User login
ANSWER
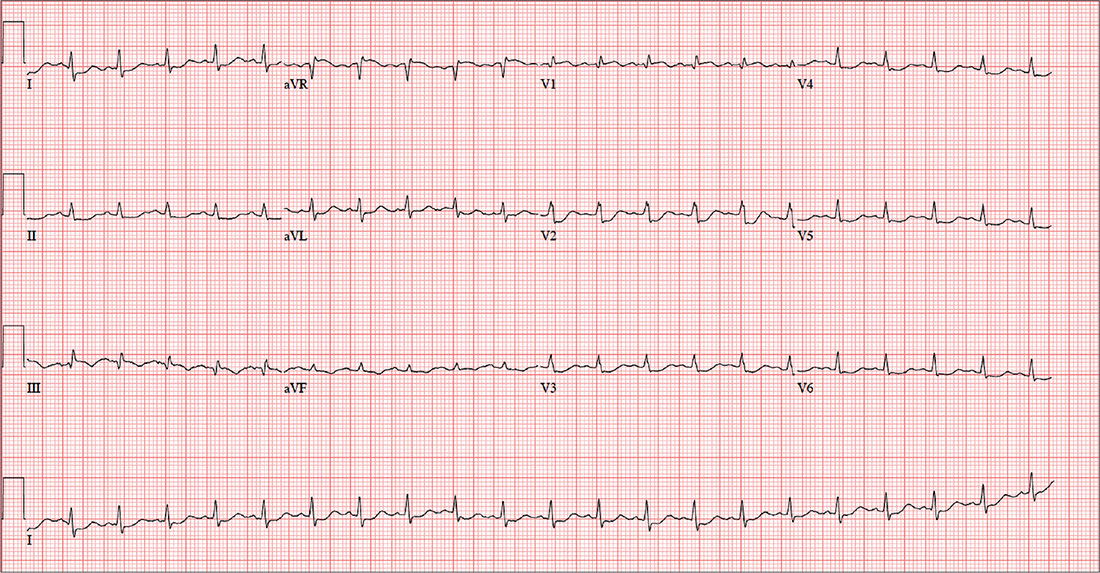
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
ANSWER
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
ANSWER
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
For the past six hours, a 58-year-old man has been experiencing substernal chest discomfort. He is a commercial airline pilot for a regional carrier. Earlier today, he served as co-pilot on a roundtrip flight; about one hour before take-off, he started to feel a dull aching sensation in his chest that he attributed to his recently diagnosed gastroesophageal reflux disease (GERD). After landing, he purchased antacids in the airport terminal and took several, which provided only mild relief for the return trip. The pilot in command suggested he “get checked out” to make certain he didn’t have a bleeding ulcer.
Upon arrival at your facility, the patient appears uncomfortable but denies pain in his chest; there is no radiation to the neck, back, or arm. He denies palpitations, nausea, vomiting, diarrhea, and constipation. He says he feels more short of breath now than he did earlier, adding that “something just doesn’t feel right.”
The patient is a widower; his wife died of breast cancer at age 40. His daughter and son-in-law live in the same neighborhood so he can be close to his grandson. An avid triathlon participant, he has his own gym at home.
His medical history is remarkable for GERD, which was confirmed two months ago by upper endoscopy following several episodes of epigastric pain. He was prescribed a proton pump inhibitor, which he has forgotten to take for the past two days. His last flight physical, performed one year ago, was normal. Surgical history is remarkable for a tonsillectomy and a left inguinal hernia repair, both during childhood.
His current medication list includes lansoprazole and ibuprofen (as needed for musculoskeletal pain). He does not smoke, and he occasionally has a beer on the weekends when he isn’t working. The review of systems is noncontributory apart from his previously detailed symptoms.
Vital signs include a blood pressure of 130/86 mm Hg; pulse, 128 beats/min; respiratory rate, 12 breaths/min-1; and temperature, 97.9°F. His weight is 189 lb and his height, 73 in.
Physical exam reveals an uncomfortable, anxious-appearing male who is otherwise in excellent physical shape. Pertinent findings include a normal thyroid, no evidence of jugular venous distention, and clear lung fields bilaterally. The cardiac exam reveals a regular rate of 130 beats/min with no evidence of murmurs or rubs. The abdomen is flat and nontender, with no organomegaly. Peripheral pulses are equal bilaterally, and there is no peripheral edema. The neurologic exam is grossly intact.
A chest x-ray, ECG, and bloodwork are obtained. The ECG reveals a ventricular rate of 128 beats/min; PR interval, 136 ms; QRS duration, 72 ms; QT/QTc interval, 326/475 ms; P axis, 44°; R axis, 40°; and T axis, –47°. The ECG obtained during his flight physical one year ago showed normal sinus rhythm with nonspecific ST- and T-wave changes but was otherwise normal. With this history in mind, what is your interpretation of today’s ECG?