User login
Sleep-disordered breathing (SDB) is a continuum of symptoms that range from primary snoring with upper airway resistance to frank obstruction seen in obstructive sleep apnea (OSA). This disease spectrum has been reported to affect 10% to 17% of men and 3% to 9% of women in the general population.1 The specific incidence of OSA has been estimated to be about 2% to 4% of the general adult population.2,3 Sleep-disordered breathing often leads to poor sleep quality, which has been associated with many medical comorbidities, including vascular disease, hypertension, major cardiac events, cardiomyopathies, impaired concentration, reduced psychomotor vigilance and cognition, and daytime somnolence.1,2,4-6 Furthermore, there is evidence that the prevalence of SDB continues to grow among the general population.1 However, the prevalence of SDB in various populations (eg, pediatric vs adult, varying body mass index, country of origin) varies widely due to the multifactorial nature of the risk factors and the difficulty in diagnosing SDB.
Some of the more intuitive medical sequelae of SDB are daytime somnolence and subsequent impaired concentration for those with disrupted sleep patterns. Medical literature has paid specific attention to cohorts of personnel who may be at heightened risk from impaired concentration or inability to focus. These populations include but are not limited to sleep-deprived resident physicians, firefighters, truck drivers, and heavy-machine operators.7,8
Military service members represent a distinct cohort that often is relied on to maintain vigilance even in austere environments. Concentration is paramount in order to perform combat operations or tasks that involve operating heavy machinery, such as nuclear submarines, aircraft, or tanks. Given the myriad of unique operational demands on service members, SDB can have detrimental consequences on an individual’s health and his or her military readiness and training. Ultimately, SDB may degrade a unit’s effectiveness and perhaps the country’s military capability.
Active-duty military service members seem to be more susceptible to clinically relevant sleep conditions. In the military, causes of disruptions in normal sleep patterns are multifactorial. Medical literature focuses on circadian disruptions due to shift work and frequent travel, frequent alternating use of caffeine and sedatives, exposure to combat/trauma, and chronic sleep deprivation.9-11 Studies have been published that focus on service members who have returned from combat deployment.10,12,13 However, these studies do not explore the overall burden of disease, and there are no specific data to suggest the prevalence, annual incidence, or associated costs.
To quantify this disease burden in the military, this study focused on the subset of sleep disorders that impact respiration during sleep and determined the prevalence and annual incidence for the entire active-duty population. Additionally, the authors fill a void in the literature by determining the financial burden of SDB on civilian care expenditures.
Methods
This study was a retrospective review of administrative military health care data spanning fiscal years (FYs) 2009 to 2013 (October 1, 2008 to September 30, 2013). The study protocol was approved by the Naval Medical Center Portsmouth Institutional Review Board, and approval was given to waive informed consent. The Health Analysis Department at the Navy and Marine Corps Public Health Center (NMCPHC) obtained and analyzed data from the Military Health System (MHS) Management Analysis and Reporting Tool (M2). The M2 system is an ad hoc query tool used for viewing population, clinical, and financial MHS data, including care received within military treatment facilities (MTFs) and care purchased through TRICARE at civilian facilities. Both inpatient and outpatient health care records were included.
The population included all active-duty service members and guard/reserve members on active duty within all military services, including air force, army, coast guard, and navy branches, between FY 2009 and FY 2013. The authors identified service members with SDB as those with at least 1 ICD-9 diagnosis code related to SDB: obstructive sleep apnea (327.23); sleep-related hypoventilation/hypoxemia (327.26); and other organic sleep disorder (327.80).
Due to the transient nature of the military population, a monthly average over the 5 years of the study determined the overall number of service members eligible for care (1,717,227 service members).
Data Analysis
Prevalence of diagnosed SDB per FY was calculated as the number of service members who received at least 1 SDB diagnostic code between October 1, 2008 and September 30, 2013, over the average total active-duty population. Incidence per year was calculated as the number of new cases per FY, using 2009 as the baseline. Data were stratified by demographic and enrollment information for diagnosed service members and analyzed using SAS 9.4 (Cary, NC) software.
