User login
Recently, the U.S. Department of Homeland Security redefined disasters into 4 types: natural hazards, societal hazards, technologic hazards, and terrorism. The incidence of manmade and natural disasters is on the rise in intensity and frequency globally. Recent events such as tornadoes and hurricanes in the southeastern U.S., tsunamis in Japan, earthquakes in Haiti, wild fires, heat waves, and terrorist attacks like that of September 11, 2001, underscore the urgency of developing and maintaining solid local public health disaster response plans to minimize mortality and morbidity.
The 2010 BP oil spill in the Gulf of Mexico, the largest in history, hurricane Katrina, and the lingering impact of hurricane Sandy on the East Coast further raise concerns about our communities’ ability to handle disasters, especially in the early hours after events, when federally coordinated help is being organized and not yet fully available locally or from other nations.1 The recent fertilizer plant explosion in West Texas, the 2013 Boston marathon bombing, and the Newtown, Connecticut, massacre remind us of the unpredictable nature of both manmade and natural disasters.
Coordinated Response
Regardless of its origin, residents expect a coordinated local response during an emergency, and it is important that government agencies meet this expectation. Fulfilling these expectations, however, takes many partners, and it is important to have a clear idea of who is involved in emergency preparedness (EP) and the response of each partner’s role.
Role of Government
Federal, state, and local governments have a critical role in emergency management (EM). When state government, local government, or an individual entity is overwhelmed with a disaster, the role of the Federal Emergency Management Agency is to provide assistance and resources to cope with the emergency.2 Private industry and traditional disaster relief agencies, such as the American Red Cross and the Adventist Development and Relief Agency, are also involved in response efforts. Recent examples have shown that these partnerships are often overwhelmed with the needs of large regions experiencing limited resources. Therefore, hospitals and local public health departments frequently must carry much of the immediate burden of stabilizing communities and coordinating response with government agencies and local partners.3
Role of Public Health and the CDC
Federal agencies and local public health departments have been given critical roles in planning and responding to disasters. In particular, the PHS focuses on population care and shapes how public health entities should respond to mass casualty events and pandemics, including local response coordination. The CDC is primarily responsible for assisting state and local governments with disaster response and recovery after a large-scale public health emergency.3 The CDC works closely with local public health departments in decision making; tracking the source, spread, and severity of health threats; assessing impacts; educating the public on how to safeguard their health; and implementing measures to protect the public. During a large-scale health emergency, the CDC also maintains and provides resources through the maintenance and distribution of the nation’s Strategic National Stockpile of medications and supplies that may be needed during events such as the recent 2009 H1N1 influenza outbreak or other public health emergencies.3
Role of Local Businesses and Professional Institutions
Nationally, businesses and professional institutions are coming together and organizing in such a way that places them as part of the solution. More specifically, the National Voluntary Organizations Active in Disaster and Community Organizations Active in Disaster have grown exponentially since September 11, 2001.4 These efforts include but are not limited to development of EP plans and the subsequent sharing of those plans, sharing of key assets critical to response activities, development of a community key asset database, and training/exercise participation.
Role of Hospitals
The Hospital Preparedness Program was developed to prepare the nation’s health care system to respond appropriately to mass casualty incidents, whether due to bioterrorism, natural disaster, or other public health emergencies. Health care systems must be able to develop a disaster medical capability that is rapid, flexible, sustainable, integrated, coordinated, and capable of providing appropriate care in the most ethical manner with the resources and capabilities it has at its disposal.3 Although involved as first responders, traditionally, medical care systems, hospitals, physicians, and pharmacists are faced with the dual task of individual patient care and are thus more limited as partners in an overall local response system.
Also vital to this discussion is the reality that hospital emergency departments (EDs) already routinely operate at or above capacity, limiting their ability to prepare for mass casualties due to a public health disaster. Hospitals continue to divert more than half a million ambulances per year due to ED overcrowding.3 How they could step up in a true emergency situation is questionable at best.
Role of First Responders
Individuals who respond immediately are referred to as first responders. First responders come in 2 archetypes: those who are there purely based on unexpected circumstances and take action and those who are trained first responders, such as firefighters, police officers, and emergency medical technicians (EMTs). These first responders are trained to partner with one another. Firefighters primarily handle fire rescue as well as assessing the extent of potential damage to the area. Law enforcement’s responsibility is to restore order after an emergency, whether it is a natural disaster, community disturbance, or outbreak of hazardous chemicals. An EMT’s role is to attend to the immediate medical care of patients who have been injured or become ill during the emergency.5
Related: Disaster Preparedness for Veterans With Dementia and Their Caregivers
There are occasions where other potential incident responders, such as health care professionals, can play a key role and yet are not integrated into the emergency response. The VHA needs to focus on this facet in order to more effectively respond to events that threaten lives, property, and current infrastructure of the veterans it serves.
Role of CBOCs and Private Physician Practices
Community-based outpatient clinics (CBOCs), including outpatient community health centers and private physician practices (PPPs), maintain and improve routine community health but are rarely involved in routine planning for disasters. They are, therefore, typically not open for business or may have limited hours as they recover from the event. This results in patients who do not have access to their primary care providers (PCPs) turning to EDs, which are already at capacity. As a result, in a disaster the costly and overburdened ED functions as the PCP site for even larger populations affected by a disaster, including those who are uninsured.6,7
Kahan and colleagues reported that two-thirds of patients preferred their family doctor or health care authorities as their first choice for care instead of receiving care in the ED.8 Researchers found that 89% of physicians in private practice felt it was their responsibility to treat, for example, patients infected with anthrax.8 Some argue that if PCPs are included in planning and appropriately trained in disaster preparedness, their attitudes and willingness to participate in emergency services would follow.9
Given the many challenges to disaster preparedness, CBOCs could be a critical partner in EM, and interest continues to grow to explore that role. Health professionals in CBOCs who are trained in disaster management (DM) could become active participants in early intervention to initiate the treatment of patients in rescue efforts during a disaster.10 For instance, a CBOC could triage patients in a postdisaster situation, thus limiting the burden on hospital EDs by evaluating populations at risk and providing them with important information when communication is difficult.
This already existing network of community-based triage stations would offer natural locations to assess the health needs of the population and determine their level of appropriate medical care. Additionally, these clinics can ensure continuation of basic services after initial medical care has been completed in the hospital setting.10 Because clinics have not been included in coordinated DM, there is scant literature that addresses their potential role in disaster response. Community-based outpatient clinics and PPPs are untapped resources; however, it is unknown whether medical staff in these medical clinics have the interest, training, knowledge, skills, and resources in DM or whether barriers to providing safe care can be overcome.10
Case Study
The VHA is the largest integrated health care system in the U.S. It is mandated to serve as a backup to the DoD during disasters, and VHA CBOCs can play an important role.11,12 The CBOCs are staffed with a medical director, nurse manager, and other clinical and support staff. As a study population, CBOCs are well suited to examine and explore staff attitudes and roles in DM. To date, no research reports have been found studying EP in CBOCs.
The purpose of this study was to learn how to best integrate the CBOCs into disaster response. This qualitative study aimed to answer 3 questions: (1) How do VA clinic personnel perceive their personal and their clinic’s risk, level of preparedness, role, and knowledge for an active response in a disaster; (2) What do VA clinic personnel perceive they need in order to function in a disaster; and (3) What resources are necessary for clinic staff to function competently in a disaster?
Methods
In this qualitative study, in-depth semistructured key informant (KI) interviews (N = 3) and focus group discussions (N = 20) guided by risk perception theory and the Andersen Behavioral Model of Health Services Use were conducted and analyzed using grounded theory methods to contextualize the potential of local clinics in disaster response.13-15 To optimize breadth of viewpoints on this issue, participants were selected by theoretical sampling methods to explore perceptions of leadership and line staff.
Study Location
Health care providers and support staff from 3 southern California CBOCs that are contracted by the local VA to provide primary care services (ie, internal medicine, geriatrics, women’s health, mental health, and some specialty care services) to veterans were recruited for this study. The CBOCs are generally connected with a VHA local hospital in their region, offer services 5 days a week, and are closed on weekends and federal holidays. Some VA CBOCs participate in telehealth remote services connected to their regional hospital to help manage their patient populations. The CBOCs are managed by a medical director and a clinic manager and report to their respective VISN, and each VISN reports to the VHA Central Office in Washington, DC.13,15 The CBOC staff includes physicians, nurse practitioners, physician assistants, registered nurses (RNs), licensed vocational nurses (LVNs), medical assistants, front office staff, social workers, case managers, counselors, pharmacists, and nonclinical staff.
In this case, the CBOCs are contracted by Loma Linda University Health to manage care of the veterans and agree to care for nonveterans in a disaster. The CBOCs contracted or not all fall under the criteria as set forth in VHA Handbook 1006.1. This handbook criteria indicate that CBOCs must maintain appropriate emergency response capability. Additionally, VHA Handbook 0320.1 states that the CBOC is responsible for developing, implementing, evaluating, and improving a CBOC Comprehensive Emergency Management Program (CEMP) and for participating in the VAMC Emergency Management Committee. The scope of the VISN-wide CEMP integrates VAMC and VISN EM programs to coordinate and enhance operations during planned and unplanned events.
