User login
Chronic obstructive pulmonary disease (COPD) affects between 11 and 24 million people in the U.S. and is the third leading cause of death in this country.1,2 Airflow obstruction on spirometry in addition to respiratory symptoms is required to establish a diagnosis of COPD.3,4 As many as 40% of patients with a clinical diagnosis of COPD have not had spirometry or have spirometry results inconsistent with the diagnosis of COPD.5,6 In addition to recommended spirometry, many patients with COPD do not receive other evidence-based therapies.7,8
About 50% of patients in the Minneapolis VA Health Care System (MVAHCS) receive care in its rural community-based outreach clinics (CBOCs). Data regarding the quality of general medical care between rural and urban populations are sparse; however, studies suggest that the quality of care delivered in rural clinics may be lower than the care provided in an urban setting.9-12 Care for patients with COPD in an urban setting is suboptimal with only 58% of patients receiving guideline-based care, and there are no comparative data for penetrance in the rural setting.8 Most published studies on patients with COPD treated in rural vs urban locations are outcomes studies that queried statewide or national registry data evaluating the frequency of emergency department (ED) visits or hospital admissions for COPD exacerbations, all-cause mortality, or COPD exacerbation-related mortality.13-18 There are no studies examining potential differences in the quality of health care received by patients with COPD in rural vs urban locations or whether these potential differences are associated with changes in health care utilization.
The authors sought to determine whether patients with the diagnosis of COPD treated in the MVAHCS and its 13 CBOCs receive similar quality of disease-related health care in rural vs urban primary care clinic locations. The authors hypothesized that patients who receive their primary care in rural clinics would be less likely to have had spirometry or to receive respiratory immunizations and short- or long-acting inhalers and that discrepancies would be associated with increased health care utilization in rural areas as measured by prescriptions for systemic corticosteroids, antibiotics, ED visits, or hospital admissions for COPD exacerbations.
Methods
The MVAHCS has 14 primary care locations; these locations were designated as rural or urban based on the Rural-Urban Commuting Area codes.19,20 There were 4 urban locations and 10 rural clinics; all rural clinics were farther than 40 miles from the main Minneapolis VAMC.
Patient Selection
The authors performed a retrospective chart review after receiving an institutional review board waiver for this quality assessment study. All patients who had a prior ICD-9 encounter diagnosis of COPD (codes: 491.0, 491.1, 491.2, 491.20, 491.21, 491.22, 491.8, 491.9, 492.0, 492.8, 494, 494.0, 494.1, 496) and who were seen in primary care during March 2015 were identified. Each subject’s first visit during that month was used as the start of the retrospective 1-year look-back period. All eligible subjects were sorted based on their rural or urban location and a randomly assigned number. Patients were then selected according to ascending numbers from each rural and urban clinic in proportion to the clinic’s representation among all eligible patients.
Outcomes
The primary outcomes—possible discrepancies in quality of health care for patients with COPD in rural vs urban primary care clinics—were assessed by (1) prior spirometry; (2) any prior pneumonia vaccination; (3) an influenza vaccination within the past year; (4) prescriptions within the past year for a short-acting beta agonist (SABA) metered-dose inhaler; and (5) prescriptions for a long-acting inhalers, including long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LAMAs), or inhaled corticosteroids (ICSs).
Secondary outcomes included (1) an active prescription for home oxygen within the past calendar year; (2) health care utilization assessed via prescriptions for intermittent courses of oral corticosteroids; (3) prescriptions for respiratory antibiotics (macrolides, tetracyclines, fluoroquinolones) within the past year for COPD exacerbations; (4) ED visits; (5) hospital admissions (and need for mechanical ventilation) for COPD exacerbations within the past year; and (6) whether patients were seen by either VA or Non-VA pulmonology providers.
Data Collection
Patients’ demographic data and comorbidities were collected via chart review. A 1-year prescription medication list was obtained by an electronic database search of the MVAHCS electronic medical record (EMR). Additional antibiotics and corticosteroid prescriptions for COPD exacerbations paid for by the VA but filled at a local pharmacy were manually searched from a separate database to supplement the electronic prescription list. Comparison of the electronic prescription list and pharmacy records in 25% of patients found 100% concordance in the prescription lists. The investigator manually reviewed and extracted the following data from the EMR, scanned-in records, and a Midwest VA COPD registry database: most recent spirometry results; immunization status for influenza in the past year; prior pneumonia vaccination; home oxygen prescription; whether the patient received respiratory antibiotic or intermittent oral corticosteroid treatment for COPD exacerbations; whether the patient had a ED visit or hospital admission for COPD exacerbation with or without need for mechanical ventilation; and whether the patient had been seen by a pulmonology provider. The investigator reviewed all primary care provider notes in the past year for documentation of non-VA ED visits or hospitalizations that were not present in the EMR, Midwest VA COPD registry database, or scanned patient records.
Data Analysis
Results are described as mean ± standard deviation, median (interquartile range) or proportion, expressed as a percentage as appropriate for the level of measurement and distribution. The proportions meeting the COPD quality of health care outcomes in the urban and rural groups were compared using a chi-square test of proportions, and 95% confidence intervals (CI) on the differences were estimated. Samples of 400 patients each from the rural and urban groups were estimated to provide a 95% 2-sided CI on the differences of about ± 0.05 (5%), assuming the proportion meeting the quality of care outcomes in the urban group would be at least 0.8 (80%).
Results
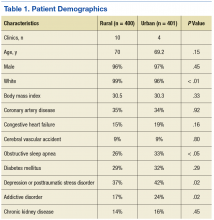
The authors identified 1,538 patients with a previous encounter diagnosis of COPD who were seen in a primary care clinic in the MVAHCS in March of 2015. The authors reviewed the medical records of 801 randomly selected patients: 400 rural clinic patients and 401 urban clinic patients. Demographic characteristics and major comorbidities of rural and urban patients were similar except more rural patients were white, and fewer had a record of obstructive sleep apnea, alcoholism, or addictive disorders (Table 1). Prescriptions for common chronic medical conditions were similar for rural and urban groups, including medications for depression (31% vs 33%) or diabetes mellitus (25% vs 28%). In patients who had spirometry, the severity of COPD, as assessed by mean forced expiratory volume (FEV1), was similar between rural and urban patients (2.06 L vs 2.10 L).
Quality of COPD Care
Spirometry was documented in fewer rural clinic patients than in urban clinic patients (51% vs 82%; difference 31%, 95% CI: 25% to 37%) (Table 2).