Direct costs associated with SDB treatment fall into 2 categories for service members: (1) care delivered by civilian providers, calculated based on the amount TRICARE paid for the service, using insurance claim data; and (2) care received at MTFs by military providers. Costs for care at MTFs cannot be calculated, as the total cost amount for a single record is not directly attributed to SDB diagnosis.
Results
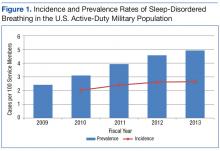
A total of 197,183 service members were diagnosed with SDB from FY 2009 to FY 2013. Both the annual incidence and prevalence of SDB for the active-duty military population showed upward trends for each of the years evaluated (Figure 1).
Notably, 72% of service members seen for SDB ranged in age from 25 to 44 years (Table).
Discussion
This study shows that the prevalence and incidence of SDB in the active-duty population are less than those reported for the civilian populace as a whole but are still greater than expected for an otherwise healthy and young population. Furthermore, the burden of disease and the cost to diagnose and treat have steadily increased for each of the past 5 fiscal years that were assessed.
The data show an upward trend in the incidence and prevalence of SDB in the military from FY 2009 to FY 2013 for reasons that are not clear but likely with many confounding contributions. As the spectrum of SDB has become better defined and the detrimental sequelae are better understood, it is likely that both service members and health care providers are more aware of the symptoms and more importantly, the potential for interventions that improve quality of life. It is also important to note that the U.S. military is a very transient organization with a nearly constant turnover between new enlistees/officers and those leaving the service or retiring after 20 years of service. Thus, despite an annual incidence of nearly 3% throughout the years evaluated, the annual increase in prevalence is not necessarily commensurate.
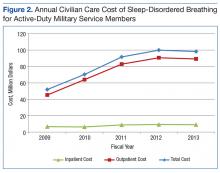
The FY 2013 prevalence (4.2%) and civilian care costs ($98,259,519) present traditional indications of the disease burden. Both metrics represent a sizable and increasing disease burden for the military. It is also important to note that these costs reflect only the short-term expenses for initial diagnosis and therapy. These costs in no way reflect the care for the long-term medical sequelae that have been recently linked to uncontrolled SDB/OSA, such as heart and vascular diseases, hypertension, and increased stroke risk. Additional costs will continue to grow.
Perhaps the most validated predictive factor for diagnosis of SDB or OSA is body habitus as measured by body mass index (BMI). In particular, nearly 60% to 90% of patients with OSA are obese.2 Weight gain seems to increase the OSA severity, whereas losing weight decreases it.14-16 Although the U.S. military employs height and weight standards that preclude those with persistently overweight or obese BMIs from continued service, these standards often are not rigid, and there are overweight or even obese active-duty members. Interestingly, despite a population that essentially controls for the most predictive risk factor, the prevalence of SDB is still approximately 1 in 20 (4.9%) in FY 2013.
Given the significant burden of disease represented by the incidence, prevalence, and cost data determined in this study and the growing recognition of long-term complications from poorly controlled SDB, it has become evident that more efficacious interventions are needed. Modern treatments for SDB can be classified as surgical or nonsurgical but with no single modality fitting the need for all patients secondary to poor adherence and/or limited efficacy.17-20 However, to mitigate the impact on military readiness and taxpayer-funded health care costs, it may be appropriate to begin exploring therapeutic options beyond the current standard of care. For example, an invasive and costly onetime surgical intervention using an implantable device to stimulate the hypoglossal nerve to open a person’s airway during inspiration is being investigated in a younger, nonobese cohort of patients.21 Further research is warranted into this specific model of therapeutic intervention and others for service members.