Study Design and Sample
After receiving institutional review board approval, 3 in-depth semi-structured clinic leadership KI interviews and 3 clinic staff (RNs, LVNs, health technicians, and nursing assistants) focus group discussions (N = 20, 1 per CBOC) to follow up on information gleaned from the analyses of the initial KIs were conducted. To provide continuity, all were conducted by the same trained facilitator who used a semistructured KI outline with questions and probes based on the guiding study framework.
Data Collection and Content Analysis
Interviews and focus group discussions were audio recorded and transcribed verbatim and then analyzed using grounded theory methods. Line-by-line coding was done to develop an initial inductive codebook, which was then organized into final codes. Once the codebook was developed, it was applied to all transcripts.
Related: Pre-Storm Dialysis Saves Lives
Transcripts and resulting codes were reviewed 3 times by independent reviewers to validate data, ensure accuracy, and delete any information that might identify participants. Pseudonyms were used to represent the participants by perspective (eg, nurse, MD) to avoid confusion in data analysis. A 4-stage data analysis approach was used: (1) immersion in the raw data by listening to tapes and reading manuscripts and notes in order to list key ideas and recurrent themes using a constant comparison method; (2) indexing by applying the thematic framework systematically to the data using and seeking new, unanticipated emerging codes; (3) arranging the data in codes and concepts/themes that represent the thematic framework of EP in clinics; (4) identifying a thematic framework for EP using codes that identified key issues, concepts, and themes that can be referenced and derived from the text.
Results
The Table describes the 4 primary emerging themes and corresponding quotes: (1) EP barriers, including lack of direction, training, and tools, which would result in negative outcomes; (2) perceived personal and clinic risk for a disaster, including negative outcomes and personal family safety; (3) perceptions of roles and responsibilities in EP, including intent to participate in DM at various staffing levels as well as patient expectations for care; and (4) existing resources that influence EP and the ability to survive a disaster collectively.
Emergency preparedness barriers. Although most respondents realized their potentially critical role in an emergency, they expressed recurrent barrier themes centered on their perceived lack of training, lack of tools to function, and lack of direction to be effective in a disaster response. Lack of knowledge of EP was identified as a great need by multiple participants. One participant stated, “Lack of information is so destructive. If you don’t know how to keep yourself from those things you don’t know…such as in a situation that’s going to be tragic, it is because of a lack of information or a lack of training. And I see that so many times…Mandate that we do our classes, so we know what we’re doing.” Another stated in reference to lack of skills, “I haven’t experienced any drills or anything like that. So I know what is going to happen here.”
Lack of abilities to communicate with key DM players also were identified. For example, “Downed power lines may result in no telephone connection to communicate next steps for critical issues, such as if evacuation of the clinic is required.” Another respondent indicated, “We need backup communication...devices, wind-up radios, or whatever.”
Lack of a clear disaster plan was also identified. Questions arose centered on details—how to actually implement a clinic response plan, including concerns that there were none, as the respondents “had not seen the plan in a couple of years” and were not sure who really was in charge of giving directions. Lack of community/organizational support voiced included aspects such as interdepartmental, facility, and community resource connectedness. There was acknowledgement that department assets should be clearly identified so that resource sharing might be used as part of the plan.
Last, regarding lack of resources, one participant said, “We don’t have the resources. We don’t have gurneys. We don’t have enough wheel chairs….We don’t have a crash cart. We don’t have the triage tarps or whatever for the triage of people; we don’t have any supplies to supply the energy room for diabetics, like what they have in the ER.”
Perceived personal and clinic risk for a disaster. Participants stated they felt at risk for natural disasters, including fire, floods, and earthquakes, but expressed concerns and even more fears about how they would handle a response to bombings, spills of hazardous materials, airplane accidents, and gunfire, which also qualify as disasters but are much harder to prepare for, because they could be so varied. One participated stated, “They are so unpredictable whether it is an earthquake or a fire…they are unpredictable….We see planes that fly close to our window and we wonder about the possibility of a crash—you never know.”
Many staff members expressed fear of what these disasters would mean to them in the clinic and to their patients. Another comment shared was, “I don’t think anybody really thinks about this kind of stuff until it happens and then it is too late…If we had just done this or that or knew how to do this or that then…” The biggest fear expressed was that of a massive earthquake in which there would be power outages and resulting fires, blocked building exits, and no way to get to evacuation areas. Fears expressed included working with people who are dying and trying to get the patients down the stairs and out of the disaster area.
Personal safety in a disaster was also a concern; a nurse stated, “Your personal safety is a priority. Yourself, that is first, if you are not safe, you can’t do any good to anyone else.” Another shared concern was the safety of family members during a disaster and conflicting obligations between duties at work and protecting family members. Participants felt they would want to be at home with their families.
Perceptions of roles and responsibilities in EP. Supervisors of the clinics shared that their primary responsibility is to the staff and their current patients; ensuring their safety was a top priority. Their knowledge, skills, and available resources were crucial to their duties, including establishing methods of communication outside the clinic for advice and direction, such as notifying the power company and other outside agencies of the condition of the clinic. They felt that their duties included making sure generators were working, ensuring telephones and lighting were available, and advising staff when to leave the building. One manager stated that more EP discussions need to happen in order to determine how to react: “...in event of a disaster it is important to control patient flow, staffing the clinic appropriately and managing the employees.” They felt a need to help empower their staff by making sure staff were trained in EP tasks and that they could complete the tasks they were required to perform.
Staff consistently reported that the doctors were in charge of providing direction concerning activities and care of the patients. However, most were able to identify their own role in helping preserve lives and keeping the patients and other staff safe. One nurse stated, “My job would be to evacuate the physicians’ offices, to make sure they are aware of the disaster, get them out safely, put an X on their door, keep the patients calm and guide them out to the designated area, then look out for medics or other help so that they would be directed to the correct locations.” Another staff nurse stated, “My role is to check the bathrooms and then under the direction of the physician assist in the care of patient injuries.”
When asked about the expectations of patients for care during a disaster, staff consistently stated that patients and their families would want to get care and direction from clinic staff who knew them instead of going to the hospital for care. Staff anticipated that patients would be calling the clinic first to discuss their medical problems. One stated, “The veterans would head to us…. We can’t turn them away.” Some staff indicated that some patients might have to go to the ED for care instead of coming to the clinic, because the clinic may not be equipped to respond, noting that “we have to remind [the patients] that in our clinic we have minimal abilities.”
Existing resources. Consistently, the respondents verbalized the importance of acquiring knowledge and skills and using available resources in their disaster plan. They felt that training was critical and that it needed to be simple and uncomplicated. Many felt that they did not have sufficient drills to maintain their knowledge and skills for all types of events. One nursing assistant stated he had extensive training in the military in DM, but clinics did not have sufficient training and were not prepared to handle multiple casualties. Others stated that it would be important for training to be “second nature” so they would not have to think much about it, with everyone pulling together and performing tasks seamlessly. However, some stated that they did not know what to do in an emergency.
Critical resources noted were access to emergency power sources, transistor radios, telephone and communication, 911 services, backup phone services, computers, and text pagers and cell phones so that connections could be made outside the clinic setting. Other critical resources needed included medical supplies and access to food for 1 week.
Finally, teamwork was identified as a critical factor for success. One example involved the clinic responding to a severe snowstorm; the medical director, lead nurse, and support staff agreed to remain on site to assist with any patients who needed help. “We shared our 4-wheel drive trucks to get around, and others called patients, advising them of storm conditions and what to do to maintain care at home and canceled appointments scheduled for that day.” They were very proud of the way they had pooled their resources to support each other and their patients.
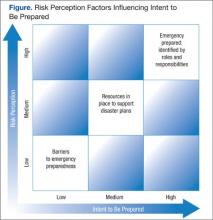
Based on these emerging themes and the inquiry guiding theories, a theoretical framework was proposed on how contributing factors influenced the process by which CBOC staff viewed their roles and the likelihood that they would participate in a disaster plan (Figure). The framework suggests that personal risks and perceived personal and clinic readiness to respond to an emergency were critical barriers to staff willingness to get involved in preparedness, whereas they saw the provision of training and resources as necessary to increase their resilience and ability to function in a disaster.
Clearly addressing barriers through training, planning, ensuring that resources functioned effectively in a disaster, and clarifying roles and responsibilities, combined with promoting personal and clinic readiness facilitated staff EP participation.
Discussion
This qualitative study explored issues surrounding the role of CBOCs in EP and how risk perception and enabling factors contributed to staff intent to participate in DM. As in many qualitative studies, findings were somewhat limited by an overall small sample size (N = 23) across 3 CBOCs in southern California. However, given the lack of available literature, the authors believe that this study helped provide critical insight into CBOC clinic staff’s willingness and readiness to be active in disaster response. The study clearly points to clinic staff’s openness to actively take part in regional disaster response and calls for better and more standardized approaches to EP and DM planning that include local CBOCs. The authors identified factors that contribute to staff intent to participate in DM and the need to reduce barriers that hinder participation.