COPD Outcomes
Home oxygen prescription rates were similar for rural and urban clinic patients (8% vs 9%; difference 1%, 95% CI: -2% to 5%). Rural patients received fewer prescriptions for intermittent oral corticosteroids (17% vs 31%; difference 14%, 95% CI: 9% to 20%) and antibiotics for COPD exacerbations (18% vs 32%; difference 14%, 95% CI: 8% to 20%). Rural patients had fewer ED visits for COPD exacerbations (7% vs 13%; difference 6%, 95% CI: 2% to 10%), and similar admission rates for COPD exacerbations (5% vs 6%; difference 1%, 95% CI: -2% to 4%). Of the few patients hospitalized for COPD exacerbations, none required mechanical ventilation. There was no significant difference in the number of rural vs urban patients seen by a pulmonologist in the calendar year of the study (6% vs 9%; difference 3%, 95% CI:-1% to 6%), with the majority seen by VA providers: 20/24 rural patients and 35/35 urban patients.
Discussion
Fewer rural patients had prior spirometry; otherwise, the COPD-related quality metrics were similar between rural and urban patient groups in the MVAHCS, including immunizations for pneumonia and influenza, and prescribing rates for short- and long-acting inhaler therapy. Despite the similarity in these COPD quality measures, rural clinic patients seemed to have less health care utilization related to COPD exacerbations.
Spirometry with airflow obstruction in the presence of respiratory symptoms is required for accurate diagnosis of COPD.3,4 Spirometry has been available at the MVAHCS hospital-based clinic for years. Efforts to address this disparity led to implementation of on-site spirometry at all rural and urban clinics about 2 years prior to the patient enrollment visit date for the study. Fewer rural patients had spirometry, which is possibly from prior disparity in resources; yet rates of spirometry in all patients with a clinical diagnosis of COPD in the MVAHCS are higher (rural 51%, urban 82%) than previously reported. A nationwide study of 94,000 veterans with recent clinical diagnosis of COPD found only 37% had spirometry within 2.5 years of diagnosis,21 and another non-VA study (n = 553) showed only 31% of patients discharged from a hospital with a diagnosis of COPD exacerbation had spirometry performed within a 8-year period prior to hospitalization.22
Annual influenza vaccines are recommended for everyone aged > 6 months, and the pneumonia vaccine is recommended for all patients with COPD in order to reduce the risk of COPD exacerbations and pneumonias.23,24 The rates of vaccination at MVAHCS rural and urban clinics for both influenza (79% vs 81%) and pneumococcus (88% vs 91%) are higher than previously published studies of patients with COPD for influenza vaccination (30%-51%) and pneumonia vaccination (21%-51%) and did not differ between rural and urban clinics.7,25-28 The observed high vaccination rates may be due to EMR prompts and requirements to document vaccination status and offer recommended vaccinations.
Long-acting inhalers have been shown to reduce rates of COPD exacerbations and improve patients’ quality of life.29 The authors found no disparity in the prescription rate of short- or long-acting inhalers between rural and urban patients, and no difference in the severity of COPD, as indicated by FEV1, that might influence prescription rates.
The authors attempted to evaluate health care resource utilization as an indicator of health care quality and outcomes. Based on previous reports, the authors expected to find lower quality of care and increased utilization in rural patients. Previous studies have shown rural patients can be more symptomatic with a higher body mass index, airflow obstruction, dyspnea, and exercise capacity index (BODE index) than are patients in urban settings.16,30 Statewide and national registry data have shown rural patients have higher rates of primary care visits, ER visits, and hospitalizations for COPD exacerbations.
Rural patients also have been shown to have higher mortality rates and were more likely to be in a long-term care center and less likely to have home care or palliative care than were their urban counterparts.13-18,31 If the severity of illness is similar in rural and urban areas, higher health care utilization related to COPD would suggest that patients in rural settings may be receiving inferior quality of health care. The authors could not find any previous reports of the quality of COPD care delivered in rural vs urban settings.
In this study the only difference in quality of care was the lower proportion of rural patients with a record of spirometry that is needed to confirm the diagnosis. The observed differences in the quality of care measures wouldn’t be expected to lead to large differences in the outcome measures. Contrary to the literature and the observed similarity in quality of care, rural patients had better COPD outcomes perhaps due to unmeasured differences in risk or failure to capture medical visits outside of the VA system. The severity of COPD based on FEV1 and concurrent diagnoses, such as heart failure, did not suggest that rural patients in this comparison had a higher burden of illness or risk of poor COPD outcomes.
More than 70,000 patients spanning a large geographic region receive primary care at MVAHCS, which provides comparable care to all COPD patients, regardless of location, by using the same EMR system, providing evidence-based order sets for disease management, proactively offering on-site and remote COPD case managers for high-risk patients, and more recently, implementing on-site spirometry testing in all clinics. This approach as opposed to the traditional outreach clinic model may in part explain the similarity in quality of care in urban and rural clinics that was not reported in previous studies.
Limitations
This study was performed retrospectively, increasing the potential of missing data, especially from outside the VA health care system. Patients were not randomly assigned to rural or urban clinics, so differences in patient characteristics could exist. Alcohol and addictive disorders were more common in urban patients, which might affect adherence to prescribed medications. In addition, lower rate of obstructive sleep apnea was found in the rural population, which has been linked to increased airway inflammation and COPD exacerbations resulting in hospitalization.32,33 Mortality was not assessed as all patients were alive and seen in clinic at time of enrollment.
The authors were not able to record a patients’ residence in a long-term care facility or institutionalization, use of home care, or palliative care services due to limitations in the EMR system. Whether patients received comanaged primary care or underwent pulmonary rehabilitation could not be obtained from the EMR. Most patients never had lung volumes or diffusion capacity and thus were not included. The authors could not report whether inhaler therapy was appropriate compared with the Global Initiative for Chronic Obstructive Lund Disease(GOLD)severity score because most of the spirometry was done at a discordant time to when inhaler therapy was assessed, and new GOLD guidelines include patient symptoms that were not reliably recorded in the EMR. Last, the authors had hoped to include smoking status and cessation practices as part of the quality measures, but due to significant variability in patients’ documented smoking status in the same period, the data were deemed unreliable.
Conclusion
No disparities were found between rural and urban clinics in the quality of health care for patients with COPD in the MVAHCS except that fewer rural patients had prior spirometry; a difference that is likely due to the fact that only recently has spirometry been implemented in the MVAHCS rural clinics. Overall the quality of COPD care was high and above the previously reported rates. Further larger studies of rural and urban quality of health care for patients with COPD are needed in other VA and non-VA systems to determine whether disparities exist and whether they are associated with clinical outcomes, including ED visits, hospitalizations, and mortality.
1. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014(260):1-161.
2. Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep. 2016;64(2):1-119.
3. Celli BR, MacNee W, Force AET. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932-946.
4. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS; GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256-1276.
5. Ghattas C, Dai A, Gemmel DJ, Awad MH. Over diagnosis of chronic obstructive pulmonary disease in an underserved patient population. Int J Chron Obstruct Pulmon Dis. 2013;8:545-549.
6. Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195(4):168-171.
7. Lopez-Campos JL, Abad Arranz M, Calero-Acuña C, et al. Guideline adherence in outpatient clinics for chronic obstructive pulmonary disease: results from a clinical audit. PLoS One. 2016;11(3):e0151896.
8. McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645.
9. Spoont M, Greer N, Su J, Fitzgerald P, Rutks I, Wilt TJ. Rural vs. Urban Ambulatory Health Care: A Systematic Review. Washington, DC: U.S. Department of Veteran Affairs; 2011.
10. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of Veterans. J Rural Health. 2006;22(3):204-211.
11. Wallace AE, Weeks WB, Wang S, Lee AF, Kazis LE. Rural and urban disparities in health-related quality of life among veterans with psychiatric disorders. Psychiatr Serv. 2006;57(6):851-856.
12. Meit M, Knudson A, Gilbert T, et al; Rural Health Reform Policy Research Center. The 2014 update of the rural-urban chartbook. https://ruralhealth.und .edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf. Published October 2014. Accessed April 18, 2017.
13. Jackson BE, Suzuki S, Coultas D, et al. Safety-net facilities and hospitalization rates of chronic obstructive pulmonary disease: a cross-sectional analysis of the 2007 Texas Health Care Information Council inpatient data. Int J Chron Obstruct Pulmon Dis. 2011;6:563-571.
14. Jackson BE, Suzuki S, Lo K, et al. Geographic disparity in COPD hospitalization rates among the Texas population. Respir Med. 2011;105(5):734-739.15. Skinner HG, Blanchard J, Elixhauser A. Trends in emergency department visits, 2006-2011: statistical brief #179. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb179-Emergency-Department-Trends.pdf. Published September 2014. Accessed May 9, 2017.
16. Jackson BE, Coultas DB, Suzuki S, Singh KP, Bae S. Rural-urban disparities in quality of life among patients with COPD. J Rural Health. 2013;29(suppl 1):62S-69S.
17. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med. 2014;46(2):e19-e29.
18. Abrams TE, Vaughan-Sarrazin M, Fan VS, Kaboli PJ. Geographic isolation and the risk for chronic obstructive pulmonary disease-related mortality: a cohort study. Ann Intern Med. 2011;155(2):80-86.
19. Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149-1155.
20. U.S. Department of Agriculture, Economic Research Service. Rural-urban commuting area codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx#U20K1F50H0A. Updated October 12, 2016. Accessed May 9, 2017.
21. Joo MJ, Lee TA, Weiss KB. Geographic variation of spirometry use in newly diagnosed COPD. Chest. 2008;134(1):38-45.
22. Damarla M, Celli BR, Mullerova HX, Pinto-Plata VM. Discrepancy in the use of confirmatory tests in patients hospitalized with the diagnosis of chronic obstructive pulmonary disease or congestive heart failure. Respir Care. 2006;51(10):1120-1124.
23. Grohskopf LA, Sokolow LZ, Olsen SJ, Bresee JS, Broder KR, Karron RA. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2015-16 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64(30):818-825.
24. Kim DK, Bridges CB, Harriman KH; Advisory Committee on Immunization Practices. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med. 2016;164(3):184-194.
25. Cimen P, Unlu M, Kirakli C, et al. Should patients with COPD be vaccinated? Respir Care. 2015;60(2):239-243.
26. Mowls DS, Cheruvu VK, Zullo MD. Influenza vaccination in adults with chronic obstructive pulmonary disease: the impact of a diagnostic breathing test on vaccination rates PLoS One. 2013;8(6):e67600.
27. Shoup JA, Madrid C, Koehler C, et al. Effectiveness and cost of influenza vaccine reminders for adults with asthma or chronic obstructive pulmonary disease. Am J Manag Care. 2015;21(7):e405-e413.
28. Arinez-Fernandez MC, Carrasco-Garrido P, Garcia-Carballo M, Hernandez-Barrera V, de Miguel AG, Jimenez-Garcia R. Determinants of pneumococcal vaccination among patients with chronic obstructive pulmonary disease in Spain. Hum Vaccin. 2006;2(3):99-104.29. Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
30. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012.
31. Goodridge D, Lawson J, Rennie D, Marciniuk D. Rural/urban differences in health care utilization and place of death for persons with respiratory illness in the last year of life. Rural Remote Health. 2010;10(2):1349.
32. Wang Y, Hu K, Liu K, et al. Obstructive sleep apnea exacerbates airway inflammation in patients with chronic obstructive pulmonary disease. Sleep Med. 2015;16(9):1123-1130.
33. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325-331
Chronic obstructive pulmonary disease (COPD) affects between 11 and 24 million people in the U.S. and is the third leading cause of death in this country.1,2 Airflow obstruction on spirometry in addition to respiratory symptoms is required to establish a diagnosis of COPD.3,4 As many as 40% of patients with a clinical diagnosis of COPD have not had spirometry or have spirometry results inconsistent with the diagnosis of COPD.5,6 In addition to recommended spirometry, many patients with COPD do not receive other evidence-based therapies.7,8
About 50% of patients in the Minneapolis VA Health Care System (MVAHCS) receive care in its rural community-based outreach clinics (CBOCs). Data regarding the quality of general medical care between rural and urban populations are sparse; however, studies suggest that the quality of care delivered in rural clinics may be lower than the care provided in an urban setting.9-12 Care for patients with COPD in an urban setting is suboptimal with only 58% of patients receiving guideline-based care, and there are no comparative data for penetrance in the rural setting.8 Most published studies on patients with COPD treated in rural vs urban locations are outcomes studies that queried statewide or national registry data evaluating the frequency of emergency department (ED) visits or hospital admissions for COPD exacerbations, all-cause mortality, or COPD exacerbation-related mortality.13-18 There are no studies examining potential differences in the quality of health care received by patients with COPD in rural vs urban locations or whether these potential differences are associated with changes in health care utilization.
The authors sought to determine whether patients with the diagnosis of COPD treated in the MVAHCS and its 13 CBOCs receive similar quality of disease-related health care in rural vs urban primary care clinic locations. The authors hypothesized that patients who receive their primary care in rural clinics would be less likely to have had spirometry or to receive respiratory immunizations and short- or long-acting inhalers and that discrepancies would be associated with increased health care utilization in rural areas as measured by prescriptions for systemic corticosteroids, antibiotics, ED visits, or hospital admissions for COPD exacerbations.
Methods
The MVAHCS has 14 primary care locations; these locations were designated as rural or urban based on the Rural-Urban Commuting Area codes.19,20 There were 4 urban locations and 10 rural clinics; all rural clinics were farther than 40 miles from the main Minneapolis VAMC.
