User login
Diabetes mellitus (DM) is considered one of the most psychologically and behaviorally demanding chronic medical conditions. Patients with DM and serious mental illness (SMI), including schizophrenia, schizoaffective disorder, major depressive disorder (MDD), and bipolar disorder, are more likely to have poor adherence to medications as well as poor adherence to diet and lifestyle recommendations, which can lead to poor glycemic control, decreased quality of life, and increased health care expenses.1-4 Up to 27% of patients with DM have a depression diagnosis, and up to 60% of patients with DM experience depressive symptoms.5 Additionally, 1 in 4 patients with schizophrenia have a DM diagnosis.6 Serious mental illness can compromise DM self-management and glycemic control, which increases the risk of DM-related complications.7
These factors combine to make DM self-management essential for optimal glycemic control and prevention of DM-related complications. The American Diabetes Association recommends coordinated management of DM and SMI to achieve DM treatment targets.8 Interventions involving collaborative care teams have assisted in managing patients with concurrent SMI and DM. Collaborative interventions have reduced all-cause mortality, increased the number of patients reaching hemoglobin A1c (HbA1c) targets, increased overall improvement in HbA1c, increased rates of depression remission, and increased medication adherence.9-12
Background
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. A study by Desai and colleagues examined the relationship between psychiatric disorders and the quality of DM care in a national sample of veterans.7 Data were collected using chart-abstracted quality data from administrative database records for a sample of veterans with DM who had at least 3 outpatient visits in the previous year (n = 38,020). About 25% of the sample had a diagnosed psychiatric disorder, 91.5% of veterans completed an HbA1c test, and most veterans with a psychiatric disorder completed the 5 quality indicators for DM care (foot inspection, HbA1c determination, pedal pulses examination, foot sensory examination, and retina examination). Veterans with psychiatric disorders did not have a poorer quality of care for secondary prevention of DM compared with that of other veterans.7
In the PROSPECT study (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), a primary care-based depression management program assessed a collaborative intervention to improve care in patients with depression and DM.9 Fifteen depression care managers, including trained social workers, registered nurses (RNs), and psychologists, collaborated with primary care physicians (PCPs) to assist in recognizing depression, offer guideline-based treatment recommendations, and provide algorithm-based care, monitoring, and follow-up. After a median follow-up of 52 months, patients with depression and DM in the intervention group were less likely to die during the 5-year follow-up period compared with those in usual care (adjusted hazard ratio, 0.49 [95% confidence interval (CI), 0.24-0.98]). The study authors concluded that integrated depression care management significantly reduced all-cause mortality in patients with depression and DM.9
A single-blind, randomized, controlled trial conducted by Katon and colleagues examined patients with poorly controlled DM, coronary artery disease (CAD), or both, and concurrent depression in 14 primary care clinics (n = 214).10 The intervention consisted of nurse care managers who were trained RNs with experience in DM education and supervised by PCPs, providing guideline-based, collaborative care over 12 months to improve glycemic control, blood pressure (BP), and lipid control. The nurse care managers followed up with patients every 2 to3 weeks at office visits, and the intervention was compared with usual care by a physician. At 12 months, patients in the intervention group had significant improvement in HbA1c, low-density lipoprotein cholesterol, systolic BP, and depression compared with that of those under usual care. At 12 months, the HbA1c in the patients in the intervention group was significantly improved with an overall percentage change of 0.81 compared with 0.23 in the usual care group (estimated between-group difference, -0.56 [95% CI, -0.85 to -0.27]). The study authors concluded that integrated management and proactive follow-up of medical and psychological illnesses improved both medical outcomes and depression in patients with DM, CAD, or both.10
Another study by Bogner and colleagues investigated an integrated care intervention for patients with depression and DM to improve adherence to antidepressant and antidiabetic medications, glycemic control, and depression remission.11 Two trained research coordinators (a bachelor’s level and a master’s level) administered all intervention activities. The integrated care managers collaborated with physicians, offering education and guideline-based treatment recommendations to patients to monitor medication adherence and clinical status. The intervention supplemented regular primary care follow-up visits and was compared with usual care. At 12 weeks, patients in the integrated care group were more likely to achieve an HbA1c < 7% (60.9% vs 35.7%; P < .001) and remission of depression (58.7% vs 30.7%; P < .001) compared with those in usual care. There also was a significant improvement in adherence to DM and antidepressant medications in the intervention group compared with those in usual care during the study period.11
A systematic review and meta-analysis by Huang and colleagues assessed randomized controlled trials of collaborative care for diabetic patients with depression.12 Trials that reported depression treatment response, depression remission, HbA1c values, and adherence to antidepressant and/or hypoglycemic medications were included. A total of 8 trials randomized 2,238 patients with concurrent depression and DM and compared collaborative care with usual care. Collaborative care was associated with a significant increase in depression treatment response, reduction in HbA1c, and significant improvement in adherence rates for antidepressant and hypoglycemic medications compared with that of usual care. A reduction in HbA1c favored the collaborative care group; however, this reduction was not significant (mean difference, -0.13 [95% CI, -0.46 to 0.19]; P = .08 for heterogeneity; I2 = 51%). The study authors concluded that a collaborative care model significantly improved depression outcomes and adherence to medications in patients with concurrent DM and depression and recommended continued collaborative care for this population.12
Methods
The current study examines a novel service involving the collaboration of a registered nurse-certified DM educator (RN CDE) and clinical pharmacy specialist (PharmD) to improve access to care and maximize DM outcomes. The Louis Stokes Cleveland VAMC defines the PharmD scope of practice. One of the pharmacist’s clinical obligations includes serving as a preceptor for the RN CDE, a collaboration that has not been investigated in previous studies. A primary care provider (PCP) refers veterans to the RN CDE/PharmD clinic, with HbA1c ≥ 8%.
