User login
The “Things We Do for No Reason” (TWDFNR) series reviews practices that have become common parts of hospital care but that may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Oral anticoagulation (OAC) is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for primary and secondary thromboembolism prevention. When patients require surgery or an invasive procedure, “bridging” anticoagulants (eg, enoxaparin) are commonly administered during the period of OAC interruption to reduce thromboembolic risk. This practice stems from small observational studies and expert opinion, which influenced several clinical guidelines despite the lack of high-quality evidence. Although prospective randomized trials of periprocedural bridging in patients with VTE and MHVs are lacking, available evidence is consistent with findings from the BRIDGE trial, which guides the following general recommendations: (1) avoid unnecessary periprocedural interruptions of OAC, especially for low bleeding risk procedures; (2) avoid the administration of periprocedural bridging anticoagulation in patients with low to moderate thromboembolic risk; (3) in patients with high thromboembolic risk, individually assess the patient-specific and procedure-specific bleeding risks versus thromboembolic risks.
A 75-year-old man with a history of hypertension, diabetes mellitus, and atrial fibrillation is admitted for surgical repair of a comminuted intertrochanteric left hip fracture. He suffered a mechanical ground-level fall without loss of consciousness. At baseline, he denies any chest pain, dyspnea on exertion, or recent change in his exercise tolerance. A physical examination is notable for stable vital signs, irregular cardiac rhythm, and a shortened and externally rotated left lower extremity with exquisite tenderness to palpation and range of motion. The patient is taking warfarin for stroke prophylaxis based on a CHA2DS2VaSc score of 4 points. The international normalized ratio (INR) is 1.9 upon admission, and surgery is planned within 48 hours, once the patient is “medically cleared.” Will this patient benefit from periprocedural bridging anticoagulation?
WHY YOU MIGHT THINK PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS HELPFUL
OAC is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for the primary or secondary prevention of thromboembolic events, with more than 35 million prescriptions written annually in the United States alone.1 Many of these patients will require a temporary interruption of their OAC for surgery or an invasive procedure.2 As a result, patients may be treated with short-acting, or “bridging,” anticoagulants, such as low-molecular-weight heparin (LMWH), to minimize the duration of anticoagulation interruption and theoretically reduce their thromboembolic risk. The rationale for bridging stemmed from small observational studies and expert opinion that perceived the estimated thromboembolic risk to be higher than the estimated bleeding risk.3-5 One such example estimated that the VTE risk increased 100-fold postoperatively, whereas heparin administration only doubled the bleeding risk.3 Furthermore, clinical practice guidelines published from the American Heart Association, American College of Cardiology, European Heart Rhythm Society, and American College of Chest Physicians recommend when and how to initiate bridging anticoagulation. Clinicians have widely adopted these recommendations despite an acknowledged paucity of high-quality supporting evidence.6,7
WHY PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS MORE HARMFUL THAN HELPFUL
Periprocedural Anticoagulation Interruption is Often Not Indicated
Patients undergoing a surgical or invasive procedure may require an interruption of OAC to minimize the periprocedural bleeding risk. The decision to interrupt OAC should generally be based on the procedure-specific bleeding risk. Procedures with low bleeding risk such as cataract surgery, dermatologic biopsy (including Mohs), arthrocentesis, diagnostic gastrointestinal endoscopy, and cardiac pacemaker implantation can be performed safely without OAC interruption.5,7 Despite evidence supporting the safety of periprocedural OAC continuation, unnecessary OAC interruptions remain commonplace and are associated with increased adverse outcomes.8 The BRUISE CONTROL trial compared uninterrupted OAC to interrupted OAC with periprocedural bridging for cardiac pacemaker or defibrillator implantation in a moderate to high thromboembolic risk population. The uninterrupted OAC group experienced significantly fewer pocket hematomas, hematoma evacuations, and prolonged hospitalizations (relative risk [RR] 0.19-0.24; P < .05) without significantly increased thromboembolic events, highlighting the potential benefits of this approach.9
Nevertheless, many surgical and invasive procedures do warrant OAC interruption due to the inherent bleeding risk of the procedure or other logistical considerations. Procedures associated with an increased bleeding risk include urologic surgery (except laser lithotripsy), surgery on highly vascular organs (eg, kidney, liver, spleen), bowel resection, cardiac surgery, and intracranial or spinal surgery.7 Alternatively, some procedures with acceptably low bleeding risk (eg, colonoscopy) are routinely performed during an OAC interruption due to the fact that a high bleeding risk intervention may be necessary during the procedure (eg, polypectomy). This approach may be preferable when a significant amount of preparation is required (eg, bowel preparation) and may be a more efficient use of healthcare resources by avoiding repeat procedures.