Patient Selection
The authors performed a retrospective chart review after receiving an institutional review board waiver for this quality assessment study. All patients who had a prior ICD-9 encounter diagnosis of COPD (codes: 491.0, 491.1, 491.2, 491.20, 491.21, 491.22, 491.8, 491.9, 492.0, 492.8, 494, 494.0, 494.1, 496) and who were seen in primary care during March 2015 were identified. Each subject’s first visit during that month was used as the start of the retrospective 1-year look-back period. All eligible subjects were sorted based on their rural or urban location and a randomly assigned number. Patients were then selected according to ascending numbers from each rural and urban clinic in proportion to the clinic’s representation among all eligible patients.
Outcomes
The primary outcomes—possible discrepancies in quality of health care for patients with COPD in rural vs urban primary care clinics—were assessed by (1) prior spirometry; (2) any prior pneumonia vaccination; (3) an influenza vaccination within the past year; (4) prescriptions within the past year for a short-acting beta agonist (SABA) metered-dose inhaler; and (5) prescriptions for a long-acting inhalers, including long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LAMAs), or inhaled corticosteroids (ICSs).
Secondary outcomes included (1) an active prescription for home oxygen within the past calendar year; (2) health care utilization assessed via prescriptions for intermittent courses of oral corticosteroids; (3) prescriptions for respiratory antibiotics (macrolides, tetracyclines, fluoroquinolones) within the past year for COPD exacerbations; (4) ED visits; (5) hospital admissions (and need for mechanical ventilation) for COPD exacerbations within the past year; and (6) whether patients were seen by either VA or Non-VA pulmonology providers.
Data Collection
Patients’ demographic data and comorbidities were collected via chart review. A 1-year prescription medication list was obtained by an electronic database search of the MVAHCS electronic medical record (EMR). Additional antibiotics and corticosteroid prescriptions for COPD exacerbations paid for by the VA but filled at a local pharmacy were manually searched from a separate database to supplement the electronic prescription list. Comparison of the electronic prescription list and pharmacy records in 25% of patients found 100% concordance in the prescription lists. The investigator manually reviewed and extracted the following data from the EMR, scanned-in records, and a Midwest VA COPD registry database: most recent spirometry results; immunization status for influenza in the past year; prior pneumonia vaccination; home oxygen prescription; whether the patient received respiratory antibiotic or intermittent oral corticosteroid treatment for COPD exacerbations; whether the patient had a ED visit or hospital admission for COPD exacerbation with or without need for mechanical ventilation; and whether the patient had been seen by a pulmonology provider. The investigator reviewed all primary care provider notes in the past year for documentation of non-VA ED visits or hospitalizations that were not present in the EMR, Midwest VA COPD registry database, or scanned patient records.
Data Analysis
Results are described as mean ± standard deviation, median (interquartile range) or proportion, expressed as a percentage as appropriate for the level of measurement and distribution. The proportions meeting the COPD quality of health care outcomes in the urban and rural groups were compared using a chi-square test of proportions, and 95% confidence intervals (CI) on the differences were estimated. Samples of 400 patients each from the rural and urban groups were estimated to provide a 95% 2-sided CI on the differences of about ± 0.05 (5%), assuming the proportion meeting the quality of care outcomes in the urban group would be at least 0.8 (80%).
Results
The authors identified 1,538 patients with a previous encounter diagnosis of COPD who were seen in a primary care clinic in the MVAHCS in March of 2015. The authors reviewed the medical records of 801 randomly selected patients: 400 rural clinic patients and 401 urban clinic patients. Demographic characteristics and major comorbidities of rural and urban patients were similar except more rural patients were white, and fewer had a record of obstructive sleep apnea, alcoholism, or addictive disorders (Table 1). Prescriptions for common chronic medical conditions were similar for rural and urban groups, including medications for depression (31% vs 33%) or diabetes mellitus (25% vs 28%). In patients who had spirometry, the severity of COPD, as assessed by mean forced expiratory volume (FEV1), was similar between rural and urban patients (2.06 L vs 2.10 L).
Quality of COPD Care
Spirometry was documented in fewer rural clinic patients than in urban clinic patients (51% vs 82%; difference 31%, 95% CI: 25% to 37%) (Table 2).
COPD Outcomes
Home oxygen prescription rates were similar for rural and urban clinic patients (8% vs 9%; difference 1%, 95% CI: -2% to 5%). Rural patients received fewer prescriptions for intermittent oral corticosteroids (17% vs 31%; difference 14%, 95% CI: 9% to 20%) and antibiotics for COPD exacerbations (18% vs 32%; difference 14%, 95% CI: 8% to 20%). Rural patients had fewer ED visits for COPD exacerbations (7% vs 13%; difference 6%, 95% CI: 2% to 10%), and similar admission rates for COPD exacerbations (5% vs 6%; difference 1%, 95% CI: -2% to 4%). Of the few patients hospitalized for COPD exacerbations, none required mechanical ventilation. There was no significant difference in the number of rural vs urban patients seen by a pulmonologist in the calendar year of the study (6% vs 9%; difference 3%, 95% CI:-1% to 6%), with the majority seen by VA providers: 20/24 rural patients and 35/35 urban patients.
Discussion
Fewer rural patients had prior spirometry; otherwise, the COPD-related quality metrics were similar between rural and urban patient groups in the MVAHCS, including immunizations for pneumonia and influenza, and prescribing rates for short- and long-acting inhaler therapy. Despite the similarity in these COPD quality measures, rural clinic patients seemed to have less health care utilization related to COPD exacerbations.
Spirometry with airflow obstruction in the presence of respiratory symptoms is required for accurate diagnosis of COPD.3,4 Spirometry has been available at the MVAHCS hospital-based clinic for years. Efforts to address this disparity led to implementation of on-site spirometry at all rural and urban clinics about 2 years prior to the patient enrollment visit date for the study. Fewer rural patients had spirometry, which is possibly from prior disparity in resources; yet rates of spirometry in all patients with a clinical diagnosis of COPD in the MVAHCS are higher (rural 51%, urban 82%) than previously reported. A nationwide study of 94,000 veterans with recent clinical diagnosis of COPD found only 37% had spirometry within 2.5 years of diagnosis,21 and another non-VA study (n = 553) showed only 31% of patients discharged from a hospital with a diagnosis of COPD exacerbation had spirometry performed within a 8-year period prior to hospitalization.22
Annual influenza vaccines are recommended for everyone aged > 6 months, and the pneumonia vaccine is recommended for all patients with COPD in order to reduce the risk of COPD exacerbations and pneumonias.23,24 The rates of vaccination at MVAHCS rural and urban clinics for both influenza (79% vs 81%) and pneumococcus (88% vs 91%) are higher than previously published studies of patients with COPD for influenza vaccination (30%-51%) and pneumonia vaccination (21%-51%) and did not differ between rural and urban clinics.7,25-28 The observed high vaccination rates may be due to EMR prompts and requirements to document vaccination status and offer recommended vaccinations.