Limitations
Limitations in this study include possible reporting errors due to improper or insufficient medical coding as well as data entry errors at the clinic that may exist within medical billing databases. Therefore, the results of this analysis may be over- or underrepresented. The increase in incidence and prevalence may not necessarily reflect an increasing number of people who have the disease. The increase could be a result of better SDB detection practices or incentives to be diagnosed with SDB (VA disability claims upon retirement). The assumption is made that procedures corresponding with SDB diagnoses are directly related to SDB, and any costs incurred from those procedures are due to SDB.
It is important to note variability between services and institutions within the DoD in the diagnosis and treatment of SDB. Specifically, some institutions use ambulatory polysomnograms, or studies done at home, and autotitration of continuous positive airway pressure, whereas others require more costly hospital-based studies and laboratory titration. Another confounder in the cost data is the number of diagnoses and treatment deferred to the network as a result of the relatively small number of sleep-trained physicians within the military.
Conclusion
As the field of sleep medicine continues to develop its literature, it is becoming clearer that the detrimental sequelae of SDB are varied and pose significant short- and long-term risks. Active-duty service members represent a subset of the population with consequences that are potentially graver than those of civilians, especially when they are expected to operate complicated machinery or to make rapid and critical decisions in battle.
The prevalence and incidence of SDB increased each year during a 5-year review and currently affects 1 in 20 service members. Furthermore, the cost of civilian care for this disease process was nearly $100 million in FY 2012 to FY 2013, suggesting a growing financial burden for taxpayers. Further research is warranted to fully appreciate the impact of SDB on both service members and the U.S. military.
Acknowledgments
The authors thank the U.S. Navy and specifically the support within the Department of Otolaryngology at the Naval Medical Center Portsmouth for the time and effort allotted for completion of this study. This research was supported in part by an appointment to the Postgraduate Research Participation Program at the Navy and Marine Corps Public Health Center (NMCPHC) administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and NMCPHC.
1. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014.
2. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-1239.
3. Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14(1):63-70.
4. Kim H, Dinges DF, Young T. Sleep-disordered breathing and psychomotor vigilance in a community-based sample. Sleep. 2007;30(10):1309-1316.
5. Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017-1028.
6. Gilat H, Vinker S, Buda I, Soudry E, Shani M, Bachar G. Obstructive sleep apnea and cardiovascular comorbidities: a large epidemiologic study. Medicine (Baltimore). 2014;93(9):e45.
7. Li X, Sundquist K, Sundquist J. Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med. 2008;9(2):129-136.
8. Barger LK, Rajaratnam SM, Wang W, et al. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J Clin Sleep Med. 2015;11(3):233-240.
9. Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549-557.
10. Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167-174.
11. Capaldi VF 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med. 2011;176(8):879-888.
12. Collen J, Orr N, Lettieri CJ, Carter K, Holley AB. Sleep disturbances among soldiers with combat-related traumatic brain injury. Chest. 2012;142(3):622-630.
13. Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173(3):230-235.
14. Dixon JB, Schachter LM, O’Brien PE. Polysomnography before and after weight loss in obese patients with severe sleep apnea. Int J Obes (Lond). 2005;29(9):1048-1054.
15. Loube DI, Loube AA, Erman MK. Continuous positive airway pressure treatment results in weight less in obese and overweight patients with obstructive sleep apnea. J Am Diet Assoc. 1997;97(8):896-897.
16. Loube DI, Loube AA, Mitler MM. Weight loss for obstructive sleep apnea: the optimal therapy for obese patients. J Am Diet Assoc. 1994;94(11):1291-1295.
17. Malhotra A, Orr JE, Owens RL. On the cutting edge of obstructive sleep apnoea: where next? Lancet Respir Med. 2015;3(5):397-403.
18. Mysliwiec V, Capaldi VF, 2nd, Gill J, et al. Adherence to positive airway pressure therapy in U.S. military personnel with sleep apnea improves sleepiness, sleep quality, and depressive symptoms. Mil Med. 2015;180(4):475-482.