In general, clinic staff who reported feeling inadequately prepared for disasters (ie, felt more vulnerable) and staff with firsthand disaster experience were more inclined to prepare than were those without experience. Without clearly spelled-out expectations, staff tend to depend and wait on others to lead in a disaster. They noted a desire for better preparation and thus, clarity of roles, need for a reliable method of communication with the outside world during a disaster, and the required equipment and supplies for self-care or care of the patients for ≥ 3 days post disaster. Some indicated that they did not have the resources to provide medical care on the scale that may be required.
Many did not have a clear understanding of an all-hazard approach plan and had not been involved in hazard assessments. Already tightly staffed for personal health care delivery, staff spent minimal time and energy thinking about the risk of a disaster or preparing for one. However, there seemed to be a direct relationship between the attitude of the supervisor and the attitudes of clinic staff to EP. Although these qualitative results are encouraging and point to these clinics as an important undertapped resource for EP, further quantitative studies should expand this inquiry.
Lessons learned from this study include the need to expand qualitative data collection to include a larger sample size to retrieve information that would contribute to a better understanding of how staff view their roles in DM. There are 152 VAMCs and hundreds of associated CBOCs that should be queried as to their EM readiness. Also, replicating this study in non-VHA clinics, such as private CBOCs and PPPs, might bring greater insight into what is needed to involve them in DM plans. Finally, future studies should determine clearer criteria when care can be provided at a clinic and when it would be appropriate for the patient to report at their local ED.
Conclusions and Recommendations
Given the VHA EP mandate, the authors recommend the following steps to address barriers identified in this study: (1) Develop a more structured approach to DM in a CBOC setting to provide staff with a clear understanding of their roles and responsibilities; (2) Conduct a comprehensive assessment of each clinic to determine staff knowledge, skills, and resources required to provide EP and institute a DM training curriculum; (3) Provide clinic leadership with direction on developing a disaster plan as well as how to partner with their primary and local VA health care system, especially onsite physicians, to provide effective DM leadership; (4) Recruit staff into routine drills for natural disasters and expand to an all-hazard approach to manmade disasters to identify gaps in delivering DM in a disaster; (5) Facilitate partnerships and a standardized approach to DM between CBOCs within the VISN by scheduling routine video and teleconferencing, live meetings, and webinars so that procedures and language are clearly understood and communicated between facilities; and (6) Identify key barriers to clinic preparedness by assessing EP elements through mock disaster drills and offer solutions to fill DM gaps.
The authors also recommend that CBOCs should be included in community DM and EP plans in order to understand how to integrate resources in a disaster. Networking, planning, and interdisciplinary staff training between agencies to include CBOCs will bring a wealth of information of what CBOCs require to participate effectively in DM. Lessons learned from these partnerships can provide valuable information to facilitate resource allocation for acute care hospitals, which may be burdened with treating patients with minor medical issues when they should be focusing on providing care to those with catastrophic medical conditions.
Acknowledgments
This study and this material is the result of work supported with resources and the use of facilities at the VA Loma Linda Health Care System. Research in this publication was in part supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number P20MD006988.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. McNeill JB, Carafano JJ, Mayer MA, Weitz R. Accepting disaster relief from nations: lessons from Katrina and Gulf oil spill. The Heritage Foundation Website. http://www.heritage.org/research/reports/2011/02/accepting-disaster-relief-from-other-nations-lessons-from-katrina-and-the-gulf-oil-spill. Published February 17, 2011. Accessed July 16, 2015.
2. Haddow GD, Bullock JA. Introduction to Emergency Management. 2nd ed. Burlington, MA: Butterworth-Heinemann; 2006.
3. Institute of Medicine. Medical Surge Capacity: Workshop Summary. Washington, DC: The National Academies Press; 2010.
4. National Voluntary Organizations Active in Disasters. Federal Emergency Management Agency Website. http://www.ready.gov/voluntary-organizations-active-disaster. Updated June 19, 2014. Accessed July 10, 2015.
5. What is the role of police, fire and EMS after a natural disaster strikes? Galls Website. http://gallsblog.com/2011/08/29/what-is-the-role-of-police-fire-and-ems-after-a-natural-disaster-strikes. Published August 29, 2011. Accessed July 14, 2015.
6. Hogan DE, Waeckerle JF, Dire DJ, Lillibridge SR. Emergency department impact of the Oklahoma City terrorist bombing. Ann Emerg Med. 1999;34(2):160-167.
7. Carlson JN, Menegazzi JJ, Callaway CW. Magnitude of national ED visits and resource utilization by the uninsured. Am J Emerg Med. 2013;31(4):722-726.
8. Kahan E, Fogelman Y, Kitai E, Vinker S. Patient and family physician p for care and communication in the eventuality of anthrax terrorism. Fam Pract. 2003;20(4):441-442.
9. Chen FM, Hickner J, Fink KS, Galliher JM, Burstin H. On the front lines: family physicians’ preparedness for bioterrorism. J Fam Pract. 2002;51(9):745-750.
10. Wood K. Community health centers: the untapped resource for public health and medical preparedness. Homeland Secur Aff. 2009;5(8):113.
11. Koenig KL. Homeland security and public health: role of the Department of Veterans Affairs, the US Department of Homeland Security, and implications for the public health community. Prehosp Disaster Med. 2003;18(4):327-333.
12. Panangala SV, Mendez BHP. Veterans Health Administration: Community-Based Outpatient Clinics. Washington, DC: Library of Congress, Congressional Research Service; 2010.
13. Tashakkori A, Teddlie C, eds. Handbook of Mixed Methods in Social & Behavioral Research. Thousand Oaks, CA: Sage Publications, Inc.; 2003.
14. Barnett DJ, Balicer RD, Blodgett DW, et al. Applying risk perception theory to public health workforce preparedness training. J Public Health Manag Pract. 2005;Suppl:33-37.
15. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
Recently, the U.S. Department of Homeland Security redefined disasters into 4 types: natural hazards, societal hazards, technologic hazards, and terrorism. The incidence of manmade and natural disasters is on the rise in intensity and frequency globally. Recent events such as tornadoes and hurricanes in the southeastern U.S., tsunamis in Japan, earthquakes in Haiti, wild fires, heat waves, and terrorist attacks like that of September 11, 2001, underscore the urgency of developing and maintaining solid local public health disaster response plans to minimize mortality and morbidity.
The 2010 BP oil spill in the Gulf of Mexico, the largest in history, hurricane Katrina, and the lingering impact of hurricane Sandy on the East Coast further raise concerns about our communities’ ability to handle disasters, especially in the early hours after events, when federally coordinated help is being organized and not yet fully available locally or from other nations.1 The recent fertilizer plant explosion in West Texas, the 2013 Boston marathon bombing, and the Newtown, Connecticut, massacre remind us of the unpredictable nature of both manmade and natural disasters.
Coordinated Response
Regardless of its origin, residents expect a coordinated local response during an emergency, and it is important that government agencies meet this expectation. Fulfilling these expectations, however, takes many partners, and it is important to have a clear idea of who is involved in emergency preparedness (EP) and the response of each partner’s role.
Role of Government
Federal, state, and local governments have a critical role in emergency management (EM). When state government, local government, or an individual entity is overwhelmed with a disaster, the role of the Federal Emergency Management Agency is to provide assistance and resources to cope with the emergency.2 Private industry and traditional disaster relief agencies, such as the American Red Cross and the Adventist Development and Relief Agency, are also involved in response efforts. Recent examples have shown that these partnerships are often overwhelmed with the needs of large regions experiencing limited resources. Therefore, hospitals and local public health departments frequently must carry much of the immediate burden of stabilizing communities and coordinating response with government agencies and local partners.3
Role of Public Health and the CDC
Federal agencies and local public health departments have been given critical roles in planning and responding to disasters. In particular, the PHS focuses on population care and shapes how public health entities should respond to mass casualty events and pandemics, including local response coordination. The CDC is primarily responsible for assisting state and local governments with disaster response and recovery after a large-scale public health emergency.3 The CDC works closely with local public health departments in decision making; tracking the source, spread, and severity of health threats; assessing impacts; educating the public on how to safeguard their health; and implementing measures to protect the public. During a large-scale health emergency, the CDC also maintains and provides resources through the maintenance and distribution of the nation’s Strategic National Stockpile of medications and supplies that may be needed during events such as the recent 2009 H1N1 influenza outbreak or other public health emergencies.3
Role of Local Businesses and Professional Institutions
Nationally, businesses and professional institutions are coming together and organizing in such a way that places them as part of the solution. More specifically, the National Voluntary Organizations Active in Disaster and Community Organizations Active in Disaster have grown exponentially since September 11, 2001.4 These efforts include but are not limited to development of EP plans and the subsequent sharing of those plans, sharing of key assets critical to response activities, development of a community key asset database, and training/exercise participation.