The RN CDE/PharmD clinic tends to receive referrals for the most challenging veterans who may have very elevated HbA1c readings, complex multidrug regimens, or basal/bolus insulin regimens. The RN CDE sees veterans in individual appointments and takes manual BP readings, checks point-of-care glucose/HbA1c readings, downloads home glucometer results into the electronic medical record (EMR), and provides education on DM management specific to the veteran’s individual needs. Because there is no established treatment algorithm for the RN CDE to follow, all medication changes are determined by a preceptor in real time.
When the RN CDE clinic was established, the RN CDE presented veterans to their PCP who determined the veteran’s plan of care. However, this plan was frustrating for the RN CDE because the PCP was not always readily available, causing delays in the workflow of the RN CDE clinic. Since the PharmD has a scope of practice and is more frequently available to discuss veteran cases, RN CDE/PharmD collaboration was initiated. Based on information gathered during the appointment, medication additions, titrations, and changes are precepted with the PharmD. Veterans can be seen in clinic every 2 to 4 weeks, allowing for continued medication adjustments if warranted until their HbA1c target is achieved. Veterans are discharged to their PCP once their HbA1c is at target.
Within the primary care clinic, this service was compared with usual care by a PCP and was associated with a clinically significant reduction in HbA1c by 2.5% compared with usual care after 1 year (P < .001).13 The same study population was investigated to determine whether there was a difference in glycemic control between veterans with SMI compared with veterans without SMI (non-SMI) to provide insight and better support for veterans with SMI and their DM care.
A retrospective review of the veterans referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014 was performed with institutional review board approval. Veterans were identified using a pharmacy-generated list searching for clinic note titles from the Computerized Patient Record System (CPRS).
The primary objective of this study was to determine the percentage change in mean HbA1c in veterans with SMI compared with that of veterans without SMI after referral to the RN CDE/PharmD clinic. The following secondary objectives also were investigated: the difference in the percentage of veterans with glycemic relapse after the intervention in veterans with SMI compared with that of veterans without SMI, and the difference in time to glycemic relapse between veterans with SMI compared with that of veterans without SMI. Serious mental illness was defined as schizophrenia, schizoaffective disorder, bipolar disorder, and MDD and identified in CPRS using ICD-9 and ICD-10 codes, medicine progress notes, and psychiatry progress notes. Glycemic relapse was defined as > 1% increase in HbA1c from the lowest HbA1c within 1 year of being followed by the RN CDE/PharmD clinic (nadir).
Veterans were included in the study if they were aged ≥ 18 years, referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014, had at least 2 clinic visits, an HbA1c > 8% at the date of the first clinic visit, and at least 1 HbA1c test at baseline and 1 HbA1c test at least 2 months after referral to the clinic. Veterans were excluded from the study if they met the following criteria: diagnosed with SMI during the study period, followed by the RN CDE or PharmD in other primary care clinics prior to referral, followed by the PharmD clinic within 365 days after the initial RN CDE/PharmD clinic visit, referred to or followed by endocrinology, or veterans enrolled in a VA DM research trial. Veterans continued to be enrolled until target enrollment was met.
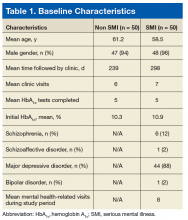
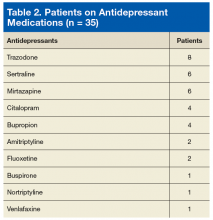
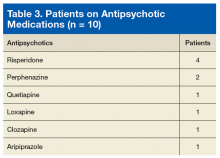
Medical records were reviewed to capture the following information: demographics (age and gender), type of SMI, date diagnosed with SMI, number of mental health-related visits, antidepressant and antipsychotic use, HbA1c prior to referral to the RN CDE/PharmD clinic (initial HbA1c) and date, HbA1c nadir and date, and highest postnadir HbA1c (glycemic relapse) and date, number of clinic visits, time followed by the clinic, and reason for glycemic relapse.
A total sample size of 100 veterans was needed to determine a medium effect size of 0.25 for between-group treatment effect on veterans with SMI compared with that of veterans without SMI, using a 2-group by 2 time-point repeated measures analysis of variance (ANOVA) with a power of 80% and alpha of 0.05. Of the 100 veterans, 50 veterans in each group were necessary to meet power. The percentage change in mean HbA1c from the initial time point to nadir was analyzed using a 2-time point by 2-group repeated measures ANOVA analysis. The secondary objectives were analyzed using descriptive statistics, a repeated measures ANOVA test to determine the percentage change in mean HbA1c from nadir to relapse, and an independent samples Student t test to analyze time to glycemic relapse.