19. Salepci B, Caglayan B, Kiral N, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58(9):1467-1473.
20. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178.
21. Pietzsch JB, Liu S, Garner AM, Kezirian EJ, Strollo PJ. Long-term cost-effectiveness of upper airway stimulation for the treatment of obstructive sleep apnea: a model-based projection based on the STAR trial. Sleep. 2015;38(5):735-744.
Sleep-disordered breathing (SDB) is a continuum of symptoms that range from primary snoring with upper airway resistance to frank obstruction seen in obstructive sleep apnea (OSA). This disease spectrum has been reported to affect 10% to 17% of men and 3% to 9% of women in the general population.1 The specific incidence of OSA has been estimated to be about 2% to 4% of the general adult population.2,3 Sleep-disordered breathing often leads to poor sleep quality, which has been associated with many medical comorbidities, including vascular disease, hypertension, major cardiac events, cardiomyopathies, impaired concentration, reduced psychomotor vigilance and cognition, and daytime somnolence.1,2,4-6 Furthermore, there is evidence that the prevalence of SDB continues to grow among the general population.1 However, the prevalence of SDB in various populations (eg, pediatric vs adult, varying body mass index, country of origin) varies widely due to the multifactorial nature of the risk factors and the difficulty in diagnosing SDB.
Some of the more intuitive medical sequelae of SDB are daytime somnolence and subsequent impaired concentration for those with disrupted sleep patterns. Medical literature has paid specific attention to cohorts of personnel who may be at heightened risk from impaired concentration or inability to focus. These populations include but are not limited to sleep-deprived resident physicians, firefighters, truck drivers, and heavy-machine operators.7,8
Military service members represent a distinct cohort that often is relied on to maintain vigilance even in austere environments. Concentration is paramount in order to perform combat operations or tasks that involve operating heavy machinery, such as nuclear submarines, aircraft, or tanks. Given the myriad of unique operational demands on service members, SDB can have detrimental consequences on an individual’s health and his or her military readiness and training. Ultimately, SDB may degrade a unit’s effectiveness and perhaps the country’s military capability.
Active-duty military service members seem to be more susceptible to clinically relevant sleep conditions. In the military, causes of disruptions in normal sleep patterns are multifactorial. Medical literature focuses on circadian disruptions due to shift work and frequent travel, frequent alternating use of caffeine and sedatives, exposure to combat/trauma, and chronic sleep deprivation.9-11 Studies have been published that focus on service members who have returned from combat deployment.10,12,13 However, these studies do not explore the overall burden of disease, and there are no specific data to suggest the prevalence, annual incidence, or associated costs.
To quantify this disease burden in the military, this study focused on the subset of sleep disorders that impact respiration during sleep and determined the prevalence and annual incidence for the entire active-duty population. Additionally, the authors fill a void in the literature by determining the financial burden of SDB on civilian care expenditures.
Methods
This study was a retrospective review of administrative military health care data spanning fiscal years (FYs) 2009 to 2013 (October 1, 2008 to September 30, 2013). The study protocol was approved by the Naval Medical Center Portsmouth Institutional Review Board, and approval was given to waive informed consent. The Health Analysis Department at the Navy and Marine Corps Public Health Center (NMCPHC) obtained and analyzed data from the Military Health System (MHS) Management Analysis and Reporting Tool (M2). The M2 system is an ad hoc query tool used for viewing population, clinical, and financial MHS data, including care received within military treatment facilities (MTFs) and care purchased through TRICARE at civilian facilities. Both inpatient and outpatient health care records were included.
The population included all active-duty service members and guard/reserve members on active duty within all military services, including air force, army, coast guard, and navy branches, between FY 2009 and FY 2013. The authors identified service members with SDB as those with at least 1 ICD-9 diagnosis code related to SDB: obstructive sleep apnea (327.23); sleep-related hypoventilation/hypoxemia (327.26); and other organic sleep disorder (327.80).