Long-acting inhalers have been shown to reduce rates of COPD exacerbations and improve patients’ quality of life.29 The authors found no disparity in the prescription rate of short- or long-acting inhalers between rural and urban patients, and no difference in the severity of COPD, as indicated by FEV1, that might influence prescription rates.
The authors attempted to evaluate health care resource utilization as an indicator of health care quality and outcomes. Based on previous reports, the authors expected to find lower quality of care and increased utilization in rural patients. Previous studies have shown rural patients can be more symptomatic with a higher body mass index, airflow obstruction, dyspnea, and exercise capacity index (BODE index) than are patients in urban settings.16,30 Statewide and national registry data have shown rural patients have higher rates of primary care visits, ER visits, and hospitalizations for COPD exacerbations.
Rural patients also have been shown to have higher mortality rates and were more likely to be in a long-term care center and less likely to have home care or palliative care than were their urban counterparts.13-18,31 If the severity of illness is similar in rural and urban areas, higher health care utilization related to COPD would suggest that patients in rural settings may be receiving inferior quality of health care. The authors could not find any previous reports of the quality of COPD care delivered in rural vs urban settings.
In this study the only difference in quality of care was the lower proportion of rural patients with a record of spirometry that is needed to confirm the diagnosis. The observed differences in the quality of care measures wouldn’t be expected to lead to large differences in the outcome measures. Contrary to the literature and the observed similarity in quality of care, rural patients had better COPD outcomes perhaps due to unmeasured differences in risk or failure to capture medical visits outside of the VA system. The severity of COPD based on FEV1 and concurrent diagnoses, such as heart failure, did not suggest that rural patients in this comparison had a higher burden of illness or risk of poor COPD outcomes.
More than 70,000 patients spanning a large geographic region receive primary care at MVAHCS, which provides comparable care to all COPD patients, regardless of location, by using the same EMR system, providing evidence-based order sets for disease management, proactively offering on-site and remote COPD case managers for high-risk patients, and more recently, implementing on-site spirometry testing in all clinics. This approach as opposed to the traditional outreach clinic model may in part explain the similarity in quality of care in urban and rural clinics that was not reported in previous studies.
Limitations
This study was performed retrospectively, increasing the potential of missing data, especially from outside the VA health care system. Patients were not randomly assigned to rural or urban clinics, so differences in patient characteristics could exist. Alcohol and addictive disorders were more common in urban patients, which might affect adherence to prescribed medications. In addition, lower rate of obstructive sleep apnea was found in the rural population, which has been linked to increased airway inflammation and COPD exacerbations resulting in hospitalization.32,33 Mortality was not assessed as all patients were alive and seen in clinic at time of enrollment.
The authors were not able to record a patients’ residence in a long-term care facility or institutionalization, use of home care, or palliative care services due to limitations in the EMR system. Whether patients received comanaged primary care or underwent pulmonary rehabilitation could not be obtained from the EMR. Most patients never had lung volumes or diffusion capacity and thus were not included. The authors could not report whether inhaler therapy was appropriate compared with the Global Initiative for Chronic Obstructive Lund Disease(GOLD)severity score because most of the spirometry was done at a discordant time to when inhaler therapy was assessed, and new GOLD guidelines include patient symptoms that were not reliably recorded in the EMR. Last, the authors had hoped to include smoking status and cessation practices as part of the quality measures, but due to significant variability in patients’ documented smoking status in the same period, the data were deemed unreliable.
Conclusion
No disparities were found between rural and urban clinics in the quality of health care for patients with COPD in the MVAHCS except that fewer rural patients had prior spirometry; a difference that is likely due to the fact that only recently has spirometry been implemented in the MVAHCS rural clinics. Overall the quality of COPD care was high and above the previously reported rates. Further larger studies of rural and urban quality of health care for patients with COPD are needed in other VA and non-VA systems to determine whether disparities exist and whether they are associated with clinical outcomes, including ED visits, hospitalizations, and mortality.
Chronic obstructive pulmonary disease (COPD) affects between 11 and 24 million people in the U.S. and is the third leading cause of death in this country.1,2 Airflow obstruction on spirometry in addition to respiratory symptoms is required to establish a diagnosis of COPD.3,4 As many as 40% of patients with a clinical diagnosis of COPD have not had spirometry or have spirometry results inconsistent with the diagnosis of COPD.5,6 In addition to recommended spirometry, many patients with COPD do not receive other evidence-based therapies.7,8
About 50% of patients in the Minneapolis VA Health Care System (MVAHCS) receive care in its rural community-based outreach clinics (CBOCs). Data regarding the quality of general medical care between rural and urban populations are sparse; however, studies suggest that the quality of care delivered in rural clinics may be lower than the care provided in an urban setting.9-12 Care for patients with COPD in an urban setting is suboptimal with only 58% of patients receiving guideline-based care, and there are no comparative data for penetrance in the rural setting.8 Most published studies on patients with COPD treated in rural vs urban locations are outcomes studies that queried statewide or national registry data evaluating the frequency of emergency department (ED) visits or hospital admissions for COPD exacerbations, all-cause mortality, or COPD exacerbation-related mortality.13-18 There are no studies examining potential differences in the quality of health care received by patients with COPD in rural vs urban locations or whether these potential differences are associated with changes in health care utilization.
The authors sought to determine whether patients with the diagnosis of COPD treated in the MVAHCS and its 13 CBOCs receive similar quality of disease-related health care in rural vs urban primary care clinic locations. The authors hypothesized that patients who receive their primary care in rural clinics would be less likely to have had spirometry or to receive respiratory immunizations and short- or long-acting inhalers and that discrepancies would be associated with increased health care utilization in rural areas as measured by prescriptions for systemic corticosteroids, antibiotics, ED visits, or hospital admissions for COPD exacerbations.
Methods
The MVAHCS has 14 primary care locations; these locations were designated as rural or urban based on the Rural-Urban Commuting Area codes.19,20 There were 4 urban locations and 10 rural clinics; all rural clinics were farther than 40 miles from the main Minneapolis VAMC.
Patient Selection
The authors performed a retrospective chart review after receiving an institutional review board waiver for this quality assessment study. All patients who had a prior ICD-9 encounter diagnosis of COPD (codes: 491.0, 491.1, 491.2, 491.20, 491.21, 491.22, 491.8, 491.9, 492.0, 492.8, 494, 494.0, 494.1, 496) and who were seen in primary care during March 2015 were identified. Each subject’s first visit during that month was used as the start of the retrospective 1-year look-back period. All eligible subjects were sorted based on their rural or urban location and a randomly assigned number. Patients were then selected according to ascending numbers from each rural and urban clinic in proportion to the clinic’s representation among all eligible patients.