Role of Hospitals
The Hospital Preparedness Program was developed to prepare the nation’s health care system to respond appropriately to mass casualty incidents, whether due to bioterrorism, natural disaster, or other public health emergencies. Health care systems must be able to develop a disaster medical capability that is rapid, flexible, sustainable, integrated, coordinated, and capable of providing appropriate care in the most ethical manner with the resources and capabilities it has at its disposal.3 Although involved as first responders, traditionally, medical care systems, hospitals, physicians, and pharmacists are faced with the dual task of individual patient care and are thus more limited as partners in an overall local response system.
Also vital to this discussion is the reality that hospital emergency departments (EDs) already routinely operate at or above capacity, limiting their ability to prepare for mass casualties due to a public health disaster. Hospitals continue to divert more than half a million ambulances per year due to ED overcrowding.3 How they could step up in a true emergency situation is questionable at best.
Role of First Responders
Individuals who respond immediately are referred to as first responders. First responders come in 2 archetypes: those who are there purely based on unexpected circumstances and take action and those who are trained first responders, such as firefighters, police officers, and emergency medical technicians (EMTs). These first responders are trained to partner with one another. Firefighters primarily handle fire rescue as well as assessing the extent of potential damage to the area. Law enforcement’s responsibility is to restore order after an emergency, whether it is a natural disaster, community disturbance, or outbreak of hazardous chemicals. An EMT’s role is to attend to the immediate medical care of patients who have been injured or become ill during the emergency.5
Related: Disaster Preparedness for Veterans With Dementia and Their Caregivers
There are occasions where other potential incident responders, such as health care professionals, can play a key role and yet are not integrated into the emergency response. The VHA needs to focus on this facet in order to more effectively respond to events that threaten lives, property, and current infrastructure of the veterans it serves.
Role of CBOCs and Private Physician Practices
Community-based outpatient clinics (CBOCs), including outpatient community health centers and private physician practices (PPPs), maintain and improve routine community health but are rarely involved in routine planning for disasters. They are, therefore, typically not open for business or may have limited hours as they recover from the event. This results in patients who do not have access to their primary care providers (PCPs) turning to EDs, which are already at capacity. As a result, in a disaster the costly and overburdened ED functions as the PCP site for even larger populations affected by a disaster, including those who are uninsured.6,7
Kahan and colleagues reported that two-thirds of patients preferred their family doctor or health care authorities as their first choice for care instead of receiving care in the ED.8 Researchers found that 89% of physicians in private practice felt it was their responsibility to treat, for example, patients infected with anthrax.8 Some argue that if PCPs are included in planning and appropriately trained in disaster preparedness, their attitudes and willingness to participate in emergency services would follow.9
Given the many challenges to disaster preparedness, CBOCs could be a critical partner in EM, and interest continues to grow to explore that role. Health professionals in CBOCs who are trained in disaster management (DM) could become active participants in early intervention to initiate the treatment of patients in rescue efforts during a disaster.10 For instance, a CBOC could triage patients in a postdisaster situation, thus limiting the burden on hospital EDs by evaluating populations at risk and providing them with important information when communication is difficult.
This already existing network of community-based triage stations would offer natural locations to assess the health needs of the population and determine their level of appropriate medical care. Additionally, these clinics can ensure continuation of basic services after initial medical care has been completed in the hospital setting.10 Because clinics have not been included in coordinated DM, there is scant literature that addresses their potential role in disaster response. Community-based outpatient clinics and PPPs are untapped resources; however, it is unknown whether medical staff in these medical clinics have the interest, training, knowledge, skills, and resources in DM or whether barriers to providing safe care can be overcome.10
Case Study
The VHA is the largest integrated health care system in the U.S. It is mandated to serve as a backup to the DoD during disasters, and VHA CBOCs can play an important role.11,12 The CBOCs are staffed with a medical director, nurse manager, and other clinical and support staff. As a study population, CBOCs are well suited to examine and explore staff attitudes and roles in DM. To date, no research reports have been found studying EP in CBOCs.
The purpose of this study was to learn how to best integrate the CBOCs into disaster response. This qualitative study aimed to answer 3 questions: (1) How do VA clinic personnel perceive their personal and their clinic’s risk, level of preparedness, role, and knowledge for an active response in a disaster; (2) What do VA clinic personnel perceive they need in order to function in a disaster; and (3) What resources are necessary for clinic staff to function competently in a disaster?
Methods
In this qualitative study, in-depth semistructured key informant (KI) interviews (N = 3) and focus group discussions (N = 20) guided by risk perception theory and the Andersen Behavioral Model of Health Services Use were conducted and analyzed using grounded theory methods to contextualize the potential of local clinics in disaster response.13-15 To optimize breadth of viewpoints on this issue, participants were selected by theoretical sampling methods to explore perceptions of leadership and line staff.
Study Location
Health care providers and support staff from 3 southern California CBOCs that are contracted by the local VA to provide primary care services (ie, internal medicine, geriatrics, women’s health, mental health, and some specialty care services) to veterans were recruited for this study. The CBOCs are generally connected with a VHA local hospital in their region, offer services 5 days a week, and are closed on weekends and federal holidays. Some VA CBOCs participate in telehealth remote services connected to their regional hospital to help manage their patient populations. The CBOCs are managed by a medical director and a clinic manager and report to their respective VISN, and each VISN reports to the VHA Central Office in Washington, DC.13,15 The CBOC staff includes physicians, nurse practitioners, physician assistants, registered nurses (RNs), licensed vocational nurses (LVNs), medical assistants, front office staff, social workers, case managers, counselors, pharmacists, and nonclinical staff.
In this case, the CBOCs are contracted by Loma Linda University Health to manage care of the veterans and agree to care for nonveterans in a disaster. The CBOCs contracted or not all fall under the criteria as set forth in VHA Handbook 1006.1. This handbook criteria indicate that CBOCs must maintain appropriate emergency response capability. Additionally, VHA Handbook 0320.1 states that the CBOC is responsible for developing, implementing, evaluating, and improving a CBOC Comprehensive Emergency Management Program (CEMP) and for participating in the VAMC Emergency Management Committee. The scope of the VISN-wide CEMP integrates VAMC and VISN EM programs to coordinate and enhance operations during planned and unplanned events.
Study Design and Sample
After receiving institutional review board approval, 3 in-depth semi-structured clinic leadership KI interviews and 3 clinic staff (RNs, LVNs, health technicians, and nursing assistants) focus group discussions (N = 20, 1 per CBOC) to follow up on information gleaned from the analyses of the initial KIs were conducted. To provide continuity, all were conducted by the same trained facilitator who used a semistructured KI outline with questions and probes based on the guiding study framework.
Data Collection and Content Analysis
Interviews and focus group discussions were audio recorded and transcribed verbatim and then analyzed using grounded theory methods. Line-by-line coding was done to develop an initial inductive codebook, which was then organized into final codes. Once the codebook was developed, it was applied to all transcripts.
Related: Pre-Storm Dialysis Saves Lives
Transcripts and resulting codes were reviewed 3 times by independent reviewers to validate data, ensure accuracy, and delete any information that might identify participants. Pseudonyms were used to represent the participants by perspective (eg, nurse, MD) to avoid confusion in data analysis. A 4-stage data analysis approach was used: (1) immersion in the raw data by listening to tapes and reading manuscripts and notes in order to list key ideas and recurrent themes using a constant comparison method; (2) indexing by applying the thematic framework systematically to the data using and seeking new, unanticipated emerging codes; (3) arranging the data in codes and concepts/themes that represent the thematic framework of EP in clinics; (4) identifying a thematic framework for EP using codes that identified key issues, concepts, and themes that can be referenced and derived from the text.
Results
The Table describes the 4 primary emerging themes and corresponding quotes: (1) EP barriers, including lack of direction, training, and tools, which would result in negative outcomes; (2) perceived personal and clinic risk for a disaster, including negative outcomes and personal family safety; (3) perceptions of roles and responsibilities in EP, including intent to participate in DM at various staffing levels as well as patient expectations for care; and (4) existing resources that influence EP and the ability to survive a disaster collectively.
Emergency preparedness barriers. Although most respondents realized their potentially critical role in an emergency, they expressed recurrent barrier themes centered on their perceived lack of training, lack of tools to function, and lack of direction to be effective in a disaster response. Lack of knowledge of EP was identified as a great need by multiple participants. One participant stated, “Lack of information is so destructive. If you don’t know how to keep yourself from those things you don’t know…such as in a situation that’s going to be tragic, it is because of a lack of information or a lack of training. And I see that so many times…Mandate that we do our classes, so we know what we’re doing.” Another stated in reference to lack of skills, “I haven’t experienced any drills or anything like that. So I know what is going to happen here.”