Results
Discussion
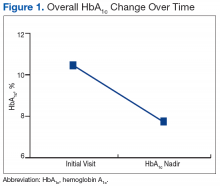
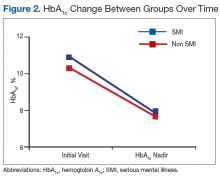
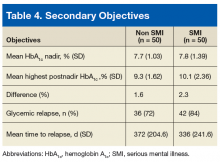
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. Although there was not a significant difference in mean HbA1c from the initial HbA1c to the nadir HbA1c between study groups, this study provided valuable insight for the RN CDE/PharmD clinic. The mean HbA1c decreased over time in both study groups, demonstrating that the collaborative intervention was effective in improving glycemic control in veterans with SMI and veterans without SMI. The mean HbA1c decrease in the SMI group was slightly higher compared with that of the non-SMI group, but the difference was not significant. The decrease in mean HbA1c also demonstrated that the RN CDE/PharmD interventions were effective in each group. Contrary to this study’s hypothesis that veterans with SMI would have worse glycemic control compared with that of veterans without SMI, this study demonstrated that there was no difference in glycemic control between groups.
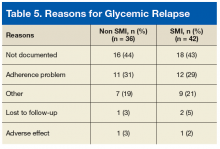
Veterans in the SMI group had a significantly greater percentage increase in mean HbA1c postnadir, indicating that their glycemic control worsened postnadir compared with that of the non-SMI group. If veterans with SMI relapsed, they tended to relapse to a greater extent compared with veterans without SMI, as indicated by a larger percentage increase in mean HbA1c. Time to relapse was shorter in veterans with SMI compared with that of veterans without SMI, but the difference was not significant. Using the information gathered, if veterans with SMI relapsed, they tended to relapse sooner and with a greater percentage increase in HbA1c compared with that of veterans without SMI.
Limitations
As a retrospective study, data collection was limited to the information found in the veteran’s EMR: Data collected were dependent on accurate and comprehensive documentation in the veteran’s problem list and progress notes. Additionally, the time between HbA1c tests was not analyzed when determining the differences in mean HbA1c. These data may be helpful in identifying reasons for glycemic relapse. Glycemic relapse depended on the number of HbA1c tests that the veteran completed. Time to glycemic relapse may occur sooner in veterans who completed more frequent HbA1c testing.
Conclusion
There was a significant decrease in mean HbA1c for the entire group over time. In comparing the percentage change in mean HbA1c between groups, there was not a significant difference in the decrease in mean HbA1c from initial to nadir HbA1c in veterans with SMI compared with that of veterans without SMI. However, veterans with SMI had a significantly larger increase in HbA1c postnadir compared with that of veterans without SMI, indicating that support would likely be needed after the veteran achieves his or her HbA1c target. Strategies such as extending the follow-up time in the RN CDE/PharmD clinic, expanding collaborative services with behavioral medicine and psychiatry, additional shared medical appointments or support groups for veterans with DM and SMI, and health literacy assessments may need to be adapted to assist in maintaining glycemic control in veterans with concurrent SMI and DM.
Click here to read the digital edition.
1. Razzano LA, Cook JA, Yost C, et al. Factors associated with co-occurring medical conditions among adults with serious mental disorders. Schizophr Res. 2015;161(2-3):458-464.
2. Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19(2):113-122.
3. Lustman PJ, Griffith LS, Freeland KE, Clouse RE. The course of major depression in diabetes. Gen Hosp Psychiatry. 1997;19(2):138-143.
4. Cox DJ, Gonder-Fredrick L. Major developments in behavioral diabetes research. J Consult Clin Psychol. 1992;60(4):628-638.
5. Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16(8):1167-1178.
6. Dixon L, Weiden P, Delahanty J, et al. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26(4):903-912.
7. Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the veterans health administration. Am J Psychiatry. 2002;159(9):1584-1590.
8. American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(suppl 1):S25-S43.
9. Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care. 2007;30(12):3005-3010.
10. Katon WJ, Lin EHB, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
11. Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10(1):15-22.
12. Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry. 2013;13(260):1-11.
13. James A, Leciejewski K, Pascuzzi K. Effect on diabetes care by a nurse certified diabetes educator with pharmacist support within a primary care clinic in a Veterans Affairs hospital. Abstract presented at: Ohio College of Clinical Pharmacy Spring Meeting; May 29, 2015; Cleveland, Ohio.