Outcomes
The primary outcomes—possible discrepancies in quality of health care for patients with COPD in rural vs urban primary care clinics—were assessed by (1) prior spirometry; (2) any prior pneumonia vaccination; (3) an influenza vaccination within the past year; (4) prescriptions within the past year for a short-acting beta agonist (SABA) metered-dose inhaler; and (5) prescriptions for a long-acting inhalers, including long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LAMAs), or inhaled corticosteroids (ICSs).
Secondary outcomes included (1) an active prescription for home oxygen within the past calendar year; (2) health care utilization assessed via prescriptions for intermittent courses of oral corticosteroids; (3) prescriptions for respiratory antibiotics (macrolides, tetracyclines, fluoroquinolones) within the past year for COPD exacerbations; (4) ED visits; (5) hospital admissions (and need for mechanical ventilation) for COPD exacerbations within the past year; and (6) whether patients were seen by either VA or Non-VA pulmonology providers.
Data Collection
Patients’ demographic data and comorbidities were collected via chart review. A 1-year prescription medication list was obtained by an electronic database search of the MVAHCS electronic medical record (EMR). Additional antibiotics and corticosteroid prescriptions for COPD exacerbations paid for by the VA but filled at a local pharmacy were manually searched from a separate database to supplement the electronic prescription list. Comparison of the electronic prescription list and pharmacy records in 25% of patients found 100% concordance in the prescription lists. The investigator manually reviewed and extracted the following data from the EMR, scanned-in records, and a Midwest VA COPD registry database: most recent spirometry results; immunization status for influenza in the past year; prior pneumonia vaccination; home oxygen prescription; whether the patient received respiratory antibiotic or intermittent oral corticosteroid treatment for COPD exacerbations; whether the patient had a ED visit or hospital admission for COPD exacerbation with or without need for mechanical ventilation; and whether the patient had been seen by a pulmonology provider. The investigator reviewed all primary care provider notes in the past year for documentation of non-VA ED visits or hospitalizations that were not present in the EMR, Midwest VA COPD registry database, or scanned patient records.
Data Analysis
Results are described as mean ± standard deviation, median (interquartile range) or proportion, expressed as a percentage as appropriate for the level of measurement and distribution. The proportions meeting the COPD quality of health care outcomes in the urban and rural groups were compared using a chi-square test of proportions, and 95% confidence intervals (CI) on the differences were estimated. Samples of 400 patients each from the rural and urban groups were estimated to provide a 95% 2-sided CI on the differences of about ± 0.05 (5%), assuming the proportion meeting the quality of care outcomes in the urban group would be at least 0.8 (80%).
Results
The authors identified 1,538 patients with a previous encounter diagnosis of COPD who were seen in a primary care clinic in the MVAHCS in March of 2015. The authors reviewed the medical records of 801 randomly selected patients: 400 rural clinic patients and 401 urban clinic patients. Demographic characteristics and major comorbidities of rural and urban patients were similar except more rural patients were white, and fewer had a record of obstructive sleep apnea, alcoholism, or addictive disorders (Table 1). Prescriptions for common chronic medical conditions were similar for rural and urban groups, including medications for depression (31% vs 33%) or diabetes mellitus (25% vs 28%). In patients who had spirometry, the severity of COPD, as assessed by mean forced expiratory volume (FEV1), was similar between rural and urban patients (2.06 L vs 2.10 L).
Quality of COPD Care
Spirometry was documented in fewer rural clinic patients than in urban clinic patients (51% vs 82%; difference 31%, 95% CI: 25% to 37%) (Table 2).
COPD Outcomes
Home oxygen prescription rates were similar for rural and urban clinic patients (8% vs 9%; difference 1%, 95% CI: -2% to 5%). Rural patients received fewer prescriptions for intermittent oral corticosteroids (17% vs 31%; difference 14%, 95% CI: 9% to 20%) and antibiotics for COPD exacerbations (18% vs 32%; difference 14%, 95% CI: 8% to 20%). Rural patients had fewer ED visits for COPD exacerbations (7% vs 13%; difference 6%, 95% CI: 2% to 10%), and similar admission rates for COPD exacerbations (5% vs 6%; difference 1%, 95% CI: -2% to 4%). Of the few patients hospitalized for COPD exacerbations, none required mechanical ventilation. There was no significant difference in the number of rural vs urban patients seen by a pulmonologist in the calendar year of the study (6% vs 9%; difference 3%, 95% CI:-1% to 6%), with the majority seen by VA providers: 20/24 rural patients and 35/35 urban patients.
Discussion
Fewer rural patients had prior spirometry; otherwise, the COPD-related quality metrics were similar between rural and urban patient groups in the MVAHCS, including immunizations for pneumonia and influenza, and prescribing rates for short- and long-acting inhaler therapy. Despite the similarity in these COPD quality measures, rural clinic patients seemed to have less health care utilization related to COPD exacerbations.
Spirometry with airflow obstruction in the presence of respiratory symptoms is required for accurate diagnosis of COPD.3,4 Spirometry has been available at the MVAHCS hospital-based clinic for years. Efforts to address this disparity led to implementation of on-site spirometry at all rural and urban clinics about 2 years prior to the patient enrollment visit date for the study. Fewer rural patients had spirometry, which is possibly from prior disparity in resources; yet rates of spirometry in all patients with a clinical diagnosis of COPD in the MVAHCS are higher (rural 51%, urban 82%) than previously reported. A nationwide study of 94,000 veterans with recent clinical diagnosis of COPD found only 37% had spirometry within 2.5 years of diagnosis,21 and another non-VA study (n = 553) showed only 31% of patients discharged from a hospital with a diagnosis of COPD exacerbation had spirometry performed within a 8-year period prior to hospitalization.22
Annual influenza vaccines are recommended for everyone aged > 6 months, and the pneumonia vaccine is recommended for all patients with COPD in order to reduce the risk of COPD exacerbations and pneumonias.23,24 The rates of vaccination at MVAHCS rural and urban clinics for both influenza (79% vs 81%) and pneumococcus (88% vs 91%) are higher than previously published studies of patients with COPD for influenza vaccination (30%-51%) and pneumonia vaccination (21%-51%) and did not differ between rural and urban clinics.7,25-28 The observed high vaccination rates may be due to EMR prompts and requirements to document vaccination status and offer recommended vaccinations.
Long-acting inhalers have been shown to reduce rates of COPD exacerbations and improve patients’ quality of life.29 The authors found no disparity in the prescription rate of short- or long-acting inhalers between rural and urban patients, and no difference in the severity of COPD, as indicated by FEV1, that might influence prescription rates.