Bridging Anticoagulation Does Not Significantly Reduce Thromboembolic Events
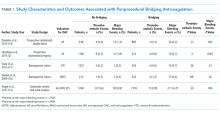
BRIDGE was a randomized, double-blind, placebo-controlled trial among patients with atrial fibrillation (n = 1884) requiring OAC interruption for mostly low-risk, ambulatory surgeries or invasive procedures (eg, gastrointestinal endoscopy, cardiac catheterization). Notably, thromboembolism events were rare, and there was no significant difference in thromboembolism events between patients randomized to placebo or bridging with LMWH (0.4% vs 0.3%, respectively; P = .73).14 However, the proportion of patients enrolled with the highest thromboembolic risk (ie, CHADS2 score 5-6 or prior transient ischemic attack and/or stroke) was low, potentially indicating an underestimated benefit in these patients. Major bleeding was significantly reduced in patients forgoing bridging anticoagulation (1.3% vs 3.2%; RR 0.41; 95% confidence interval, 0.20-0.78; P = .005), although bleeding occurred more frequently than thromboembolism in both groups.
Even though randomized trials assessing the safety and efficacy of bridging for VTE or MHVs have not been completed, evidence is not entirely lacking.16,17 A rigorous observational study limited to a VTE cohort (deep vein thrombosis of upper or lower extremity and/or pulmonary embolism) analyzed the effects of bridging in patients with a surgical or invasive procedure-related OAC interruption. Patients were stratified according to the American College of Chest Physicians perioperative guideline risk-stratification schema, and most VTE events (≥93%) occurred more than 12 months prior to OAC interruption.7 Importantly, the study found a nonsignificant difference in thromboembolism events between patients who were bridged and those who were not (0.0% vs 0.2%, respectively; P = .56), a very low overall thromboembolism event rate (0.2%), and a lack of correlation between events and risk-stratification category.17 In other words, all thromboembolic events occurred in the low- and moderate-risk groups, which include patients who do not warrant bridging under current guidelines. Clinically relevant bleeding occurred in 17 (0.9%) of 1812 patients studied. Notably, 15 (2.7%) of 555 patients receiving bridging suffered clinically relevant bleeding as compared with 2 (0.2%) of 1257 patients forgoing bridging anticoagulation.
The Bleeding Risk of Bridging Anticoagulation Often Outweighs the Potential Benefits
The early observational studies on LMWH bridging demonstrated that thromboembolic events are infrequent (0.4%-0.9%), whereas major bleeding events occur up to 7 times more often (0.7%-6.7%).10-12 The BRIDGE trial demonstrated comparably low thromboembolic events (0.3%). In the patients treated with bridging LMWH, major bleeding (3.2%) occurred 10 times more frequently than thromboembolism.14 Likewise, in a VTE cohort study, Clark et al.17 demonstrated “a 17-fold higher risk of bleeding without a significant difference in the rate of recurrent VTE” in patients bridged with heparin as compared with those who were not. Considering that recurrent VTE and major bleeding events have similar case-fatality rates,18 these increases in major bleeding events without reductions in thromboembolic events unmistakably tip the risk–benefit balance sharply towards an increased risk of harm.
When is bridging anticoagulation potentially helpful?
WHAT SHOULD YOU DO INSTEAD?
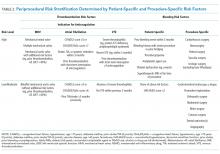
First, determine whether periprocedural OAC interruption is necessary for patients on chronic OAC due to atrial fibrillation, VTE, or MHVs. Avoid unwarranted OAC interruption by discussing the need for OAC interruptions with the surgeon or proceduralist, especially if the surgery is associated with a low bleeding risk and the patient has a high thromboembolic risk. When a periprocedural OAC interruption is justified, bridging should be avoided in the majority of patients, especially those with low to moderate thromboembolic risk or increased bleeding risk according to current risk-stratification schema.7,15,19
Periprocedural management of direct oral anticoagulants (DOACs) is different than that of warfarin. The duration of DOAC interruption is determined by the procedural bleeding risk, drug half-life, and a patient’s creatinine clearance. Although the pharmacokinetics of DOACs generally allow for brief interruptions (eg, 24-48 hours), longer interruptions (eg, 96-120 hours) are warranted prior to high bleeding risk procedures, when drug half-life is prolonged (ie, dabigatran), and in patients with renal impairment. Parenteral bridging anticoagulation is not recommended during brief DOAC interruptions, and substituting a DOAC in place of LMWH for bridging is not advised. The 2017 American College of Cardiology Expert Consensus Decision Pathway provides periprocedural OAC interruption guidance for atrial fibrillation, with many principles applicable to other OAC indications.15We developed an institutional guideline that provides clinicians a structured approach to bridging OAC that steers them away from inappropriate bridging and helps them make decisions when evidence is lacking. Shared decision-making represents another effective method for well-informed patients and clinicians to arrive at a mutually agreed upon bridging decision.