Diabetes mellitus (DM) is considered one of the most psychologically and behaviorally demanding chronic medical conditions. Patients with DM and serious mental illness (SMI), including schizophrenia, schizoaffective disorder, major depressive disorder (MDD), and bipolar disorder, are more likely to have poor adherence to medications as well as poor adherence to diet and lifestyle recommendations, which can lead to poor glycemic control, decreased quality of life, and increased health care expenses.1-4 Up to 27% of patients with DM have a depression diagnosis, and up to 60% of patients with DM experience depressive symptoms.5 Additionally, 1 in 4 patients with schizophrenia have a DM diagnosis.6 Serious mental illness can compromise DM self-management and glycemic control, which increases the risk of DM-related complications.7
These factors combine to make DM self-management essential for optimal glycemic control and prevention of DM-related complications. The American Diabetes Association recommends coordinated management of DM and SMI to achieve DM treatment targets.8 Interventions involving collaborative care teams have assisted in managing patients with concurrent SMI and DM. Collaborative interventions have reduced all-cause mortality, increased the number of patients reaching hemoglobin A1c (HbA1c) targets, increased overall improvement in HbA1c, increased rates of depression remission, and increased medication adherence.9-12
Background
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. A study by Desai and colleagues examined the relationship between psychiatric disorders and the quality of DM care in a national sample of veterans.7 Data were collected using chart-abstracted quality data from administrative database records for a sample of veterans with DM who had at least 3 outpatient visits in the previous year (n = 38,020). About 25% of the sample had a diagnosed psychiatric disorder, 91.5% of veterans completed an HbA1c test, and most veterans with a psychiatric disorder completed the 5 quality indicators for DM care (foot inspection, HbA1c determination, pedal pulses examination, foot sensory examination, and retina examination). Veterans with psychiatric disorders did not have a poorer quality of care for secondary prevention of DM compared with that of other veterans.7
In the PROSPECT study (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), a primary care-based depression management program assessed a collaborative intervention to improve care in patients with depression and DM.9 Fifteen depression care managers, including trained social workers, registered nurses (RNs), and psychologists, collaborated with primary care physicians (PCPs) to assist in recognizing depression, offer guideline-based treatment recommendations, and provide algorithm-based care, monitoring, and follow-up. After a median follow-up of 52 months, patients with depression and DM in the intervention group were less likely to die during the 5-year follow-up period compared with those in usual care (adjusted hazard ratio, 0.49 [95% confidence interval (CI), 0.24-0.98]). The study authors concluded that integrated depression care management significantly reduced all-cause mortality in patients with depression and DM.9
A single-blind, randomized, controlled trial conducted by Katon and colleagues examined patients with poorly controlled DM, coronary artery disease (CAD), or both, and concurrent depression in 14 primary care clinics (n = 214).10 The intervention consisted of nurse care managers who were trained RNs with experience in DM education and supervised by PCPs, providing guideline-based, collaborative care over 12 months to improve glycemic control, blood pressure (BP), and lipid control. The nurse care managers followed up with patients every 2 to3 weeks at office visits, and the intervention was compared with usual care by a physician. At 12 months, patients in the intervention group had significant improvement in HbA1c, low-density lipoprotein cholesterol, systolic BP, and depression compared with that of those under usual care. At 12 months, the HbA1c in the patients in the intervention group was significantly improved with an overall percentage change of 0.81 compared with 0.23 in the usual care group (estimated between-group difference, -0.56 [95% CI, -0.85 to -0.27]). The study authors concluded that integrated management and proactive follow-up of medical and psychological illnesses improved both medical outcomes and depression in patients with DM, CAD, or both.10
Another study by Bogner and colleagues investigated an integrated care intervention for patients with depression and DM to improve adherence to antidepressant and antidiabetic medications, glycemic control, and depression remission.11 Two trained research coordinators (a bachelor’s level and a master’s level) administered all intervention activities. The integrated care managers collaborated with physicians, offering education and guideline-based treatment recommendations to patients to monitor medication adherence and clinical status. The intervention supplemented regular primary care follow-up visits and was compared with usual care. At 12 weeks, patients in the integrated care group were more likely to achieve an HbA1c < 7% (60.9% vs 35.7%; P < .001) and remission of depression (58.7% vs 30.7%; P < .001) compared with those in usual care. There also was a significant improvement in adherence to DM and antidepressant medications in the intervention group compared with those in usual care during the study period.11
A systematic review and meta-analysis by Huang and colleagues assessed randomized controlled trials of collaborative care for diabetic patients with depression.12 Trials that reported depression treatment response, depression remission, HbA1c values, and adherence to antidepressant and/or hypoglycemic medications were included. A total of 8 trials randomized 2,238 patients with concurrent depression and DM and compared collaborative care with usual care. Collaborative care was associated with a significant increase in depression treatment response, reduction in HbA1c, and significant improvement in adherence rates for antidepressant and hypoglycemic medications compared with that of usual care. A reduction in HbA1c favored the collaborative care group; however, this reduction was not significant (mean difference, -0.13 [95% CI, -0.46 to 0.19]; P = .08 for heterogeneity; I2 = 51%). The study authors concluded that a collaborative care model significantly improved depression outcomes and adherence to medications in patients with concurrent DM and depression and recommended continued collaborative care for this population.12
Methods
The current study examines a novel service involving the collaboration of a registered nurse-certified DM educator (RN CDE) and clinical pharmacy specialist (PharmD) to improve access to care and maximize DM outcomes. The Louis Stokes Cleveland VAMC defines the PharmD scope of practice. One of the pharmacist’s clinical obligations includes serving as a preceptor for the RN CDE, a collaboration that has not been investigated in previous studies. A primary care provider (PCP) refers veterans to the RN CDE/PharmD clinic, with HbA1c ≥ 8%.
The RN CDE/PharmD clinic tends to receive referrals for the most challenging veterans who may have very elevated HbA1c readings, complex multidrug regimens, or basal/bolus insulin regimens. The RN CDE sees veterans in individual appointments and takes manual BP readings, checks point-of-care glucose/HbA1c readings, downloads home glucometer results into the electronic medical record (EMR), and provides education on DM management specific to the veteran’s individual needs. Because there is no established treatment algorithm for the RN CDE to follow, all medication changes are determined by a preceptor in real time.
