric illness and dementia create a wide range of barriers to health care. These patients are unable to provide reliable details with respect to their illness or even discuss basic features of their medical history, forcing providers to rely on contributions from caregiver reports and medical records. Confounding the limits on medical information, physical examinations are often abbreviated or completely refused because of the patient’s distrust, discomfort, or delusion. Over time, the involvement of consulting services may amplify the impact of these barriers as the need for diagnostic and therapeutic interventions emerge. Meanwhile, this delay in definitive management opens a window of risk for deterioration, in which patients cannot be relied on to report important clinical changes.
This case report describes a patient with significant cognitive dysfunction who developed a rare and devastating complication of a hematologic disorder. As the case illustrates, transferring a patient from the psychiatric ward to Internal Medicine (IM) can create unique diagnostic and management challenges.
CASE REPORT
A 64-year-old man developed hematochezia after having been hospitalized in a locked psychiatric ward for the preceding 6 months following a suicide attempt. The episode of hematochezia occurred while on anticoagulation treatment with warfarin for chronic lower extremity deep venous thrombosis (DVT), which prompted the IM consultation. The patient’s past medical history was notable for dementia, hypothyroidism, Crohn disease, and primary sclerosing cholangitis.
The IM Consult Service recommended holding anticoagulation therapy and reversing the coagulopathy with vitamin K. The patient’s stool returned hemoccult and toxin positive for Clostridium difficile (C difficile). The hematochezia was attributed to the infection with C difficile in the setting of anticoagulation. Oral metronidazole was started. Hemoglobin remained stable without further episodes of bleeding. Seven days after the episode of hematochezia, the patient experienced worsening generalized pain and new skin findings. He was transferred to the general medical ward for further management.
The patient’s medical records revealed early cognitive decline with recommendations for supervised residential care as early as age 59 years. An extensive neurocognitive assessment indicated a diagnosis of semantic dementia. He also had a history of recurrent DVT with anticoagulation therapy for > 10 years with no prior workup for a hypercoagulable state. A recent baseline mental status report described a childlike demeanor, profound global speech deficits with marked difficulty understanding even basic medical concepts (eg, the need for a peripheral intravenous catheter), and generalized anxiety disorder complicated by hyperesthesia. The patient frequently refused physical examinations and blood draws as a result. He devoted himself to simple puzzles of kittens and puppies.
Vital signs were normal as were the head and neck, pulmonary, cardiac, and abdominal examinations. The patient’s neurocognitive examination was remarkable for his dependence on instrumental activities of daily living, global aphasia, impaired short- and long-term recall, and poor judgment. He scored 21 out of 30 on a recent mini-mental state examination: failure to achieve 3-word recall; disorientation to month, season, hospital, and county; and an inability to write a sentence or identify a pen. Otherwise, he had fluent speech, facial symmetry, intact strength and sensation throughout, and normal reflexes.
A skin examination revealed diffuse tender subcutaneous lesions. The largest lesion was about 5 cm, located in the left anterolateral thigh. Smaller lesions of about 1 cm were noted in the abdominal wall, right thigh, and bilateral upper extremities. An exquisitely tender, well-demarcated 20-cm elliptical lesion with central necrosis and an erythematous border developed in the left axilla the following day (Figure 1A). Pain limited adduction of the left arm.
The initial laboratory evaluation demonstrated a stable hemoglobin level of 11.1 g/dL, a platelet count of 128 k/mL, and no leukocytosis. Electrolytes and renal indexes were normal. D-dimer and fibrin split products were > 10,000 ng/mL and 20 mg/mL, respectively. Fibrinogen level was 351 mg/dL. The prothrombin time and international normalized ratio were 15.1 seconds and 1.4, respectively. The activated partial thromboplastin time (aPTT) was measured at 40 seconds. High sensitivity C-reactive protein was 4.59. Recent head imaging included a brain magnetic resonance imaging (MRI) notable for enlarged sulci and ventricles with temporal predominance. Positron emission tomography (PET) brain imaging was significant for diffuse hypometabolism in bilateral parietal and temporal lobes with preservation of sensorimotor and occipital cortexes. There was no clear radiographic evidence of cerebral embolic phenomenon or focal cerebrovascular events.
Enoxaparin treatment was initiated for a suspected hypercoagulable state. Ceftriaxone was administered for a urinary tract infection (UTI). Despite premedication, the bedside biopsy of his necrotic skin lesion was aborted due to severe anxiety and generalized somatic pain. A surgical excisional biopsy was thus obtained under general anesthesia. Enoxaparin was held the night before and the morning of surgery. There were no immediate complications related to the biopsy, and malignancy was not seen on intraoperative frozen sections.
Generalized somatic pain persisted the morning after the surgical biopsy, but the patient remained clinically unchanged. An hour later, he was found unresponsive with no pulse. Despite extensive resuscitative efforts, the patient died.