RECOMMENDATIONS
- Avoid unnecessary periprocedural interruptions of OAC, especially for procedures with a low bleeding risk.
- Avoid the administration of bridging anticoagulation in patients with low to moderate thromboembolic risk during periprocedural OAC interruptions.
- In patients with a high thromboembolic risk, an individualized assessment of the patient-specific and procedure-specific bleeding risks versus the thromboembolic risks is necessary when considering bridging anticoagulation administration.
CONCLUSION
Returning to the opening case, the patient requires an anticoagulation interruption and INR correction prior to surgery. Because the CHA2DS2VaSc score of 4 does not categorize him as a high thromboembolic risk, bridging anticoagulation should be avoided. In the majority of patients on OAC, bridging anticoagulation does not reduce thromboembolic events and is associated with increased major bleeding. Unnecessary anticoagulation interruptions should be avoided for procedures associated with low bleeding risk. Bridging should not be administered to the majority of patients requiring a periprocedural anticoagulation interruption.
Do
Disclosure: The authors report no conflicts of interest relevant to this article to disclose.
1. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5(5):615-621. PubMed
2. Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494. PubMed
3. Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336(21):1506-1511. PubMed
4. Eckman MH. “Bridging on the river Kwai”: the perioperative management of anticoagulation therapy. Med Decis Making. 2005;25(4):370-373. PubMed
5. Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med. 2003;163(8):901-908. PubMed
6. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071-2104. PubMed
7. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-e350S. PubMed
8. Gerson LB, Gage BF, Owens DK, Triadafilopoulos G. Effect and outcomes of the ASGE guidelines on the periendoscopic management of patients who take anticoagulants. Am J Gastroenterol. 2000;95(7):1717-1724. PubMed
9. Birnie DH, Healey JS, Wells GA, et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med. 2013;368(22):2084-2093. PubMed
10. Douketis JD, Johnson JA, Turpie AG. Low-molecular-weight heparin as bridging anticoagulation during interruption of warfarin: assessment of a standardized periprocedural anticoagulation regimen. Arch Intern Med. 2004;164(12):1319-1326. PubMed
11. Spyropoulos AC, Turpie AG, Dunn AS, et al. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252. PubMed
12. Kovacs MJ, Kearon C, Rodger M, et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation. 2004;110(12):1658-1663. PubMed
13. Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126(13):1630-1639. PubMed
14. Douketis JD, Spyropoulos AC, Kaatz S, et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015;373(9):823-833. PubMed
15. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: A Report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898. PubMed
16. Daniels PR, McBane RD, Litin SC, et al. Peri-procedural anticoagulation management of mechanical prosthetic heart valve patients. Thromb Res. 2009;124(3):300-305. PubMed
17. Clark NP, Witt DM, Davies LE, et al. Bleeding, Recurrent Venous Thromboembolism, and Mortality Risks During Warfarin Interruption for Invasive Procedures. JAMA Intern Med. 2015;175(7):1163-1168. PubMed
18. Carrier M, Le Gal G, Wells PS, Rodger MA. Systematic review: case-fatality rates of recurrent venous thromboembolism and major bleeding events among patients treated for venous thromboembolism. Ann Intern Med. 2010;152(9):578-589. PubMed
19. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159-e1195. PubMed
The “Things We Do for No Reason” (TWDFNR) series reviews practices that have become common parts of hospital care but that may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Oral anticoagulation (OAC) is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for primary and secondary thromboembolism prevention. When patients require surgery or an invasive procedure, “bridging” anticoagulants (eg, enoxaparin) are commonly administered during the period of OAC interruption to reduce thromboembolic risk. This practice stems from small observational studies and expert opinion, which influenced several clinical guidelines despite the lack of high-quality evidence. Although prospective randomized trials of periprocedural bridging in patients with VTE and MHVs are lacking, available evidence is consistent with findings from the BRIDGE trial, which guides the following general recommendations: (1) avoid unnecessary periprocedural interruptions of OAC, especially for low bleeding risk procedures; (2) avoid the administration of periprocedural bridging anticoagulation in patients with low to moderate thromboembolic risk; (3) in patients with high thromboembolic risk, individually assess the patient-specific and procedure-specific bleeding risks versus thromboembolic risks.
A 75-year-old man with a history of hypertension, diabetes mellitus, and atrial fibrillation is admitted for surgical repair of a comminuted intertrochanteric left hip fracture. He suffered a mechanical ground-level fall without loss of consciousness. At baseline, he denies any chest pain, dyspnea on exertion, or recent change in his exercise tolerance. A physical examination is notable for stable vital signs, irregular cardiac rhythm, and a shortened and externally rotated left lower extremity with exquisite tenderness to palpation and range of motion. The patient is taking warfarin for stroke prophylaxis based on a CHA2DS2VaSc score of 4 points. The international normalized ratio (INR) is 1.9 upon admission, and surgery is planned within 48 hours, once the patient is “medically cleared.” Will this patient benefit from periprocedural bridging anticoagulation?
