User login
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
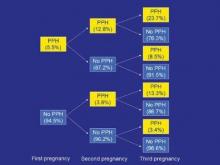
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
FROM THE ANNUAL MEETING OF THE SOCIETY FOR OBSTETRIC ANESTHESIA AND PERINATOLOGY