When the RN CDE clinic was established, the RN CDE presented veterans to their PCP who determined the veteran’s plan of care. However, this plan was frustrating for the RN CDE because the PCP was not always readily available, causing delays in the workflow of the RN CDE clinic. Since the PharmD has a scope of practice and is more frequently available to discuss veteran cases, RN CDE/PharmD collaboration was initiated. Based on information gathered during the appointment, medication additions, titrations, and changes are precepted with the PharmD. Veterans can be seen in clinic every 2 to 4 weeks, allowing for continued medication adjustments if warranted until their HbA1c target is achieved. Veterans are discharged to their PCP once their HbA1c is at target.
Within the primary care clinic, this service was compared with usual care by a PCP and was associated with a clinically significant reduction in HbA1c by 2.5% compared with usual care after 1 year (P < .001).13 The same study population was investigated to determine whether there was a difference in glycemic control between veterans with SMI compared with veterans without SMI (non-SMI) to provide insight and better support for veterans with SMI and their DM care.
A retrospective review of the veterans referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014 was performed with institutional review board approval. Veterans were identified using a pharmacy-generated list searching for clinic note titles from the Computerized Patient Record System (CPRS).
The primary objective of this study was to determine the percentage change in mean HbA1c in veterans with SMI compared with that of veterans without SMI after referral to the RN CDE/PharmD clinic. The following secondary objectives also were investigated: the difference in the percentage of veterans with glycemic relapse after the intervention in veterans with SMI compared with that of veterans without SMI, and the difference in time to glycemic relapse between veterans with SMI compared with that of veterans without SMI. Serious mental illness was defined as schizophrenia, schizoaffective disorder, bipolar disorder, and MDD and identified in CPRS using ICD-9 and ICD-10 codes, medicine progress notes, and psychiatry progress notes. Glycemic relapse was defined as > 1% increase in HbA1c from the lowest HbA1c within 1 year of being followed by the RN CDE/PharmD clinic (nadir).
Veterans were included in the study if they were aged ≥ 18 years, referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014, had at least 2 clinic visits, an HbA1c > 8% at the date of the first clinic visit, and at least 1 HbA1c test at baseline and 1 HbA1c test at least 2 months after referral to the clinic. Veterans were excluded from the study if they met the following criteria: diagnosed with SMI during the study period, followed by the RN CDE or PharmD in other primary care clinics prior to referral, followed by the PharmD clinic within 365 days after the initial RN CDE/PharmD clinic visit, referred to or followed by endocrinology, or veterans enrolled in a VA DM research trial. Veterans continued to be enrolled until target enrollment was met.
Medical records were reviewed to capture the following information: demographics (age and gender), type of SMI, date diagnosed with SMI, number of mental health-related visits, antidepressant and antipsychotic use, HbA1c prior to referral to the RN CDE/PharmD clinic (initial HbA1c) and date, HbA1c nadir and date, and highest postnadir HbA1c (glycemic relapse) and date, number of clinic visits, time followed by the clinic, and reason for glycemic relapse.
A total sample size of 100 veterans was needed to determine a medium effect size of 0.25 for between-group treatment effect on veterans with SMI compared with that of veterans without SMI, using a 2-group by 2 time-point repeated measures analysis of variance (ANOVA) with a power of 80% and alpha of 0.05. Of the 100 veterans, 50 veterans in each group were necessary to meet power. The percentage change in mean HbA1c from the initial time point to nadir was analyzed using a 2-time point by 2-group repeated measures ANOVA analysis. The secondary objectives were analyzed using descriptive statistics, a repeated measures ANOVA test to determine the percentage change in mean HbA1c from nadir to relapse, and an independent samples Student t test to analyze time to glycemic relapse.
Results
Discussion
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. Although there was not a significant difference in mean HbA1c from the initial HbA1c to the nadir HbA1c between study groups, this study provided valuable insight for the RN CDE/PharmD clinic. The mean HbA1c decreased over time in both study groups, demonstrating that the collaborative intervention was effective in improving glycemic control in veterans with SMI and veterans without SMI. The mean HbA1c decrease in the SMI group was slightly higher compared with that of the non-SMI group, but the difference was not significant. The decrease in mean HbA1c also demonstrated that the RN CDE/PharmD interventions were effective in each group. Contrary to this study’s hypothesis that veterans with SMI would have worse glycemic control compared with that of veterans without SMI, this study demonstrated that there was no difference in glycemic control between groups.
Veterans in the SMI group had a significantly greater percentage increase in mean HbA1c postnadir, indicating that their glycemic control worsened postnadir compared with that of the non-SMI group. If veterans with SMI relapsed, they tended to relapse to a greater extent compared with veterans without SMI, as indicated by a larger percentage increase in mean HbA1c. Time to relapse was shorter in veterans with SMI compared with that of veterans without SMI, but the difference was not significant. Using the information gathered, if veterans with SMI relapsed, they tended to relapse sooner and with a greater percentage increase in HbA1c compared with that of veterans without SMI.
Limitations
As a retrospective study, data collection was limited to the information found in the veteran’s EMR: Data collected were dependent on accurate and comprehensive documentation in the veteran’s problem list and progress notes. Additionally, the time between HbA1c tests was not analyzed when determining the differences in mean HbA1c. These data may be helpful in identifying reasons for glycemic relapse. Glycemic relapse depended on the number of HbA1c tests that the veteran completed. Time to glycemic relapse may occur sooner in veterans who completed more frequent HbA1c testing.