WHY YOU MIGHT THINK PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS HELPFUL
OAC is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for the primary or secondary prevention of thromboembolic events, with more than 35 million prescriptions written annually in the United States alone.1 Many of these patients will require a temporary interruption of their OAC for surgery or an invasive procedure.2 As a result, patients may be treated with short-acting, or “bridging,” anticoagulants, such as low-molecular-weight heparin (LMWH), to minimize the duration of anticoagulation interruption and theoretically reduce their thromboembolic risk. The rationale for bridging stemmed from small observational studies and expert opinion that perceived the estimated thromboembolic risk to be higher than the estimated bleeding risk.3-5 One such example estimated that the VTE risk increased 100-fold postoperatively, whereas heparin administration only doubled the bleeding risk.3 Furthermore, clinical practice guidelines published from the American Heart Association, American College of Cardiology, European Heart Rhythm Society, and American College of Chest Physicians recommend when and how to initiate bridging anticoagulation. Clinicians have widely adopted these recommendations despite an acknowledged paucity of high-quality supporting evidence.6,7
WHY PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS MORE HARMFUL THAN HELPFUL
Periprocedural Anticoagulation Interruption is Often Not Indicated
Patients undergoing a surgical or invasive procedure may require an interruption of OAC to minimize the periprocedural bleeding risk. The decision to interrupt OAC should generally be based on the procedure-specific bleeding risk. Procedures with low bleeding risk such as cataract surgery, dermatologic biopsy (including Mohs), arthrocentesis, diagnostic gastrointestinal endoscopy, and cardiac pacemaker implantation can be performed safely without OAC interruption.5,7 Despite evidence supporting the safety of periprocedural OAC continuation, unnecessary OAC interruptions remain commonplace and are associated with increased adverse outcomes.8 The BRUISE CONTROL trial compared uninterrupted OAC to interrupted OAC with periprocedural bridging for cardiac pacemaker or defibrillator implantation in a moderate to high thromboembolic risk population. The uninterrupted OAC group experienced significantly fewer pocket hematomas, hematoma evacuations, and prolonged hospitalizations (relative risk [RR] 0.19-0.24; P < .05) without significantly increased thromboembolic events, highlighting the potential benefits of this approach.9
Nevertheless, many surgical and invasive procedures do warrant OAC interruption due to the inherent bleeding risk of the procedure or other logistical considerations. Procedures associated with an increased bleeding risk include urologic surgery (except laser lithotripsy), surgery on highly vascular organs (eg, kidney, liver, spleen), bowel resection, cardiac surgery, and intracranial or spinal surgery.7 Alternatively, some procedures with acceptably low bleeding risk (eg, colonoscopy) are routinely performed during an OAC interruption due to the fact that a high bleeding risk intervention may be necessary during the procedure (eg, polypectomy). This approach may be preferable when a significant amount of preparation is required (eg, bowel preparation) and may be a more efficient use of healthcare resources by avoiding repeat procedures.
Bridging Anticoagulation Does Not Significantly Reduce Thromboembolic Events
BRIDGE was a randomized, double-blind, placebo-controlled trial among patients with atrial fibrillation (n = 1884) requiring OAC interruption for mostly low-risk, ambulatory surgeries or invasive procedures (eg, gastrointestinal endoscopy, cardiac catheterization). Notably, thromboembolism events were rare, and there was no significant difference in thromboembolism events between patients randomized to placebo or bridging with LMWH (0.4% vs 0.3%, respectively; P = .73).14 However, the proportion of patients enrolled with the highest thromboembolic risk (ie, CHADS2 score 5-6 or prior transient ischemic attack and/or stroke) was low, potentially indicating an underestimated benefit in these patients. Major bleeding was significantly reduced in patients forgoing bridging anticoagulation (1.3% vs 3.2%; RR 0.41; 95% confidence interval, 0.20-0.78; P = .005), although bleeding occurred more frequently than thromboembolism in both groups.
Even though randomized trials assessing the safety and efficacy of bridging for VTE or MHVs have not been completed, evidence is not entirely lacking.16,17 A rigorous observational study limited to a VTE cohort (deep vein thrombosis of upper or lower extremity and/or pulmonary embolism) analyzed the effects of bridging in patients with a surgical or invasive procedure-related OAC interruption. Patients were stratified according to the American College of Chest Physicians perioperative guideline risk-stratification schema, and most VTE events (≥93%) occurred more than 12 months prior to OAC interruption.7 Importantly, the study found a nonsignificant difference in thromboembolism events between patients who were bridged and those who were not (0.0% vs 0.2%, respectively; P = .56), a very low overall thromboembolism event rate (0.2%), and a lack of correlation between events and risk-stratification category.17 In other words, all thromboembolic events occurred in the low- and moderate-risk groups, which include patients who do not warrant bridging under current guidelines. Clinically relevant bleeding occurred in 17 (0.9%) of 1812 patients studied. Notably, 15 (2.7%) of 555 patients receiving bridging suffered clinically relevant bleeding as compared with 2 (0.2%) of 1257 patients forgoing bridging anticoagulation.