The authors attempted to evaluate health care resource utilization as an indicator of health care quality and outcomes. Based on previous reports, the authors expected to find lower quality of care and increased utilization in rural patients. Previous studies have shown rural patients can be more symptomatic with a higher body mass index, airflow obstruction, dyspnea, and exercise capacity index (BODE index) than are patients in urban settings.16,30 Statewide and national registry data have shown rural patients have higher rates of primary care visits, ER visits, and hospitalizations for COPD exacerbations.
Rural patients also have been shown to have higher mortality rates and were more likely to be in a long-term care center and less likely to have home care or palliative care than were their urban counterparts.13-18,31 If the severity of illness is similar in rural and urban areas, higher health care utilization related to COPD would suggest that patients in rural settings may be receiving inferior quality of health care. The authors could not find any previous reports of the quality of COPD care delivered in rural vs urban settings.
In this study the only difference in quality of care was the lower proportion of rural patients with a record of spirometry that is needed to confirm the diagnosis. The observed differences in the quality of care measures wouldn’t be expected to lead to large differences in the outcome measures. Contrary to the literature and the observed similarity in quality of care, rural patients had better COPD outcomes perhaps due to unmeasured differences in risk or failure to capture medical visits outside of the VA system. The severity of COPD based on FEV1 and concurrent diagnoses, such as heart failure, did not suggest that rural patients in this comparison had a higher burden of illness or risk of poor COPD outcomes.
More than 70,000 patients spanning a large geographic region receive primary care at MVAHCS, which provides comparable care to all COPD patients, regardless of location, by using the same EMR system, providing evidence-based order sets for disease management, proactively offering on-site and remote COPD case managers for high-risk patients, and more recently, implementing on-site spirometry testing in all clinics. This approach as opposed to the traditional outreach clinic model may in part explain the similarity in quality of care in urban and rural clinics that was not reported in previous studies.
Limitations
This study was performed retrospectively, increasing the potential of missing data, especially from outside the VA health care system. Patients were not randomly assigned to rural or urban clinics, so differences in patient characteristics could exist. Alcohol and addictive disorders were more common in urban patients, which might affect adherence to prescribed medications. In addition, lower rate of obstructive sleep apnea was found in the rural population, which has been linked to increased airway inflammation and COPD exacerbations resulting in hospitalization.32,33 Mortality was not assessed as all patients were alive and seen in clinic at time of enrollment.
The authors were not able to record a patients’ residence in a long-term care facility or institutionalization, use of home care, or palliative care services due to limitations in the EMR system. Whether patients received comanaged primary care or underwent pulmonary rehabilitation could not be obtained from the EMR. Most patients never had lung volumes or diffusion capacity and thus were not included. The authors could not report whether inhaler therapy was appropriate compared with the Global Initiative for Chronic Obstructive Lund Disease(GOLD)severity score because most of the spirometry was done at a discordant time to when inhaler therapy was assessed, and new GOLD guidelines include patient symptoms that were not reliably recorded in the EMR. Last, the authors had hoped to include smoking status and cessation practices as part of the quality measures, but due to significant variability in patients’ documented smoking status in the same period, the data were deemed unreliable.
Conclusion
No disparities were found between rural and urban clinics in the quality of health care for patients with COPD in the MVAHCS except that fewer rural patients had prior spirometry; a difference that is likely due to the fact that only recently has spirometry been implemented in the MVAHCS rural clinics. Overall the quality of COPD care was high and above the previously reported rates. Further larger studies of rural and urban quality of health care for patients with COPD are needed in other VA and non-VA systems to determine whether disparities exist and whether they are associated with clinical outcomes, including ED visits, hospitalizations, and mortality.
1. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014(260):1-161.
2. Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep. 2016;64(2):1-119.
3. Celli BR, MacNee W, Force AET. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932-946.
4. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS; GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256-1276.
5. Ghattas C, Dai A, Gemmel DJ, Awad MH. Over diagnosis of chronic obstructive pulmonary disease in an underserved patient population. Int J Chron Obstruct Pulmon Dis. 2013;8:545-549.
6. Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195(4):168-171.
7. Lopez-Campos JL, Abad Arranz M, Calero-Acuña C, et al. Guideline adherence in outpatient clinics for chronic obstructive pulmonary disease: results from a clinical audit. PLoS One. 2016;11(3):e0151896.
8. McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645.
9. Spoont M, Greer N, Su J, Fitzgerald P, Rutks I, Wilt TJ. Rural vs. Urban Ambulatory Health Care: A Systematic Review. Washington, DC: U.S. Department of Veteran Affairs; 2011.
10. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of Veterans. J Rural Health. 2006;22(3):204-211.
11. Wallace AE, Weeks WB, Wang S, Lee AF, Kazis LE. Rural and urban disparities in health-related quality of life among veterans with psychiatric disorders. Psychiatr Serv. 2006;57(6):851-856.
12. Meit M, Knudson A, Gilbert T, et al; Rural Health Reform Policy Research Center. The 2014 update of the rural-urban chartbook. https://ruralhealth.und .edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf. Published October 2014. Accessed April 18, 2017.
13. Jackson BE, Suzuki S, Coultas D, et al. Safety-net facilities and hospitalization rates of chronic obstructive pulmonary disease: a cross-sectional analysis of the 2007 Texas Health Care Information Council inpatient data. Int J Chron Obstruct Pulmon Dis. 2011;6:563-571.
14. Jackson BE, Suzuki S, Lo K, et al. Geographic disparity in COPD hospitalization rates among the Texas population. Respir Med. 2011;105(5):734-739.15. Skinner HG, Blanchard J, Elixhauser A. Trends in emergency department visits, 2006-2011: statistical brief #179. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb179-Emergency-Department-Trends.pdf. Published September 2014. Accessed May 9, 2017.
16. Jackson BE, Coultas DB, Suzuki S, Singh KP, Bae S. Rural-urban disparities in quality of life among patients with COPD. J Rural Health. 2013;29(suppl 1):62S-69S.
17. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med. 2014;46(2):e19-e29.
18. Abrams TE, Vaughan-Sarrazin M, Fan VS, Kaboli PJ. Geographic isolation and the risk for chronic obstructive pulmonary disease-related mortality: a cohort study. Ann Intern Med. 2011;155(2):80-86.
19. Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149-1155.
20. U.S. Department of Agriculture, Economic Research Service. Rural-urban commuting area codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx#U20K1F50H0A. Updated October 12, 2016. Accessed May 9, 2017.
21. Joo MJ, Lee TA, Weiss KB. Geographic variation of spirometry use in newly diagnosed COPD. Chest. 2008;134(1):38-45.
22. Damarla M, Celli BR, Mullerova HX, Pinto-Plata VM. Discrepancy in the use of confirmatory tests in patients hospitalized with the diagnosis of chronic obstructive pulmonary disease or congestive heart failure. Respir Care. 2006;51(10):1120-1124.