Lack of abilities to communicate with key DM players also were identified. For example, “Downed power lines may result in no telephone connection to communicate next steps for critical issues, such as if evacuation of the clinic is required.” Another respondent indicated, “We need backup communication...devices, wind-up radios, or whatever.”
Lack of a clear disaster plan was also identified. Questions arose centered on details—how to actually implement a clinic response plan, including concerns that there were none, as the respondents “had not seen the plan in a couple of years” and were not sure who really was in charge of giving directions. Lack of community/organizational support voiced included aspects such as interdepartmental, facility, and community resource connectedness. There was acknowledgement that department assets should be clearly identified so that resource sharing might be used as part of the plan.
Last, regarding lack of resources, one participant said, “We don’t have the resources. We don’t have gurneys. We don’t have enough wheel chairs….We don’t have a crash cart. We don’t have the triage tarps or whatever for the triage of people; we don’t have any supplies to supply the energy room for diabetics, like what they have in the ER.”
Perceived personal and clinic risk for a disaster. Participants stated they felt at risk for natural disasters, including fire, floods, and earthquakes, but expressed concerns and even more fears about how they would handle a response to bombings, spills of hazardous materials, airplane accidents, and gunfire, which also qualify as disasters but are much harder to prepare for, because they could be so varied. One participated stated, “They are so unpredictable whether it is an earthquake or a fire…they are unpredictable….We see planes that fly close to our window and we wonder about the possibility of a crash—you never know.”
Many staff members expressed fear of what these disasters would mean to them in the clinic and to their patients. Another comment shared was, “I don’t think anybody really thinks about this kind of stuff until it happens and then it is too late…If we had just done this or that or knew how to do this or that then…” The biggest fear expressed was that of a massive earthquake in which there would be power outages and resulting fires, blocked building exits, and no way to get to evacuation areas. Fears expressed included working with people who are dying and trying to get the patients down the stairs and out of the disaster area.
Personal safety in a disaster was also a concern; a nurse stated, “Your personal safety is a priority. Yourself, that is first, if you are not safe, you can’t do any good to anyone else.” Another shared concern was the safety of family members during a disaster and conflicting obligations between duties at work and protecting family members. Participants felt they would want to be at home with their families.
Perceptions of roles and responsibilities in EP. Supervisors of the clinics shared that their primary responsibility is to the staff and their current patients; ensuring their safety was a top priority. Their knowledge, skills, and available resources were crucial to their duties, including establishing methods of communication outside the clinic for advice and direction, such as notifying the power company and other outside agencies of the condition of the clinic. They felt that their duties included making sure generators were working, ensuring telephones and lighting were available, and advising staff when to leave the building. One manager stated that more EP discussions need to happen in order to determine how to react: “...in event of a disaster it is important to control patient flow, staffing the clinic appropriately and managing the employees.” They felt a need to help empower their staff by making sure staff were trained in EP tasks and that they could complete the tasks they were required to perform.
Staff consistently reported that the doctors were in charge of providing direction concerning activities and care of the patients. However, most were able to identify their own role in helping preserve lives and keeping the patients and other staff safe. One nurse stated, “My job would be to evacuate the physicians’ offices, to make sure they are aware of the disaster, get them out safely, put an X on their door, keep the patients calm and guide them out to the designated area, then look out for medics or other help so that they would be directed to the correct locations.” Another staff nurse stated, “My role is to check the bathrooms and then under the direction of the physician assist in the care of patient injuries.”
When asked about the expectations of patients for care during a disaster, staff consistently stated that patients and their families would want to get care and direction from clinic staff who knew them instead of going to the hospital for care. Staff anticipated that patients would be calling the clinic first to discuss their medical problems. One stated, “The veterans would head to us…. We can’t turn them away.” Some staff indicated that some patients might have to go to the ED for care instead of coming to the clinic, because the clinic may not be equipped to respond, noting that “we have to remind [the patients] that in our clinic we have minimal abilities.”
Existing resources. Consistently, the respondents verbalized the importance of acquiring knowledge and skills and using available resources in their disaster plan. They felt that training was critical and that it needed to be simple and uncomplicated. Many felt that they did not have sufficient drills to maintain their knowledge and skills for all types of events. One nursing assistant stated he had extensive training in the military in DM, but clinics did not have sufficient training and were not prepared to handle multiple casualties. Others stated that it would be important for training to be “second nature” so they would not have to think much about it, with everyone pulling together and performing tasks seamlessly. However, some stated that they did not know what to do in an emergency.
Critical resources noted were access to emergency power sources, transistor radios, telephone and communication, 911 services, backup phone services, computers, and text pagers and cell phones so that connections could be made outside the clinic setting. Other critical resources needed included medical supplies and access to food for 1 week.
Finally, teamwork was identified as a critical factor for success. One example involved the clinic responding to a severe snowstorm; the medical director, lead nurse, and support staff agreed to remain on site to assist with any patients who needed help. “We shared our 4-wheel drive trucks to get around, and others called patients, advising them of storm conditions and what to do to maintain care at home and canceled appointments scheduled for that day.” They were very proud of the way they had pooled their resources to support each other and their patients.
Based on these emerging themes and the inquiry guiding theories, a theoretical framework was proposed on how contributing factors influenced the process by which CBOC staff viewed their roles and the likelihood that they would participate in a disaster plan (Figure). The framework suggests that personal risks and perceived personal and clinic readiness to respond to an emergency were critical barriers to staff willingness to get involved in preparedness, whereas they saw the provision of training and resources as necessary to increase their resilience and ability to function in a disaster.
Clearly addressing barriers through training, planning, ensuring that resources functioned effectively in a disaster, and clarifying roles and responsibilities, combined with promoting personal and clinic readiness facilitated staff EP participation.
Discussion
This qualitative study explored issues surrounding the role of CBOCs in EP and how risk perception and enabling factors contributed to staff intent to participate in DM. As in many qualitative studies, findings were somewhat limited by an overall small sample size (N = 23) across 3 CBOCs in southern California. However, given the lack of available literature, the authors believe that this study helped provide critical insight into CBOC clinic staff’s willingness and readiness to be active in disaster response. The study clearly points to clinic staff’s openness to actively take part in regional disaster response and calls for better and more standardized approaches to EP and DM planning that include local CBOCs. The authors identified factors that contribute to staff intent to participate in DM and the need to reduce barriers that hinder participation.
In general, clinic staff who reported feeling inadequately prepared for disasters (ie, felt more vulnerable) and staff with firsthand disaster experience were more inclined to prepare than were those without experience. Without clearly spelled-out expectations, staff tend to depend and wait on others to lead in a disaster. They noted a desire for better preparation and thus, clarity of roles, need for a reliable method of communication with the outside world during a disaster, and the required equipment and supplies for self-care or care of the patients for ≥ 3 days post disaster. Some indicated that they did not have the resources to provide medical care on the scale that may be required.
Many did not have a clear understanding of an all-hazard approach plan and had not been involved in hazard assessments. Already tightly staffed for personal health care delivery, staff spent minimal time and energy thinking about the risk of a disaster or preparing for one. However, there seemed to be a direct relationship between the attitude of the supervisor and the attitudes of clinic staff to EP. Although these qualitative results are encouraging and point to these clinics as an important undertapped resource for EP, further quantitative studies should expand this inquiry.
Lessons learned from this study include the need to expand qualitative data collection to include a larger sample size to retrieve information that would contribute to a better understanding of how staff view their roles in DM. There are 152 VAMCs and hundreds of associated CBOCs that should be queried as to their EM readiness. Also, replicating this study in non-VHA clinics, such as private CBOCs and PPPs, might bring greater insight into what is needed to involve them in DM plans. Finally, future studies should determine clearer criteria when care can be provided at a clinic and when it would be appropriate for the patient to report at their local ED.
Conclusions and Recommendations
Given the VHA EP mandate, the authors recommend the following steps to address barriers identified in this study: (1) Develop a more structured approach to DM in a CBOC setting to provide staff with a clear understanding of their roles and responsibilities; (2) Conduct a comprehensive assessment of each clinic to determine staff knowledge, skills, and resources required to provide EP and institute a DM training curriculum; (3) Provide clinic leadership with direction on developing a disaster plan as well as how to partner with their primary and local VA health care system, especially onsite physicians, to provide effective DM leadership; (4) Recruit staff into routine drills for natural disasters and expand to an all-hazard approach to manmade disasters to identify gaps in delivering DM in a disaster; (5) Facilitate partnerships and a standardized approach to DM between CBOCs within the VISN by scheduling routine video and teleconferencing, live meetings, and webinars so that procedures and language are clearly understood and communicated between facilities; and (6) Identify key barriers to clinic preparedness by assessing EP elements through mock disaster drills and offer solutions to fill DM gaps.
The authors also recommend that CBOCs should be included in community DM and EP plans in order to understand how to integrate resources in a disaster. Networking, planning, and interdisciplinary staff training between agencies to include CBOCs will bring a wealth of information of what CBOCs require to participate effectively in DM. Lessons learned from these partnerships can provide valuable information to facilitate resource allocation for acute care hospitals, which may be burdened with treating patients with minor medical issues when they should be focusing on providing care to those with catastrophic medical conditions.