The Bleeding Risk of Bridging Anticoagulation Often Outweighs the Potential Benefits
The early observational studies on LMWH bridging demonstrated that thromboembolic events are infrequent (0.4%-0.9%), whereas major bleeding events occur up to 7 times more often (0.7%-6.7%).10-12 The BRIDGE trial demonstrated comparably low thromboembolic events (0.3%). In the patients treated with bridging LMWH, major bleeding (3.2%) occurred 10 times more frequently than thromboembolism.14 Likewise, in a VTE cohort study, Clark et al.17 demonstrated “a 17-fold higher risk of bleeding without a significant difference in the rate of recurrent VTE” in patients bridged with heparin as compared with those who were not. Considering that recurrent VTE and major bleeding events have similar case-fatality rates,18 these increases in major bleeding events without reductions in thromboembolic events unmistakably tip the risk–benefit balance sharply towards an increased risk of harm.
When is bridging anticoagulation potentially helpful?
WHAT SHOULD YOU DO INSTEAD?
First, determine whether periprocedural OAC interruption is necessary for patients on chronic OAC due to atrial fibrillation, VTE, or MHVs. Avoid unwarranted OAC interruption by discussing the need for OAC interruptions with the surgeon or proceduralist, especially if the surgery is associated with a low bleeding risk and the patient has a high thromboembolic risk. When a periprocedural OAC interruption is justified, bridging should be avoided in the majority of patients, especially those with low to moderate thromboembolic risk or increased bleeding risk according to current risk-stratification schema.7,15,19
Periprocedural management of direct oral anticoagulants (DOACs) is different than that of warfarin. The duration of DOAC interruption is determined by the procedural bleeding risk, drug half-life, and a patient’s creatinine clearance. Although the pharmacokinetics of DOACs generally allow for brief interruptions (eg, 24-48 hours), longer interruptions (eg, 96-120 hours) are warranted prior to high bleeding risk procedures, when drug half-life is prolonged (ie, dabigatran), and in patients with renal impairment. Parenteral bridging anticoagulation is not recommended during brief DOAC interruptions, and substituting a DOAC in place of LMWH for bridging is not advised. The 2017 American College of Cardiology Expert Consensus Decision Pathway provides periprocedural OAC interruption guidance for atrial fibrillation, with many principles applicable to other OAC indications.15We developed an institutional guideline that provides clinicians a structured approach to bridging OAC that steers them away from inappropriate bridging and helps them make decisions when evidence is lacking. Shared decision-making represents another effective method for well-informed patients and clinicians to arrive at a mutually agreed upon bridging decision.
RECOMMENDATIONS
- Avoid unnecessary periprocedural interruptions of OAC, especially for procedures with a low bleeding risk.
- Avoid the administration of bridging anticoagulation in patients with low to moderate thromboembolic risk during periprocedural OAC interruptions.
- In patients with a high thromboembolic risk, an individualized assessment of the patient-specific and procedure-specific bleeding risks versus the thromboembolic risks is necessary when considering bridging anticoagulation administration.
CONCLUSION
Returning to the opening case, the patient requires an anticoagulation interruption and INR correction prior to surgery. Because the CHA2DS2VaSc score of 4 does not categorize him as a high thromboembolic risk, bridging anticoagulation should be avoided. In the majority of patients on OAC, bridging anticoagulation does not reduce thromboembolic events and is associated with increased major bleeding. Unnecessary anticoagulation interruptions should be avoided for procedures associated with low bleeding risk. Bridging should not be administered to the majority of patients requiring a periprocedural anticoagulation interruption.
Do
Disclosure: The authors report no conflicts of interest relevant to this article to disclose.
The “Things We Do for No Reason” (TWDFNR) series reviews practices that have become common parts of hospital care but that may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Oral anticoagulation (OAC) is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for primary and secondary thromboembolism prevention. When patients require surgery or an invasive procedure, “bridging” anticoagulants (eg, enoxaparin) are commonly administered during the period of OAC interruption to reduce thromboembolic risk. This practice stems from small observational studies and expert opinion, which influenced several clinical guidelines despite the lack of high-quality evidence. Although prospective randomized trials of periprocedural bridging in patients with VTE and MHVs are lacking, available evidence is consistent with findings from the BRIDGE trial, which guides the following general recommendations: (1) avoid unnecessary periprocedural interruptions of OAC, especially for low bleeding risk procedures; (2) avoid the administration of periprocedural bridging anticoagulation in patients with low to moderate thromboembolic risk; (3) in patients with high thromboembolic risk, individually assess the patient-specific and procedure-specific bleeding risks versus thromboembolic risks.