23. Grohskopf LA, Sokolow LZ, Olsen SJ, Bresee JS, Broder KR, Karron RA. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2015-16 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64(30):818-825.
24. Kim DK, Bridges CB, Harriman KH; Advisory Committee on Immunization Practices. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med. 2016;164(3):184-194.
25. Cimen P, Unlu M, Kirakli C, et al. Should patients with COPD be vaccinated? Respir Care. 2015;60(2):239-243.
26. Mowls DS, Cheruvu VK, Zullo MD. Influenza vaccination in adults with chronic obstructive pulmonary disease: the impact of a diagnostic breathing test on vaccination rates PLoS One. 2013;8(6):e67600.
27. Shoup JA, Madrid C, Koehler C, et al. Effectiveness and cost of influenza vaccine reminders for adults with asthma or chronic obstructive pulmonary disease. Am J Manag Care. 2015;21(7):e405-e413.
28. Arinez-Fernandez MC, Carrasco-Garrido P, Garcia-Carballo M, Hernandez-Barrera V, de Miguel AG, Jimenez-Garcia R. Determinants of pneumococcal vaccination among patients with chronic obstructive pulmonary disease in Spain. Hum Vaccin. 2006;2(3):99-104.29. Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
30. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012.
31. Goodridge D, Lawson J, Rennie D, Marciniuk D. Rural/urban differences in health care utilization and place of death for persons with respiratory illness in the last year of life. Rural Remote Health. 2010;10(2):1349.
32. Wang Y, Hu K, Liu K, et al. Obstructive sleep apnea exacerbates airway inflammation in patients with chronic obstructive pulmonary disease. Sleep Med. 2015;16(9):1123-1130.
33. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325-331
1. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014(260):1-161.
2. Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep. 2016;64(2):1-119.
3. Celli BR, MacNee W, Force AET. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932-946.
4. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS; GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256-1276.
5. Ghattas C, Dai A, Gemmel DJ, Awad MH. Over diagnosis of chronic obstructive pulmonary disease in an underserved patient population. Int J Chron Obstruct Pulmon Dis. 2013;8:545-549.
6. Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195(4):168-171.
7. Lopez-Campos JL, Abad Arranz M, Calero-Acuña C, et al. Guideline adherence in outpatient clinics for chronic obstructive pulmonary disease: results from a clinical audit. PLoS One. 2016;11(3):e0151896.
8. McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645.
9. Spoont M, Greer N, Su J, Fitzgerald P, Rutks I, Wilt TJ. Rural vs. Urban Ambulatory Health Care: A Systematic Review. Washington, DC: U.S. Department of Veteran Affairs; 2011.
10. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of Veterans. J Rural Health. 2006;22(3):204-211.
11. Wallace AE, Weeks WB, Wang S, Lee AF, Kazis LE. Rural and urban disparities in health-related quality of life among veterans with psychiatric disorders. Psychiatr Serv. 2006;57(6):851-856.
12. Meit M, Knudson A, Gilbert T, et al; Rural Health Reform Policy Research Center. The 2014 update of the rural-urban chartbook. https://ruralhealth.und .edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf. Published October 2014. Accessed April 18, 2017.
13. Jackson BE, Suzuki S, Coultas D, et al. Safety-net facilities and hospitalization rates of chronic obstructive pulmonary disease: a cross-sectional analysis of the 2007 Texas Health Care Information Council inpatient data. Int J Chron Obstruct Pulmon Dis. 2011;6:563-571.
14. Jackson BE, Suzuki S, Lo K, et al. Geographic disparity in COPD hospitalization rates among the Texas population. Respir Med. 2011;105(5):734-739.15. Skinner HG, Blanchard J, Elixhauser A. Trends in emergency department visits, 2006-2011: statistical brief #179. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb179-Emergency-Department-Trends.pdf. Published September 2014. Accessed May 9, 2017.
16. Jackson BE, Coultas DB, Suzuki S, Singh KP, Bae S. Rural-urban disparities in quality of life among patients with COPD. J Rural Health. 2013;29(suppl 1):62S-69S.
17. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med. 2014;46(2):e19-e29.
18. Abrams TE, Vaughan-Sarrazin M, Fan VS, Kaboli PJ. Geographic isolation and the risk for chronic obstructive pulmonary disease-related mortality: a cohort study. Ann Intern Med. 2011;155(2):80-86.
19. Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149-1155.
20. U.S. Department of Agriculture, Economic Research Service. Rural-urban commuting area codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx#U20K1F50H0A. Updated October 12, 2016. Accessed May 9, 2017.
21. Joo MJ, Lee TA, Weiss KB. Geographic variation of spirometry use in newly diagnosed COPD. Chest. 2008;134(1):38-45.
22. Damarla M, Celli BR, Mullerova HX, Pinto-Plata VM. Discrepancy in the use of confirmatory tests in patients hospitalized with the diagnosis of chronic obstructive pulmonary disease or congestive heart failure. Respir Care. 2006;51(10):1120-1124.
23. Grohskopf LA, Sokolow LZ, Olsen SJ, Bresee JS, Broder KR, Karron RA. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2015-16 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64(30):818-825.
24. Kim DK, Bridges CB, Harriman KH; Advisory Committee on Immunization Practices. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med. 2016;164(3):184-194.
25. Cimen P, Unlu M, Kirakli C, et al. Should patients with COPD be vaccinated? Respir Care. 2015;60(2):239-243.
26. Mowls DS, Cheruvu VK, Zullo MD. Influenza vaccination in adults with chronic obstructive pulmonary disease: the impact of a diagnostic breathing test on vaccination rates PLoS One. 2013;8(6):e67600.
27. Shoup JA, Madrid C, Koehler C, et al. Effectiveness and cost of influenza vaccine reminders for adults with asthma or chronic obstructive pulmonary disease. Am J Manag Care. 2015;21(7):e405-e413.
28. Arinez-Fernandez MC, Carrasco-Garrido P, Garcia-Carballo M, Hernandez-Barrera V, de Miguel AG, Jimenez-Garcia R. Determinants of pneumococcal vaccination among patients with chronic obstructive pulmonary disease in Spain. Hum Vaccin. 2006;2(3):99-104.29. Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
30. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012.
31. Goodridge D, Lawson J, Rennie D, Marciniuk D. Rural/urban differences in health care utilization and place of death for persons with respiratory illness in the last year of life. Rural Remote Health. 2010;10(2):1349.
32. Wang Y, Hu K, Liu K, et al. Obstructive sleep apnea exacerbates airway inflammation in patients with chronic obstructive pulmonary disease. Sleep Med. 2015;16(9):1123-1130.
33. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325-331