Acknowledgments
This study and this material is the result of work supported with resources and the use of facilities at the VA Loma Linda Health Care System. Research in this publication was in part supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number P20MD006988.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Recently, the U.S. Department of Homeland Security redefined disasters into 4 types: natural hazards, societal hazards, technologic hazards, and terrorism. The incidence of manmade and natural disasters is on the rise in intensity and frequency globally. Recent events such as tornadoes and hurricanes in the southeastern U.S., tsunamis in Japan, earthquakes in Haiti, wild fires, heat waves, and terrorist attacks like that of September 11, 2001, underscore the urgency of developing and maintaining solid local public health disaster response plans to minimize mortality and morbidity.
The 2010 BP oil spill in the Gulf of Mexico, the largest in history, hurricane Katrina, and the lingering impact of hurricane Sandy on the East Coast further raise concerns about our communities’ ability to handle disasters, especially in the early hours after events, when federally coordinated help is being organized and not yet fully available locally or from other nations.1 The recent fertilizer plant explosion in West Texas, the 2013 Boston marathon bombing, and the Newtown, Connecticut, massacre remind us of the unpredictable nature of both manmade and natural disasters.
Coordinated Response
Regardless of its origin, residents expect a coordinated local response during an emergency, and it is important that government agencies meet this expectation. Fulfilling these expectations, however, takes many partners, and it is important to have a clear idea of who is involved in emergency preparedness (EP) and the response of each partner’s role.
Role of Government
Federal, state, and local governments have a critical role in emergency management (EM). When state government, local government, or an individual entity is overwhelmed with a disaster, the role of the Federal Emergency Management Agency is to provide assistance and resources to cope with the emergency.2 Private industry and traditional disaster relief agencies, such as the American Red Cross and the Adventist Development and Relief Agency, are also involved in response efforts. Recent examples have shown that these partnerships are often overwhelmed with the needs of large regions experiencing limited resources. Therefore, hospitals and local public health departments frequently must carry much of the immediate burden of stabilizing communities and coordinating response with government agencies and local partners.3
Role of Public Health and the CDC
Federal agencies and local public health departments have been given critical roles in planning and responding to disasters. In particular, the PHS focuses on population care and shapes how public health entities should respond to mass casualty events and pandemics, including local response coordination. The CDC is primarily responsible for assisting state and local governments with disaster response and recovery after a large-scale public health emergency.3 The CDC works closely with local public health departments in decision making; tracking the source, spread, and severity of health threats; assessing impacts; educating the public on how to safeguard their health; and implementing measures to protect the public. During a large-scale health emergency, the CDC also maintains and provides resources through the maintenance and distribution of the nation’s Strategic National Stockpile of medications and supplies that may be needed during events such as the recent 2009 H1N1 influenza outbreak or other public health emergencies.3
Role of Local Businesses and Professional Institutions
Nationally, businesses and professional institutions are coming together and organizing in such a way that places them as part of the solution. More specifically, the National Voluntary Organizations Active in Disaster and Community Organizations Active in Disaster have grown exponentially since September 11, 2001.4 These efforts include but are not limited to development of EP plans and the subsequent sharing of those plans, sharing of key assets critical to response activities, development of a community key asset database, and training/exercise participation.
Role of Hospitals
The Hospital Preparedness Program was developed to prepare the nation’s health care system to respond appropriately to mass casualty incidents, whether due to bioterrorism, natural disaster, or other public health emergencies. Health care systems must be able to develop a disaster medical capability that is rapid, flexible, sustainable, integrated, coordinated, and capable of providing appropriate care in the most ethical manner with the resources and capabilities it has at its disposal.3 Although involved as first responders, traditionally, medical care systems, hospitals, physicians, and pharmacists are faced with the dual task of individual patient care and are thus more limited as partners in an overall local response system.
Also vital to this discussion is the reality that hospital emergency departments (EDs) already routinely operate at or above capacity, limiting their ability to prepare for mass casualties due to a public health disaster. Hospitals continue to divert more than half a million ambulances per year due to ED overcrowding.3 How they could step up in a true emergency situation is questionable at best.
Role of First Responders
Individuals who respond immediately are referred to as first responders. First responders come in 2 archetypes: those who are there purely based on unexpected circumstances and take action and those who are trained first responders, such as firefighters, police officers, and emergency medical technicians (EMTs). These first responders are trained to partner with one another. Firefighters primarily handle fire rescue as well as assessing the extent of potential damage to the area. Law enforcement’s responsibility is to restore order after an emergency, whether it is a natural disaster, community disturbance, or outbreak of hazardous chemicals. An EMT’s role is to attend to the immediate medical care of patients who have been injured or become ill during the emergency.5
Related: Disaster Preparedness for Veterans With Dementia and Their Caregivers
There are occasions where other potential incident responders, such as health care professionals, can play a key role and yet are not integrated into the emergency response. The VHA needs to focus on this facet in order to more effectively respond to events that threaten lives, property, and current infrastructure of the veterans it serves.
Role of CBOCs and Private Physician Practices
Community-based outpatient clinics (CBOCs), including outpatient community health centers and private physician practices (PPPs), maintain and improve routine community health but are rarely involved in routine planning for disasters. They are, therefore, typically not open for business or may have limited hours as they recover from the event. This results in patients who do not have access to their primary care providers (PCPs) turning to EDs, which are already at capacity. As a result, in a disaster the costly and overburdened ED functions as the PCP site for even larger populations affected by a disaster, including those who are uninsured.6,7
Kahan and colleagues reported that two-thirds of patients preferred their family doctor or health care authorities as their first choice for care instead of receiving care in the ED.8 Researchers found that 89% of physicians in private practice felt it was their responsibility to treat, for example, patients infected with anthrax.8 Some argue that if PCPs are included in planning and appropriately trained in disaster preparedness, their attitudes and willingness to participate in emergency services would follow.9
Given the many challenges to disaster preparedness, CBOCs could be a critical partner in EM, and interest continues to grow to explore that role. Health professionals in CBOCs who are trained in disaster management (DM) could become active participants in early intervention to initiate the treatment of patients in rescue efforts during a disaster.10 For instance, a CBOC could triage patients in a postdisaster situation, thus limiting the burden on hospital EDs by evaluating populations at risk and providing them with important information when communication is difficult.
This already existing network of community-based triage stations would offer natural locations to assess the health needs of the population and determine their level of appropriate medical care. Additionally, these clinics can ensure continuation of basic services after initial medical care has been completed in the hospital setting.10 Because clinics have not been included in coordinated DM, there is scant literature that addresses their potential role in disaster response. Community-based outpatient clinics and PPPs are untapped resources; however, it is unknown whether medical staff in these medical clinics have the interest, training, knowledge, skills, and resources in DM or whether barriers to providing safe care can be overcome.10
Case Study
The VHA is the largest integrated health care system in the U.S. It is mandated to serve as a backup to the DoD during disasters, and VHA CBOCs can play an important role.11,12 The CBOCs are staffed with a medical director, nurse manager, and other clinical and support staff. As a study population, CBOCs are well suited to examine and explore staff attitudes and roles in DM. To date, no research reports have been found studying EP in CBOCs.
The purpose of this study was to learn how to best integrate the CBOCs into disaster response. This qualitative study aimed to answer 3 questions: (1) How do VA clinic personnel perceive their personal and their clinic’s risk, level of preparedness, role, and knowledge for an active response in a disaster; (2) What do VA clinic personnel perceive they need in order to function in a disaster; and (3) What resources are necessary for clinic staff to function competently in a disaster?
Methods
In this qualitative study, in-depth semistructured key informant (KI) interviews (N = 3) and focus group discussions (N = 20) guided by risk perception theory and the Andersen Behavioral Model of Health Services Use were conducted and analyzed using grounded theory methods to contextualize the potential of local clinics in disaster response.13-15 To optimize breadth of viewpoints on this issue, participants were selected by theoretical sampling methods to explore perceptions of leadership and line staff.
Study Location
Health care providers and support staff from 3 southern California CBOCs that are contracted by the local VA to provide primary care services (ie, internal medicine, geriatrics, women’s health, mental health, and some specialty care services) to veterans were recruited for this study. The CBOCs are generally connected with a VHA local hospital in their region, offer services 5 days a week, and are closed on weekends and federal holidays. Some VA CBOCs participate in telehealth remote services connected to their regional hospital to help manage their patient populations. The CBOCs are managed by a medical director and a clinic manager and report to their respective VISN, and each VISN reports to the VHA Central Office in Washington, DC.13,15 The CBOC staff includes physicians, nurse practitioners, physician assistants, registered nurses (RNs), licensed vocational nurses (LVNs), medical assistants, front office staff, social workers, case managers, counselors, pharmacists, and nonclinical staff.