A 75-year-old man with a history of hypertension, diabetes mellitus, and atrial fibrillation is admitted for surgical repair of a comminuted intertrochanteric left hip fracture. He suffered a mechanical ground-level fall without loss of consciousness. At baseline, he denies any chest pain, dyspnea on exertion, or recent change in his exercise tolerance. A physical examination is notable for stable vital signs, irregular cardiac rhythm, and a shortened and externally rotated left lower extremity with exquisite tenderness to palpation and range of motion. The patient is taking warfarin for stroke prophylaxis based on a CHA2DS2VaSc score of 4 points. The international normalized ratio (INR) is 1.9 upon admission, and surgery is planned within 48 hours, once the patient is “medically cleared.” Will this patient benefit from periprocedural bridging anticoagulation?
WHY YOU MIGHT THINK PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS HELPFUL
OAC is commonly prescribed to patients with atrial fibrillation, venous thromboembolism (VTE), and mechanical heart valves (MHVs) for the primary or secondary prevention of thromboembolic events, with more than 35 million prescriptions written annually in the United States alone.1 Many of these patients will require a temporary interruption of their OAC for surgery or an invasive procedure.2 As a result, patients may be treated with short-acting, or “bridging,” anticoagulants, such as low-molecular-weight heparin (LMWH), to minimize the duration of anticoagulation interruption and theoretically reduce their thromboembolic risk. The rationale for bridging stemmed from small observational studies and expert opinion that perceived the estimated thromboembolic risk to be higher than the estimated bleeding risk.3-5 One such example estimated that the VTE risk increased 100-fold postoperatively, whereas heparin administration only doubled the bleeding risk.3 Furthermore, clinical practice guidelines published from the American Heart Association, American College of Cardiology, European Heart Rhythm Society, and American College of Chest Physicians recommend when and how to initiate bridging anticoagulation. Clinicians have widely adopted these recommendations despite an acknowledged paucity of high-quality supporting evidence.6,7
WHY PERIPROCEDURAL “BRIDGING” ANTICOAGULATION IS MORE HARMFUL THAN HELPFUL
Periprocedural Anticoagulation Interruption is Often Not Indicated
Patients undergoing a surgical or invasive procedure may require an interruption of OAC to minimize the periprocedural bleeding risk. The decision to interrupt OAC should generally be based on the procedure-specific bleeding risk. Procedures with low bleeding risk such as cataract surgery, dermatologic biopsy (including Mohs), arthrocentesis, diagnostic gastrointestinal endoscopy, and cardiac pacemaker implantation can be performed safely without OAC interruption.5,7 Despite evidence supporting the safety of periprocedural OAC continuation, unnecessary OAC interruptions remain commonplace and are associated with increased adverse outcomes.8 The BRUISE CONTROL trial compared uninterrupted OAC to interrupted OAC with periprocedural bridging for cardiac pacemaker or defibrillator implantation in a moderate to high thromboembolic risk population. The uninterrupted OAC group experienced significantly fewer pocket hematomas, hematoma evacuations, and prolonged hospitalizations (relative risk [RR] 0.19-0.24; P < .05) without significantly increased thromboembolic events, highlighting the potential benefits of this approach.9
Nevertheless, many surgical and invasive procedures do warrant OAC interruption due to the inherent bleeding risk of the procedure or other logistical considerations. Procedures associated with an increased bleeding risk include urologic surgery (except laser lithotripsy), surgery on highly vascular organs (eg, kidney, liver, spleen), bowel resection, cardiac surgery, and intracranial or spinal surgery.7 Alternatively, some procedures with acceptably low bleeding risk (eg, colonoscopy) are routinely performed during an OAC interruption due to the fact that a high bleeding risk intervention may be necessary during the procedure (eg, polypectomy). This approach may be preferable when a significant amount of preparation is required (eg, bowel preparation) and may be a more efficient use of healthcare resources by avoiding repeat procedures.
Bridging Anticoagulation Does Not Significantly Reduce Thromboembolic Events
BRIDGE was a randomized, double-blind, placebo-controlled trial among patients with atrial fibrillation (n = 1884) requiring OAC interruption for mostly low-risk, ambulatory surgeries or invasive procedures (eg, gastrointestinal endoscopy, cardiac catheterization). Notably, thromboembolism events were rare, and there was no significant difference in thromboembolism events between patients randomized to placebo or bridging with LMWH (0.4% vs 0.3%, respectively; P = .73).14 However, the proportion of patients enrolled with the highest thromboembolic risk (ie, CHADS2 score 5-6 or prior transient ischemic attack and/or stroke) was low, potentially indicating an underestimated benefit in these patients. Major bleeding was significantly reduced in patients forgoing bridging anticoagulation (1.3% vs 3.2%; RR 0.41; 95% confidence interval, 0.20-0.78; P = .005), although bleeding occurred more frequently than thromboembolism in both groups.