Conclusion
There was a significant decrease in mean HbA1c for the entire group over time. In comparing the percentage change in mean HbA1c between groups, there was not a significant difference in the decrease in mean HbA1c from initial to nadir HbA1c in veterans with SMI compared with that of veterans without SMI. However, veterans with SMI had a significantly larger increase in HbA1c postnadir compared with that of veterans without SMI, indicating that support would likely be needed after the veteran achieves his or her HbA1c target. Strategies such as extending the follow-up time in the RN CDE/PharmD clinic, expanding collaborative services with behavioral medicine and psychiatry, additional shared medical appointments or support groups for veterans with DM and SMI, and health literacy assessments may need to be adapted to assist in maintaining glycemic control in veterans with concurrent SMI and DM.
Click here to read the digital edition.
Diabetes mellitus (DM) is considered one of the most psychologically and behaviorally demanding chronic medical conditions. Patients with DM and serious mental illness (SMI), including schizophrenia, schizoaffective disorder, major depressive disorder (MDD), and bipolar disorder, are more likely to have poor adherence to medications as well as poor adherence to diet and lifestyle recommendations, which can lead to poor glycemic control, decreased quality of life, and increased health care expenses.1-4 Up to 27% of patients with DM have a depression diagnosis, and up to 60% of patients with DM experience depressive symptoms.5 Additionally, 1 in 4 patients with schizophrenia have a DM diagnosis.6 Serious mental illness can compromise DM self-management and glycemic control, which increases the risk of DM-related complications.7
These factors combine to make DM self-management essential for optimal glycemic control and prevention of DM-related complications. The American Diabetes Association recommends coordinated management of DM and SMI to achieve DM treatment targets.8 Interventions involving collaborative care teams have assisted in managing patients with concurrent SMI and DM. Collaborative interventions have reduced all-cause mortality, increased the number of patients reaching hemoglobin A1c (HbA1c) targets, increased overall improvement in HbA1c, increased rates of depression remission, and increased medication adherence.9-12
Background
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. A study by Desai and colleagues examined the relationship between psychiatric disorders and the quality of DM care in a national sample of veterans.7 Data were collected using chart-abstracted quality data from administrative database records for a sample of veterans with DM who had at least 3 outpatient visits in the previous year (n = 38,020). About 25% of the sample had a diagnosed psychiatric disorder, 91.5% of veterans completed an HbA1c test, and most veterans with a psychiatric disorder completed the 5 quality indicators for DM care (foot inspection, HbA1c determination, pedal pulses examination, foot sensory examination, and retina examination). Veterans with psychiatric disorders did not have a poorer quality of care for secondary prevention of DM compared with that of other veterans.7
In the PROSPECT study (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), a primary care-based depression management program assessed a collaborative intervention to improve care in patients with depression and DM.9 Fifteen depression care managers, including trained social workers, registered nurses (RNs), and psychologists, collaborated with primary care physicians (PCPs) to assist in recognizing depression, offer guideline-based treatment recommendations, and provide algorithm-based care, monitoring, and follow-up. After a median follow-up of 52 months, patients with depression and DM in the intervention group were less likely to die during the 5-year follow-up period compared with those in usual care (adjusted hazard ratio, 0.49 [95% confidence interval (CI), 0.24-0.98]). The study authors concluded that integrated depression care management significantly reduced all-cause mortality in patients with depression and DM.9
A single-blind, randomized, controlled trial conducted by Katon and colleagues examined patients with poorly controlled DM, coronary artery disease (CAD), or both, and concurrent depression in 14 primary care clinics (n = 214).10 The intervention consisted of nurse care managers who were trained RNs with experience in DM education and supervised by PCPs, providing guideline-based, collaborative care over 12 months to improve glycemic control, blood pressure (BP), and lipid control. The nurse care managers followed up with patients every 2 to3 weeks at office visits, and the intervention was compared with usual care by a physician. At 12 months, patients in the intervention group had significant improvement in HbA1c, low-density lipoprotein cholesterol, systolic BP, and depression compared with that of those under usual care. At 12 months, the HbA1c in the patients in the intervention group was significantly improved with an overall percentage change of 0.81 compared with 0.23 in the usual care group (estimated between-group difference, -0.56 [95% CI, -0.85 to -0.27]). The study authors concluded that integrated management and proactive follow-up of medical and psychological illnesses improved both medical outcomes and depression in patients with DM, CAD, or both.10
Another study by Bogner and colleagues investigated an integrated care intervention for patients with depression and DM to improve adherence to antidepressant and antidiabetic medications, glycemic control, and depression remission.11 Two trained research coordinators (a bachelor’s level and a master’s level) administered all intervention activities. The integrated care managers collaborated with physicians, offering education and guideline-based treatment recommendations to patients to monitor medication adherence and clinical status. The intervention supplemented regular primary care follow-up visits and was compared with usual care. At 12 weeks, patients in the integrated care group were more likely to achieve an HbA1c < 7% (60.9% vs 35.7%; P < .001) and remission of depression (58.7% vs 30.7%; P < .001) compared with those in usual care. There also was a significant improvement in adherence to DM and antidepressant medications in the intervention group compared with those in usual care during the study period.11
A systematic review and meta-analysis by Huang and colleagues assessed randomized controlled trials of collaborative care for diabetic patients with depression.12 Trials that reported depression treatment response, depression remission, HbA1c values, and adherence to antidepressant and/or hypoglycemic medications were included. A total of 8 trials randomized 2,238 patients with concurrent depression and DM and compared collaborative care with usual care. Collaborative care was associated with a significant increase in depression treatment response, reduction in HbA1c, and significant improvement in adherence rates for antidepressant and hypoglycemic medications compared with that of usual care. A reduction in HbA1c favored the collaborative care group; however, this reduction was not significant (mean difference, -0.13 [95% CI, -0.46 to 0.19]; P = .08 for heterogeneity; I2 = 51%). The study authors concluded that a collaborative care model significantly improved depression outcomes and adherence to medications in patients with concurrent DM and depression and recommended continued collaborative care for this population.12
Methods
The current study examines a novel service involving the collaboration of a registered nurse-certified DM educator (RN CDE) and clinical pharmacy specialist (PharmD) to improve access to care and maximize DM outcomes. The Louis Stokes Cleveland VAMC defines the PharmD scope of practice. One of the pharmacist’s clinical obligations includes serving as a preceptor for the RN CDE, a collaboration that has not been investigated in previous studies. A primary care provider (PCP) refers veterans to the RN CDE/PharmD clinic, with HbA1c ≥ 8%.