Postmortem
There was a high index of suspicion for a hemostatic perturbation given the skin findings and recent manipulation of anticoagulation with a prior thrombotic event. The axillary lesion closely resembled warfarin-related skin necrosis. Management included enoxaparin with supportive care, pending definitive pathologic findings.
Postmortem examination confirmed diffuse multiorgan involvement similar to the process seen in the thigh biopsy. Ischemic injury secondary to small vessel microthrombi were evident in the skin, subcutaneous fat, large bowel, urinary bladder, and associated pericystic fat (Figure 1B). Interpretation of the surgical thigh biopsy became available after the patient died. It demonstrated infarcted fat with fat necrosis and hemorrhage (Figure 2).
The results of the laboratory investigations for thrombophilia also came back after the patient died. A potent lupus anticoagulant (LA) was demonstrated. It manifested primarily in the intrinsic pathway as a strongly positive LA-sensitive-aPTT (delta time = 20.5 seconds) assay with a weakly positive dilute Russell’s viper venom time assay. The antigenic specificity of the LA antibodies was not uncovered, as the plasma levels of both IgM and IgG anticardiolipin and anti-Β2-glycoprotein-I antibodies were within the reference range. Factor (F) II and FV genotyping revealed wild-type FV, and the prothrombin gene G20210A was without mutation.
Assays for plasma levels of protein S and antithrombin activity were also normal, which excluded deficiencies in these proteins. The assay for protein C activity was slightly decreased. This may have exacerbated the hemostatic imbalance caused by the LA, as the FVII level had normalized. However, the etiology of the protein C deficiency is not clear. Considerations include (1) a warfarin disequilibrium state due to the discontinuation of oral anticoagulation and institution of vitamin K therapy; (2) an epiphenomenon resulting from active thromboses; or (3) a possible hereditary protein C deficiency.
The definitive diagnosis of the catastrophic antiphospholipid antibody (APA) syndrome relies on multiorgan failure in < 1 week, histopathologic evidence of small vessel thrombosis, and a positive LA.1 The study patient fulfilled these criteria (Table).
DISCUSSION
Catastrophic progression of APA syndrome is an infrequent and devastating complication of this autoimmune disorder with a mortality rate of nearly 50%.1 Antiphospholipid antibody syndrome typically presents with thromboses of the larger vessels, and it more commonly affects the venous system. In contrast, diffuse small vessel thromboses underlie the pathogenesis of catastrophic APA syndrome (CAPS).2 This catastrophic progression occurs in < 1 out of 100 patients with the APA syndrome, more frequently in women (69%), and over an age range of 7 decades (mean 38 years).2 A case series analysis identified older age (aged > 36 years), history of systemic lupus erythematous, and broader organ involvement as prognostic indicators of a poor outcome. Better outcomes are associated with thrombocytopenia and anticoagulation treatment. However, gender did not influence mortality.3
Prevention is key to APA management, given the lack of efficacious treatment.2 Preventive measures are focused on avoiding triggers and aggressively treating those triggers that may arise. Possible triggers in this case included cessation of anticoagulation due to hematochezia and in anticipation of surgery, infection (C difficile colitis, suspected necrotic skin wound super infection, and a UTI), and biopsy-related trauma.
Initial clinical stability in this patient with abrupt decompensation along with pending laboratory and pathology results limited the opportunity for more aggressive therapeutic intervention for CAPS. Moreover, the relative sparing of the cardiopulmonary and renal systems contrasted with the more classical systemic involvement usually seen in CAPS. Second-line therapies for CAPS include plasma exchange and high-dose steroids.2 Third-line therapeutics include immunosuppressive agents, such as cyclophosphamide.2
The rapid decompensation, described on postoperative day 1, after a low-risk surgical biopsy highlights the importance of perioperative care in patients with this autoimmune condition. Following a review of surgical cases, Erkan and colleagues concluded that standard antithrombotic regimens for general and orthopedic surgery are likely to undertreat patients with APA syndrome.4 They recommend the following guidelines in place of standard antithrombotic management: preoperative platelet count > 100 k/µL, higher threshold before proceeding with surgery/interventional procedures, limiting intravascular manipulations, and minimizing periods without anticoagulation therapy.4
A case report of a 31-year-old female undergoing mitral valve replacement complicated postoperatively by CAPS-associated biventricular failure, despite preoperative transition of warfarin to unfractionated heparin, illustrates this significant perioperative risk.5 Evidence-based guidelines recommend holding enoxaparin 24 hours before surgery and 24 hours after invasive procedures in patients requiring bridging anticoagulation therapy.6
Treatment of the patient in this case was complicated by his cognitive impairment. Dementia is a less common but well-documented consequence of APA syndrome. A case review of 28 patients with the APA syndrome and dementia suggests an early onset of cognitive decline with a mean age of 49 years. There may be no clear preceding history of stroke in > 50% of patients.7 Interestingly, dementia followed initial manifestations of disease by an average of 3.5 years, even in some patients receiving anticoagulation therapy.7
A nuclear medicine study of 22 patients with APA syndrome and mild neuropsychiatric symptoms demonstrated a 73% incidence of cerebral hypoperfusion (55% diffuse and 18% local) based on PET imaging despite unremarkable MRI findings.8 Extended periods of hypoperfusion secondary to arterial thromboses in the temporal and parietal lobes may have been the primary etiology for dementia in this case. As such, the coexistence of neurologic abnormalities and a hypercoagulability state warrants a thorough diagnostic workup for similar disorders, despite the higher prevalence of dementia in advanced age.
