User login
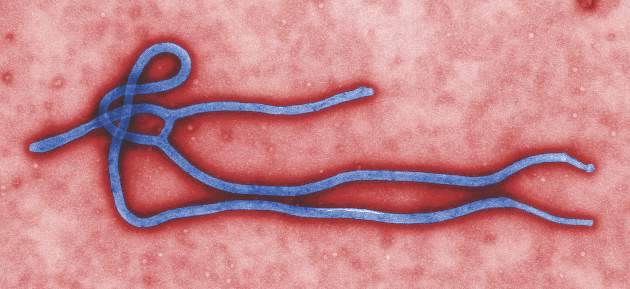
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
A new rapid diagnostic test for Ebola (RDT-Ebola) has been used to diagnose patients in Forécariah, Guinea. The National Ebola Coordination Cell implemented the test to enhance efforts to detect new Ebola cases and to ensure that such cases are not clinically misdiagnosed as malaria.
Jennifer Y. Huang and her associates found that among 13 sentinel sites during Oct. 1–Nov. 23, 2015, 1,544 (73%) of 2,115 consultations were for evaluation of febrile illness. Of those 1,544 consultations, 1,553 RDT-Malaria tests were reported to have been conducted and 1,000 RDT-Ebola tests were conducted. A total of 1,112 patients tested positive for malaria by RDT (the range of percentage of positive malaria tests among 13 sentinel sites was 52.3%-85.7%); none tested positive for Ebola by RDT-Ebola.
The ratio of RDT-Ebola to RDT-Malaria tests used was 0.64 overall and ranged from 0.27 to 1.00, according to the researchers.
Reported barriers to RDT-Ebola use – inadequate stock of RDT-Ebola kits, lack of understanding of the Centers for Disease Control and Prevention RDT-Ebola testing protocol, and patient refusal of RDT-Ebola testing – may have contributed to the differences in the numbers of malaria and Ebola tests conducted, the researchers wrote.
“Ongoing data collection from the sentinel sites can help to monitor the success of RDT-Ebola implementation, inform supply chain management, and identify and address barriers to RDT-Ebola use. RDT-Ebola implementation at the sentinel sites can also aid in screening for undetected Ebola cases to prevent establishment of new transmission chains,” the researchers concluded.
Find the study in Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6512a4).
FROM MMWR