In this case, the CBOCs are contracted by Loma Linda University Health to manage care of the veterans and agree to care for nonveterans in a disaster. The CBOCs contracted or not all fall under the criteria as set forth in VHA Handbook 1006.1. This handbook criteria indicate that CBOCs must maintain appropriate emergency response capability. Additionally, VHA Handbook 0320.1 states that the CBOC is responsible for developing, implementing, evaluating, and improving a CBOC Comprehensive Emergency Management Program (CEMP) and for participating in the VAMC Emergency Management Committee. The scope of the VISN-wide CEMP integrates VAMC and VISN EM programs to coordinate and enhance operations during planned and unplanned events.
Study Design and Sample
After receiving institutional review board approval, 3 in-depth semi-structured clinic leadership KI interviews and 3 clinic staff (RNs, LVNs, health technicians, and nursing assistants) focus group discussions (N = 20, 1 per CBOC) to follow up on information gleaned from the analyses of the initial KIs were conducted. To provide continuity, all were conducted by the same trained facilitator who used a semistructured KI outline with questions and probes based on the guiding study framework.
Data Collection and Content Analysis
Interviews and focus group discussions were audio recorded and transcribed verbatim and then analyzed using grounded theory methods. Line-by-line coding was done to develop an initial inductive codebook, which was then organized into final codes. Once the codebook was developed, it was applied to all transcripts.
Related: Pre-Storm Dialysis Saves Lives
Transcripts and resulting codes were reviewed 3 times by independent reviewers to validate data, ensure accuracy, and delete any information that might identify participants. Pseudonyms were used to represent the participants by perspective (eg, nurse, MD) to avoid confusion in data analysis. A 4-stage data analysis approach was used: (1) immersion in the raw data by listening to tapes and reading manuscripts and notes in order to list key ideas and recurrent themes using a constant comparison method; (2) indexing by applying the thematic framework systematically to the data using and seeking new, unanticipated emerging codes; (3) arranging the data in codes and concepts/themes that represent the thematic framework of EP in clinics; (4) identifying a thematic framework for EP using codes that identified key issues, concepts, and themes that can be referenced and derived from the text.
Results
The Table describes the 4 primary emerging themes and corresponding quotes: (1) EP barriers, including lack of direction, training, and tools, which would result in negative outcomes; (2) perceived personal and clinic risk for a disaster, including negative outcomes and personal family safety; (3) perceptions of roles and responsibilities in EP, including intent to participate in DM at various staffing levels as well as patient expectations for care; and (4) existing resources that influence EP and the ability to survive a disaster collectively.
Emergency preparedness barriers. Although most respondents realized their potentially critical role in an emergency, they expressed recurrent barrier themes centered on their perceived lack of training, lack of tools to function, and lack of direction to be effective in a disaster response. Lack of knowledge of EP was identified as a great need by multiple participants. One participant stated, “Lack of information is so destructive. If you don’t know how to keep yourself from those things you don’t know…such as in a situation that’s going to be tragic, it is because of a lack of information or a lack of training. And I see that so many times…Mandate that we do our classes, so we know what we’re doing.” Another stated in reference to lack of skills, “I haven’t experienced any drills or anything like that. So I know what is going to happen here.”
Lack of abilities to communicate with key DM players also were identified. For example, “Downed power lines may result in no telephone connection to communicate next steps for critical issues, such as if evacuation of the clinic is required.” Another respondent indicated, “We need backup communication...devices, wind-up radios, or whatever.”
Lack of a clear disaster plan was also identified. Questions arose centered on details—how to actually implement a clinic response plan, including concerns that there were none, as the respondents “had not seen the plan in a couple of years” and were not sure who really was in charge of giving directions. Lack of community/organizational support voiced included aspects such as interdepartmental, facility, and community resource connectedness. There was acknowledgement that department assets should be clearly identified so that resource sharing might be used as part of the plan.
Last, regarding lack of resources, one participant said, “We don’t have the resources. We don’t have gurneys. We don’t have enough wheel chairs….We don’t have a crash cart. We don’t have the triage tarps or whatever for the triage of people; we don’t have any supplies to supply the energy room for diabetics, like what they have in the ER.”
Perceived personal and clinic risk for a disaster. Participants stated they felt at risk for natural disasters, including fire, floods, and earthquakes, but expressed concerns and even more fears about how they would handle a response to bombings, spills of hazardous materials, airplane accidents, and gunfire, which also qualify as disasters but are much harder to prepare for, because they could be so varied. One participated stated, “They are so unpredictable whether it is an earthquake or a fire…they are unpredictable….We see planes that fly close to our window and we wonder about the possibility of a crash—you never know.”
Many staff members expressed fear of what these disasters would mean to them in the clinic and to their patients. Another comment shared was, “I don’t think anybody really thinks about this kind of stuff until it happens and then it is too late…If we had just done this or that or knew how to do this or that then…” The biggest fear expressed was that of a massive earthquake in which there would be power outages and resulting fires, blocked building exits, and no way to get to evacuation areas. Fears expressed included working with people who are dying and trying to get the patients down the stairs and out of the disaster area.
Personal safety in a disaster was also a concern; a nurse stated, “Your personal safety is a priority. Yourself, that is first, if you are not safe, you can’t do any good to anyone else.” Another shared concern was the safety of family members during a disaster and conflicting obligations between duties at work and protecting family members. Participants felt they would want to be at home with their families.
Perceptions of roles and responsibilities in EP. Supervisors of the clinics shared that their primary responsibility is to the staff and their current patients; ensuring their safety was a top priority. Their knowledge, skills, and available resources were crucial to their duties, including establishing methods of communication outside the clinic for advice and direction, such as notifying the power company and other outside agencies of the condition of the clinic. They felt that their duties included making sure generators were working, ensuring telephones and lighting were available, and advising staff when to leave the building. One manager stated that more EP discussions need to happen in order to determine how to react: “...in event of a disaster it is important to control patient flow, staffing the clinic appropriately and managing the employees.” They felt a need to help empower their staff by making sure staff were trained in EP tasks and that they could complete the tasks they were required to perform.
Staff consistently reported that the doctors were in charge of providing direction concerning activities and care of the patients. However, most were able to identify their own role in helping preserve lives and keeping the patients and other staff safe. One nurse stated, “My job would be to evacuate the physicians’ offices, to make sure they are aware of the disaster, get them out safely, put an X on their door, keep the patients calm and guide them out to the designated area, then look out for medics or other help so that they would be directed to the correct locations.” Another staff nurse stated, “My role is to check the bathrooms and then under the direction of the physician assist in the care of patient injuries.”
When asked about the expectations of patients for care during a disaster, staff consistently stated that patients and their families would want to get care and direction from clinic staff who knew them instead of going to the hospital for care. Staff anticipated that patients would be calling the clinic first to discuss their medical problems. One stated, “The veterans would head to us…. We can’t turn them away.” Some staff indicated that some patients might have to go to the ED for care instead of coming to the clinic, because the clinic may not be equipped to respond, noting that “we have to remind [the patients] that in our clinic we have minimal abilities.”
Existing resources. Consistently, the respondents verbalized the importance of acquiring knowledge and skills and using available resources in their disaster plan. They felt that training was critical and that it needed to be simple and uncomplicated. Many felt that they did not have sufficient drills to maintain their knowledge and skills for all types of events. One nursing assistant stated he had extensive training in the military in DM, but clinics did not have sufficient training and were not prepared to handle multiple casualties. Others stated that it would be important for training to be “second nature” so they would not have to think much about it, with everyone pulling together and performing tasks seamlessly. However, some stated that they did not know what to do in an emergency.
Critical resources noted were access to emergency power sources, transistor radios, telephone and communication, 911 services, backup phone services, computers, and text pagers and cell phones so that connections could be made outside the clinic setting. Other critical resources needed included medical supplies and access to food for 1 week.
Finally, teamwork was identified as a critical factor for success. One example involved the clinic responding to a severe snowstorm; the medical director, lead nurse, and support staff agreed to remain on site to assist with any patients who needed help. “We shared our 4-wheel drive trucks to get around, and others called patients, advising them of storm conditions and what to do to maintain care at home and canceled appointments scheduled for that day.” They were very proud of the way they had pooled their resources to support each other and their patients.
Based on these emerging themes and the inquiry guiding theories, a theoretical framework was proposed on how contributing factors influenced the process by which CBOC staff viewed their roles and the likelihood that they would participate in a disaster plan (Figure). The framework suggests that personal risks and perceived personal and clinic readiness to respond to an emergency were critical barriers to staff willingness to get involved in preparedness, whereas they saw the provision of training and resources as necessary to increase their resilience and ability to function in a disaster.
Clearly addressing barriers through training, planning, ensuring that resources functioned effectively in a disaster, and clarifying roles and responsibilities, combined with promoting personal and clinic readiness facilitated staff EP participation.