Unfortunately, this patient’s cognitive disorder prevented a timely and less invasive bedside biopsy and required a surgical biopsy for which anticoagulation therapy was interrupted. A less invasive biopsy and timelier laboratory findings may have avoided triggers, including trauma from the surgical biopsy and interruptions in anticoagulation therapy, which may have contributed to the onset of CAPS.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Asherson RA, Cervera R, Piette J, et al. Catastrophic antiphospholipid syndrome: Clues to the pathogenesis from a series of 80 patients. Medicine (Baltimore). 2001;80(6):355-377.
2. Cervera R, Asherson RA. Multiorgan failure due to rapid occlusive vascular disease in antiphospholipid syndrome: The ‘catastrophic’ antiphospholipid syndrome. APLAR J Rheumatol. 2004;7(3):254-262.
3. Bayraktar UD, Erkan D, Bucciarelli S, Epinosa G, Asherson R; Catastrophic Antiphospholipid Syndrome Project Group. The clinical spectrum of catastrophic antiphospholipid syndrome in the absence and presence of lupus. J Rheumatol. 2007;34(2):346-352.
4. Erkan D, Leibowitz E, Berman J, Lockshin MD. Perioperative medical management of antiphospholipid syndrome: Hospital for special surgery experience, review of literature, and recommendations. J Rheumatol. 2002;29(4):843-849.
5. Dornan RIP. Acute postoperative biventricular failure associated with antiphospholipid antibody syndrome. Br J Anaesth. 2004;92(5):748-754.
6. Douketis JD, Berger PD, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(suppl 6):S299-S339.
7. Gómez-Puerta JA, Cervera R, Calvo LM, et al. Dementia associated with the antiphospolipid syndrome: Clinical and radiological characteristics of 30 patients. Rheumatology (Oxford). 2005;44(1):95-99.
8. Kao C-H, Lan J-L, Hsieh J-F, Ho Y-J, ChangLai S-P, Lee J-K, et al. Evaluation of regional cerebral blood flow with 99mTc-HMPAO in primary antiphospholipid antibody syndrome. J Nucl Med. 1999;40:1446-1450.
1. Asherson RA, Cervera R, Piette J, et al. Catastrophic antiphospholipid syndrome: Clues to the pathogenesis from a series of 80 patients. Medicine (Baltimore). 2001;80(6):355-377.
2. Cervera R, Asherson RA. Multiorgan failure due to rapid occlusive vascular disease in antiphospholipid syndrome: The ‘catastrophic’ antiphospholipid syndrome. APLAR J Rheumatol. 2004;7(3):254-262.
3. Bayraktar UD, Erkan D, Bucciarelli S, Epinosa G, Asherson R; Catastrophic Antiphospholipid Syndrome Project Group. The clinical spectrum of catastrophic antiphospholipid syndrome in the absence and presence of lupus. J Rheumatol. 2007;34(2):346-352.
4. Erkan D, Leibowitz E, Berman J, Lockshin MD. Perioperative medical management of antiphospholipid syndrome: Hospital for special surgery experience, review of literature, and recommendations. J Rheumatol. 2002;29(4):843-849.
5. Dornan RIP. Acute postoperative biventricular failure associated with antiphospholipid antibody syndrome. Br J Anaesth. 2004;92(5):748-754.
6. Douketis JD, Berger PD, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(suppl 6):S299-S339.
7. Gómez-Puerta JA, Cervera R, Calvo LM, et al. Dementia associated with the antiphospolipid syndrome: Clinical and radiological characteristics of 30 patients. Rheumatology (Oxford). 2005;44(1):95-99.
8. Kao C-H, Lan J-L, Hsieh J-F, Ho Y-J, ChangLai S-P, Lee J-K, et al. Evaluation of regional cerebral blood flow with 99mTc-HMPAO in primary antiphospholipid antibody syndrome. J Nucl Med. 1999;40:1446-1450.