The RN CDE/PharmD clinic tends to receive referrals for the most challenging veterans who may have very elevated HbA1c readings, complex multidrug regimens, or basal/bolus insulin regimens. The RN CDE sees veterans in individual appointments and takes manual BP readings, checks point-of-care glucose/HbA1c readings, downloads home glucometer results into the electronic medical record (EMR), and provides education on DM management specific to the veteran’s individual needs. Because there is no established treatment algorithm for the RN CDE to follow, all medication changes are determined by a preceptor in real time.
When the RN CDE clinic was established, the RN CDE presented veterans to their PCP who determined the veteran’s plan of care. However, this plan was frustrating for the RN CDE because the PCP was not always readily available, causing delays in the workflow of the RN CDE clinic. Since the PharmD has a scope of practice and is more frequently available to discuss veteran cases, RN CDE/PharmD collaboration was initiated. Based on information gathered during the appointment, medication additions, titrations, and changes are precepted with the PharmD. Veterans can be seen in clinic every 2 to 4 weeks, allowing for continued medication adjustments if warranted until their HbA1c target is achieved. Veterans are discharged to their PCP once their HbA1c is at target.
Within the primary care clinic, this service was compared with usual care by a PCP and was associated with a clinically significant reduction in HbA1c by 2.5% compared with usual care after 1 year (P < .001).13 The same study population was investigated to determine whether there was a difference in glycemic control between veterans with SMI compared with veterans without SMI (non-SMI) to provide insight and better support for veterans with SMI and their DM care.
A retrospective review of the veterans referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014 was performed with institutional review board approval. Veterans were identified using a pharmacy-generated list searching for clinic note titles from the Computerized Patient Record System (CPRS).
The primary objective of this study was to determine the percentage change in mean HbA1c in veterans with SMI compared with that of veterans without SMI after referral to the RN CDE/PharmD clinic. The following secondary objectives also were investigated: the difference in the percentage of veterans with glycemic relapse after the intervention in veterans with SMI compared with that of veterans without SMI, and the difference in time to glycemic relapse between veterans with SMI compared with that of veterans without SMI. Serious mental illness was defined as schizophrenia, schizoaffective disorder, bipolar disorder, and MDD and identified in CPRS using ICD-9 and ICD-10 codes, medicine progress notes, and psychiatry progress notes. Glycemic relapse was defined as > 1% increase in HbA1c from the lowest HbA1c within 1 year of being followed by the RN CDE/PharmD clinic (nadir).
Veterans were included in the study if they were aged ≥ 18 years, referred to the RN CDE/PharmD clinic from January 1, 2011 to December 31, 2014, had at least 2 clinic visits, an HbA1c > 8% at the date of the first clinic visit, and at least 1 HbA1c test at baseline and 1 HbA1c test at least 2 months after referral to the clinic. Veterans were excluded from the study if they met the following criteria: diagnosed with SMI during the study period, followed by the RN CDE or PharmD in other primary care clinics prior to referral, followed by the PharmD clinic within 365 days after the initial RN CDE/PharmD clinic visit, referred to or followed by endocrinology, or veterans enrolled in a VA DM research trial. Veterans continued to be enrolled until target enrollment was met.
Medical records were reviewed to capture the following information: demographics (age and gender), type of SMI, date diagnosed with SMI, number of mental health-related visits, antidepressant and antipsychotic use, HbA1c prior to referral to the RN CDE/PharmD clinic (initial HbA1c) and date, HbA1c nadir and date, and highest postnadir HbA1c (glycemic relapse) and date, number of clinic visits, time followed by the clinic, and reason for glycemic relapse.
A total sample size of 100 veterans was needed to determine a medium effect size of 0.25 for between-group treatment effect on veterans with SMI compared with that of veterans without SMI, using a 2-group by 2 time-point repeated measures analysis of variance (ANOVA) with a power of 80% and alpha of 0.05. Of the 100 veterans, 50 veterans in each group were necessary to meet power. The percentage change in mean HbA1c from the initial time point to nadir was analyzed using a 2-time point by 2-group repeated measures ANOVA analysis. The secondary objectives were analyzed using descriptive statistics, a repeated measures ANOVA test to determine the percentage change in mean HbA1c from nadir to relapse, and an independent samples Student t test to analyze time to glycemic relapse.
