User login
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
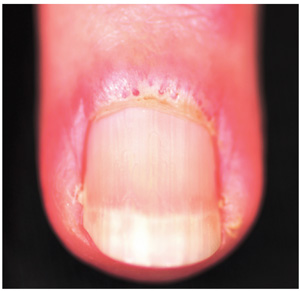
A three-month history of muscle weakness, fatigue, and skin changes prompts a 59-year-old woman to self-refer to dermatology. Otherwise healthy prior to the onset of these symptoms, she has had to take a leave of absence from work due to her inability to carry out her duties, which include light lifting and prolonged periods of time on her feet as a clerk in a pharmacy. She first consulted her primary care provider (PCP), who informed her that she was not anemic and did not have thyroid disease; the PCP felt that stress was probably a factor. She then purchased a number of products from her health food store, which she started taking until the skin on her hands began to change. On examination, atrophic pinkish red planar plaques are noted on 10/10 fingers, confined to the dorsal aspects of her joints and sharply sparing the interphalangeal spaces. The cuticles demonstrate the presence of dilated and irregularly shaped capillary loops. Several of her cuticles are also overgrown and frayed. Examination of the rest of the patient’s skin reveals a blanchable, faintly sunburned appearance to her anterior neck.