Even though randomized trials assessing the safety and efficacy of bridging for VTE or MHVs have not been completed, evidence is not entirely lacking.16,17 A rigorous observational study limited to a VTE cohort (deep vein thrombosis of upper or lower extremity and/or pulmonary embolism) analyzed the effects of bridging in patients with a surgical or invasive procedure-related OAC interruption. Patients were stratified according to the American College of Chest Physicians perioperative guideline risk-stratification schema, and most VTE events (≥93%) occurred more than 12 months prior to OAC interruption.7 Importantly, the study found a nonsignificant difference in thromboembolism events between patients who were bridged and those who were not (0.0% vs 0.2%, respectively; P = .56), a very low overall thromboembolism event rate (0.2%), and a lack of correlation between events and risk-stratification category.17 In other words, all thromboembolic events occurred in the low- and moderate-risk groups, which include patients who do not warrant bridging under current guidelines. Clinically relevant bleeding occurred in 17 (0.9%) of 1812 patients studied. Notably, 15 (2.7%) of 555 patients receiving bridging suffered clinically relevant bleeding as compared with 2 (0.2%) of 1257 patients forgoing bridging anticoagulation.
The Bleeding Risk of Bridging Anticoagulation Often Outweighs the Potential Benefits
The early observational studies on LMWH bridging demonstrated that thromboembolic events are infrequent (0.4%-0.9%), whereas major bleeding events occur up to 7 times more often (0.7%-6.7%).10-12 The BRIDGE trial demonstrated comparably low thromboembolic events (0.3%). In the patients treated with bridging LMWH, major bleeding (3.2%) occurred 10 times more frequently than thromboembolism.14 Likewise, in a VTE cohort study, Clark et al.17 demonstrated “a 17-fold higher risk of bleeding without a significant difference in the rate of recurrent VTE” in patients bridged with heparin as compared with those who were not. Considering that recurrent VTE and major bleeding events have similar case-fatality rates,18 these increases in major bleeding events without reductions in thromboembolic events unmistakably tip the risk–benefit balance sharply towards an increased risk of harm.
When is bridging anticoagulation potentially helpful?
WHAT SHOULD YOU DO INSTEAD?
First, determine whether periprocedural OAC interruption is necessary for patients on chronic OAC due to atrial fibrillation, VTE, or MHVs. Avoid unwarranted OAC interruption by discussing the need for OAC interruptions with the surgeon or proceduralist, especially if the surgery is associated with a low bleeding risk and the patient has a high thromboembolic risk. When a periprocedural OAC interruption is justified, bridging should be avoided in the majority of patients, especially those with low to moderate thromboembolic risk or increased bleeding risk according to current risk-stratification schema.7,15,19
Periprocedural management of direct oral anticoagulants (DOACs) is different than that of warfarin. The duration of DOAC interruption is determined by the procedural bleeding risk, drug half-life, and a patient’s creatinine clearance. Although the pharmacokinetics of DOACs generally allow for brief interruptions (eg, 24-48 hours), longer interruptions (eg, 96-120 hours) are warranted prior to high bleeding risk procedures, when drug half-life is prolonged (ie, dabigatran), and in patients with renal impairment. Parenteral bridging anticoagulation is not recommended during brief DOAC interruptions, and substituting a DOAC in place of LMWH for bridging is not advised. The 2017 American College of Cardiology Expert Consensus Decision Pathway provides periprocedural OAC interruption guidance for atrial fibrillation, with many principles applicable to other OAC indications.15We developed an institutional guideline that provides clinicians a structured approach to bridging OAC that steers them away from inappropriate bridging and helps them make decisions when evidence is lacking. Shared decision-making represents another effective method for well-informed patients and clinicians to arrive at a mutually agreed upon bridging decision.
RECOMMENDATIONS
- Avoid unnecessary periprocedural interruptions of OAC, especially for procedures with a low bleeding risk.
- Avoid the administration of bridging anticoagulation in patients with low to moderate thromboembolic risk during periprocedural OAC interruptions.
- In patients with a high thromboembolic risk, an individualized assessment of the patient-specific and procedure-specific bleeding risks versus the thromboembolic risks is necessary when considering bridging anticoagulation administration.
CONCLUSION
Returning to the opening case, the patient requires an anticoagulation interruption and INR correction prior to surgery. Because the CHA2DS2VaSc score of 4 does not categorize him as a high thromboembolic risk, bridging anticoagulation should be avoided. In the majority of patients on OAC, bridging anticoagulation does not reduce thromboembolic events and is associated with increased major bleeding. Unnecessary anticoagulation interruptions should be avoided for procedures associated with low bleeding risk. Bridging should not be administered to the majority of patients requiring a periprocedural anticoagulation interruption.