Results
Discussion
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. Although there was not a significant difference in mean HbA1c from the initial HbA1c to the nadir HbA1c between study groups, this study provided valuable insight for the RN CDE/PharmD clinic. The mean HbA1c decreased over time in both study groups, demonstrating that the collaborative intervention was effective in improving glycemic control in veterans with SMI and veterans without SMI. The mean HbA1c decrease in the SMI group was slightly higher compared with that of the non-SMI group, but the difference was not significant. The decrease in mean HbA1c also demonstrated that the RN CDE/PharmD interventions were effective in each group. Contrary to this study’s hypothesis that veterans with SMI would have worse glycemic control compared with that of veterans without SMI, this study demonstrated that there was no difference in glycemic control between groups.
Veterans in the SMI group had a significantly greater percentage increase in mean HbA1c postnadir, indicating that their glycemic control worsened postnadir compared with that of the non-SMI group. If veterans with SMI relapsed, they tended to relapse to a greater extent compared with veterans without SMI, as indicated by a larger percentage increase in mean HbA1c. Time to relapse was shorter in veterans with SMI compared with that of veterans without SMI, but the difference was not significant. Using the information gathered, if veterans with SMI relapsed, they tended to relapse sooner and with a greater percentage increase in HbA1c compared with that of veterans without SMI.
Limitations
As a retrospective study, data collection was limited to the information found in the veteran’s EMR: Data collected were dependent on accurate and comprehensive documentation in the veteran’s problem list and progress notes. Additionally, the time between HbA1c tests was not analyzed when determining the differences in mean HbA1c. These data may be helpful in identifying reasons for glycemic relapse. Glycemic relapse depended on the number of HbA1c tests that the veteran completed. Time to glycemic relapse may occur sooner in veterans who completed more frequent HbA1c testing.
Conclusion
There was a significant decrease in mean HbA1c for the entire group over time. In comparing the percentage change in mean HbA1c between groups, there was not a significant difference in the decrease in mean HbA1c from initial to nadir HbA1c in veterans with SMI compared with that of veterans without SMI. However, veterans with SMI had a significantly larger increase in HbA1c postnadir compared with that of veterans without SMI, indicating that support would likely be needed after the veteran achieves his or her HbA1c target. Strategies such as extending the follow-up time in the RN CDE/PharmD clinic, expanding collaborative services with behavioral medicine and psychiatry, additional shared medical appointments or support groups for veterans with DM and SMI, and health literacy assessments may need to be adapted to assist in maintaining glycemic control in veterans with concurrent SMI and DM.
Click here to read the digital edition.
1. Razzano LA, Cook JA, Yost C, et al. Factors associated with co-occurring medical conditions among adults with serious mental disorders. Schizophr Res. 2015;161(2-3):458-464.
2. Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19(2):113-122.
3. Lustman PJ, Griffith LS, Freeland KE, Clouse RE. The course of major depression in diabetes. Gen Hosp Psychiatry. 1997;19(2):138-143.
4. Cox DJ, Gonder-Fredrick L. Major developments in behavioral diabetes research. J Consult Clin Psychol. 1992;60(4):628-638.
5. Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16(8):1167-1178.
6. Dixon L, Weiden P, Delahanty J, et al. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26(4):903-912.
7. Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the veterans health administration. Am J Psychiatry. 2002;159(9):1584-1590.
8. American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(suppl 1):S25-S43.
9. Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care. 2007;30(12):3005-3010.
10. Katon WJ, Lin EHB, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
11. Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10(1):15-22.
12. Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry. 2013;13(260):1-11.
13. James A, Leciejewski K, Pascuzzi K. Effect on diabetes care by a nurse certified diabetes educator with pharmacist support within a primary care clinic in a Veterans Affairs hospital. Abstract presented at: Ohio College of Clinical Pharmacy Spring Meeting; May 29, 2015; Cleveland, Ohio.
1. Razzano LA, Cook JA, Yost C, et al. Factors associated with co-occurring medical conditions among adults with serious mental disorders. Schizophr Res. 2015;161(2-3):458-464.
2. Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19(2):113-122.
3. Lustman PJ, Griffith LS, Freeland KE, Clouse RE. The course of major depression in diabetes. Gen Hosp Psychiatry. 1997;19(2):138-143.
4. Cox DJ, Gonder-Fredrick L. Major developments in behavioral diabetes research. J Consult Clin Psychol. 1992;60(4):628-638.
5. Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16(8):1167-1178.
6. Dixon L, Weiden P, Delahanty J, et al. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26(4):903-912.
7. Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the veterans health administration. Am J Psychiatry. 2002;159(9):1584-1590.
8. American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(suppl 1):S25-S43.
9. Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care. 2007;30(12):3005-3010.
10. Katon WJ, Lin EHB, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
11. Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10(1):15-22.
12. Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry. 2013;13(260):1-11.
13. James A, Leciejewski K, Pascuzzi K. Effect on diabetes care by a nurse certified diabetes educator with pharmacist support within a primary care clinic in a Veterans Affairs hospital. Abstract presented at: Ohio College of Clinical Pharmacy Spring Meeting; May 29, 2015; Cleveland, Ohio.