Discussion
This qualitative study explored issues surrounding the role of CBOCs in EP and how risk perception and enabling factors contributed to staff intent to participate in DM. As in many qualitative studies, findings were somewhat limited by an overall small sample size (N = 23) across 3 CBOCs in southern California. However, given the lack of available literature, the authors believe that this study helped provide critical insight into CBOC clinic staff’s willingness and readiness to be active in disaster response. The study clearly points to clinic staff’s openness to actively take part in regional disaster response and calls for better and more standardized approaches to EP and DM planning that include local CBOCs. The authors identified factors that contribute to staff intent to participate in DM and the need to reduce barriers that hinder participation.
In general, clinic staff who reported feeling inadequately prepared for disasters (ie, felt more vulnerable) and staff with firsthand disaster experience were more inclined to prepare than were those without experience. Without clearly spelled-out expectations, staff tend to depend and wait on others to lead in a disaster. They noted a desire for better preparation and thus, clarity of roles, need for a reliable method of communication with the outside world during a disaster, and the required equipment and supplies for self-care or care of the patients for ≥ 3 days post disaster. Some indicated that they did not have the resources to provide medical care on the scale that may be required.
Many did not have a clear understanding of an all-hazard approach plan and had not been involved in hazard assessments. Already tightly staffed for personal health care delivery, staff spent minimal time and energy thinking about the risk of a disaster or preparing for one. However, there seemed to be a direct relationship between the attitude of the supervisor and the attitudes of clinic staff to EP. Although these qualitative results are encouraging and point to these clinics as an important undertapped resource for EP, further quantitative studies should expand this inquiry.
Lessons learned from this study include the need to expand qualitative data collection to include a larger sample size to retrieve information that would contribute to a better understanding of how staff view their roles in DM. There are 152 VAMCs and hundreds of associated CBOCs that should be queried as to their EM readiness. Also, replicating this study in non-VHA clinics, such as private CBOCs and PPPs, might bring greater insight into what is needed to involve them in DM plans. Finally, future studies should determine clearer criteria when care can be provided at a clinic and when it would be appropriate for the patient to report at their local ED.
Conclusions and Recommendations
Given the VHA EP mandate, the authors recommend the following steps to address barriers identified in this study: (1) Develop a more structured approach to DM in a CBOC setting to provide staff with a clear understanding of their roles and responsibilities; (2) Conduct a comprehensive assessment of each clinic to determine staff knowledge, skills, and resources required to provide EP and institute a DM training curriculum; (3) Provide clinic leadership with direction on developing a disaster plan as well as how to partner with their primary and local VA health care system, especially onsite physicians, to provide effective DM leadership; (4) Recruit staff into routine drills for natural disasters and expand to an all-hazard approach to manmade disasters to identify gaps in delivering DM in a disaster; (5) Facilitate partnerships and a standardized approach to DM between CBOCs within the VISN by scheduling routine video and teleconferencing, live meetings, and webinars so that procedures and language are clearly understood and communicated between facilities; and (6) Identify key barriers to clinic preparedness by assessing EP elements through mock disaster drills and offer solutions to fill DM gaps.
The authors also recommend that CBOCs should be included in community DM and EP plans in order to understand how to integrate resources in a disaster. Networking, planning, and interdisciplinary staff training between agencies to include CBOCs will bring a wealth of information of what CBOCs require to participate effectively in DM. Lessons learned from these partnerships can provide valuable information to facilitate resource allocation for acute care hospitals, which may be burdened with treating patients with minor medical issues when they should be focusing on providing care to those with catastrophic medical conditions.
Acknowledgments
This study and this material is the result of work supported with resources and the use of facilities at the VA Loma Linda Health Care System. Research in this publication was in part supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number P20MD006988.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. McNeill JB, Carafano JJ, Mayer MA, Weitz R. Accepting disaster relief from nations: lessons from Katrina and Gulf oil spill. The Heritage Foundation Website. http://www.heritage.org/research/reports/2011/02/accepting-disaster-relief-from-other-nations-lessons-from-katrina-and-the-gulf-oil-spill. Published February 17, 2011. Accessed July 16, 2015.
2. Haddow GD, Bullock JA. Introduction to Emergency Management. 2nd ed. Burlington, MA: Butterworth-Heinemann; 2006.
3. Institute of Medicine. Medical Surge Capacity: Workshop Summary. Washington, DC: The National Academies Press; 2010.
4. National Voluntary Organizations Active in Disasters. Federal Emergency Management Agency Website. http://www.ready.gov/voluntary-organizations-active-disaster. Updated June 19, 2014. Accessed July 10, 2015.
5. What is the role of police, fire and EMS after a natural disaster strikes? Galls Website. http://gallsblog.com/2011/08/29/what-is-the-role-of-police-fire-and-ems-after-a-natural-disaster-strikes. Published August 29, 2011. Accessed July 14, 2015.
6. Hogan DE, Waeckerle JF, Dire DJ, Lillibridge SR. Emergency department impact of the Oklahoma City terrorist bombing. Ann Emerg Med. 1999;34(2):160-167.
7. Carlson JN, Menegazzi JJ, Callaway CW. Magnitude of national ED visits and resource utilization by the uninsured. Am J Emerg Med. 2013;31(4):722-726.
8. Kahan E, Fogelman Y, Kitai E, Vinker S. Patient and family physician p for care and communication in the eventuality of anthrax terrorism. Fam Pract. 2003;20(4):441-442.
9. Chen FM, Hickner J, Fink KS, Galliher JM, Burstin H. On the front lines: family physicians’ preparedness for bioterrorism. J Fam Pract. 2002;51(9):745-750.
10. Wood K. Community health centers: the untapped resource for public health and medical preparedness. Homeland Secur Aff. 2009;5(8):113.
11. Koenig KL. Homeland security and public health: role of the Department of Veterans Affairs, the US Department of Homeland Security, and implications for the public health community. Prehosp Disaster Med. 2003;18(4):327-333.
12. Panangala SV, Mendez BHP. Veterans Health Administration: Community-Based Outpatient Clinics. Washington, DC: Library of Congress, Congressional Research Service; 2010.
13. Tashakkori A, Teddlie C, eds. Handbook of Mixed Methods in Social & Behavioral Research. Thousand Oaks, CA: Sage Publications, Inc.; 2003.
14. Barnett DJ, Balicer RD, Blodgett DW, et al. Applying risk perception theory to public health workforce preparedness training. J Public Health Manag Pract. 2005;Suppl:33-37.
15. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
1. McNeill JB, Carafano JJ, Mayer MA, Weitz R. Accepting disaster relief from nations: lessons from Katrina and Gulf oil spill. The Heritage Foundation Website. http://www.heritage.org/research/reports/2011/02/accepting-disaster-relief-from-other-nations-lessons-from-katrina-and-the-gulf-oil-spill. Published February 17, 2011. Accessed July 16, 2015.
2. Haddow GD, Bullock JA. Introduction to Emergency Management. 2nd ed. Burlington, MA: Butterworth-Heinemann; 2006.
3. Institute of Medicine. Medical Surge Capacity: Workshop Summary. Washington, DC: The National Academies Press; 2010.
4. National Voluntary Organizations Active in Disasters. Federal Emergency Management Agency Website. http://www.ready.gov/voluntary-organizations-active-disaster. Updated June 19, 2014. Accessed July 10, 2015.
5. What is the role of police, fire and EMS after a natural disaster strikes? Galls Website. http://gallsblog.com/2011/08/29/what-is-the-role-of-police-fire-and-ems-after-a-natural-disaster-strikes. Published August 29, 2011. Accessed July 14, 2015.
6. Hogan DE, Waeckerle JF, Dire DJ, Lillibridge SR. Emergency department impact of the Oklahoma City terrorist bombing. Ann Emerg Med. 1999;34(2):160-167.
7. Carlson JN, Menegazzi JJ, Callaway CW. Magnitude of national ED visits and resource utilization by the uninsured. Am J Emerg Med. 2013;31(4):722-726.
8. Kahan E, Fogelman Y, Kitai E, Vinker S. Patient and family physician p for care and communication in the eventuality of anthrax terrorism. Fam Pract. 2003;20(4):441-442.
9. Chen FM, Hickner J, Fink KS, Galliher JM, Burstin H. On the front lines: family physicians’ preparedness for bioterrorism. J Fam Pract. 2002;51(9):745-750.
10. Wood K. Community health centers: the untapped resource for public health and medical preparedness. Homeland Secur Aff. 2009;5(8):113.
11. Koenig KL. Homeland security and public health: role of the Department of Veterans Affairs, the US Department of Homeland Security, and implications for the public health community. Prehosp Disaster Med. 2003;18(4):327-333.
12. Panangala SV, Mendez BHP. Veterans Health Administration: Community-Based Outpatient Clinics. Washington, DC: Library of Congress, Congressional Research Service; 2010.
13. Tashakkori A, Teddlie C, eds. Handbook of Mixed Methods in Social & Behavioral Research. Thousand Oaks, CA: Sage Publications, Inc.; 2003.
14. Barnett DJ, Balicer RD, Blodgett DW, et al. Applying risk perception theory to public health workforce preparedness training. J Public Health Manag Pract. 2005;Suppl:33-37.
15. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.