Do
Disclosure: The authors report no conflicts of interest relevant to this article to disclose.
1. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5(5):615-621. PubMed
2. Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494. PubMed
3. Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336(21):1506-1511. PubMed
4. Eckman MH. “Bridging on the river Kwai”: the perioperative management of anticoagulation therapy. Med Decis Making. 2005;25(4):370-373. PubMed
5. Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med. 2003;163(8):901-908. PubMed
6. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071-2104. PubMed
7. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-e350S. PubMed
8. Gerson LB, Gage BF, Owens DK, Triadafilopoulos G. Effect and outcomes of the ASGE guidelines on the periendoscopic management of patients who take anticoagulants. Am J Gastroenterol. 2000;95(7):1717-1724. PubMed
9. Birnie DH, Healey JS, Wells GA, et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med. 2013;368(22):2084-2093. PubMed
10. Douketis JD, Johnson JA, Turpie AG. Low-molecular-weight heparin as bridging anticoagulation during interruption of warfarin: assessment of a standardized periprocedural anticoagulation regimen. Arch Intern Med. 2004;164(12):1319-1326. PubMed
11. Spyropoulos AC, Turpie AG, Dunn AS, et al. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252. PubMed
12. Kovacs MJ, Kearon C, Rodger M, et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation. 2004;110(12):1658-1663. PubMed
13. Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126(13):1630-1639. PubMed
14. Douketis JD, Spyropoulos AC, Kaatz S, et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015;373(9):823-833. PubMed
15. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: A Report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898. PubMed
16. Daniels PR, McBane RD, Litin SC, et al. Peri-procedural anticoagulation management of mechanical prosthetic heart valve patients. Thromb Res. 2009;124(3):300-305. PubMed
17. Clark NP, Witt DM, Davies LE, et al. Bleeding, Recurrent Venous Thromboembolism, and Mortality Risks During Warfarin Interruption for Invasive Procedures. JAMA Intern Med. 2015;175(7):1163-1168. PubMed
18. Carrier M, Le Gal G, Wells PS, Rodger MA. Systematic review: case-fatality rates of recurrent venous thromboembolism and major bleeding events among patients treated for venous thromboembolism. Ann Intern Med. 2010;152(9):578-589. PubMed
19. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159-e1195. PubMed
1. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5(5):615-621. PubMed
2. Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488-494. PubMed
3. Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336(21):1506-1511. PubMed
4. Eckman MH. “Bridging on the river Kwai”: the perioperative management of anticoagulation therapy. Med Decis Making. 2005;25(4):370-373. PubMed
5. Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med. 2003;163(8):901-908. PubMed
6. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071-2104. PubMed
7. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-e350S. PubMed
8. Gerson LB, Gage BF, Owens DK, Triadafilopoulos G. Effect and outcomes of the ASGE guidelines on the periendoscopic management of patients who take anticoagulants. Am J Gastroenterol. 2000;95(7):1717-1724. PubMed
9. Birnie DH, Healey JS, Wells GA, et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med. 2013;368(22):2084-2093. PubMed
10. Douketis JD, Johnson JA, Turpie AG. Low-molecular-weight heparin as bridging anticoagulation during interruption of warfarin: assessment of a standardized periprocedural anticoagulation regimen. Arch Intern Med. 2004;164(12):1319-1326. PubMed
11. Spyropoulos AC, Turpie AG, Dunn AS, et al. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246-1252. PubMed
12. Kovacs MJ, Kearon C, Rodger M, et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation. 2004;110(12):1658-1663. PubMed
13. Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126(13):1630-1639. PubMed
14. Douketis JD, Spyropoulos AC, Kaatz S, et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015;373(9):823-833. PubMed
15. Doherty JU, Gluckman TJ, Hucker WJ, et al. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: A Report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol. 2017;69(7):871-898. PubMed
16. Daniels PR, McBane RD, Litin SC, et al. Peri-procedural anticoagulation management of mechanical prosthetic heart valve patients. Thromb Res. 2009;124(3):300-305. PubMed
17. Clark NP, Witt DM, Davies LE, et al. Bleeding, Recurrent Venous Thromboembolism, and Mortality Risks During Warfarin Interruption for Invasive Procedures. JAMA Intern Med. 2015;175(7):1163-1168. PubMed
18. Carrier M, Le Gal G, Wells PS, Rodger MA. Systematic review: case-fatality rates of recurrent venous thromboembolism and major bleeding events among patients treated for venous thromboembolism. Ann Intern Med. 2010;152(9):578-589. PubMed
19. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159-e1195. PubMed
© 2018 Society of Hospital Medicine