Due to the transient nature of the military population, a monthly average over the 5 years of the study determined the overall number of service members eligible for care (1,717,227 service members).
Data Analysis
Prevalence of diagnosed SDB per FY was calculated as the number of service members who received at least 1 SDB diagnostic code between October 1, 2008 and September 30, 2013, over the average total active-duty population. Incidence per year was calculated as the number of new cases per FY, using 2009 as the baseline. Data were stratified by demographic and enrollment information for diagnosed service members and analyzed using SAS 9.4 (Cary, NC) software.
Direct costs associated with SDB treatment fall into 2 categories for service members: (1) care delivered by civilian providers, calculated based on the amount TRICARE paid for the service, using insurance claim data; and (2) care received at MTFs by military providers. Costs for care at MTFs cannot be calculated, as the total cost amount for a single record is not directly attributed to SDB diagnosis.
Results
A total of 197,183 service members were diagnosed with SDB from FY 2009 to FY 2013. Both the annual incidence and prevalence of SDB for the active-duty military population showed upward trends for each of the years evaluated (Figure 1).
Notably, 72% of service members seen for SDB ranged in age from 25 to 44 years (Table).
Discussion
This study shows that the prevalence and incidence of SDB in the active-duty population are less than those reported for the civilian populace as a whole but are still greater than expected for an otherwise healthy and young population. Furthermore, the burden of disease and the cost to diagnose and treat have steadily increased for each of the past 5 fiscal years that were assessed.
The data show an upward trend in the incidence and prevalence of SDB in the military from FY 2009 to FY 2013 for reasons that are not clear but likely with many confounding contributions. As the spectrum of SDB has become better defined and the detrimental sequelae are better understood, it is likely that both service members and health care providers are more aware of the symptoms and more importantly, the potential for interventions that improve quality of life. It is also important to note that the U.S. military is a very transient organization with a nearly constant turnover between new enlistees/officers and those leaving the service or retiring after 20 years of service. Thus, despite an annual incidence of nearly 3% throughout the years evaluated, the annual increase in prevalence is not necessarily commensurate.
The FY 2013 prevalence (4.2%) and civilian care costs ($98,259,519) present traditional indications of the disease burden. Both metrics represent a sizable and increasing disease burden for the military. It is also important to note that these costs reflect only the short-term expenses for initial diagnosis and therapy. These costs in no way reflect the care for the long-term medical sequelae that have been recently linked to uncontrolled SDB/OSA, such as heart and vascular diseases, hypertension, and increased stroke risk. Additional costs will continue to grow.
Perhaps the most validated predictive factor for diagnosis of SDB or OSA is body habitus as measured by body mass index (BMI). In particular, nearly 60% to 90% of patients with OSA are obese.2 Weight gain seems to increase the OSA severity, whereas losing weight decreases it.14-16 Although the U.S. military employs height and weight standards that preclude those with persistently overweight or obese BMIs from continued service, these standards often are not rigid, and there are overweight or even obese active-duty members. Interestingly, despite a population that essentially controls for the most predictive risk factor, the prevalence of SDB is still approximately 1 in 20 (4.9%) in FY 2013.
Given the significant burden of disease represented by the incidence, prevalence, and cost data determined in this study and the growing recognition of long-term complications from poorly controlled SDB, it has become evident that more efficacious interventions are needed. Modern treatments for SDB can be classified as surgical or nonsurgical but with no single modality fitting the need for all patients secondary to poor adherence and/or limited efficacy.17-20 However, to mitigate the impact on military readiness and taxpayer-funded health care costs, it may be appropriate to begin exploring therapeutic options beyond the current standard of care. For example, an invasive and costly onetime surgical intervention using an implantable device to stimulate the hypoglossal nerve to open a person’s airway during inspiration is being investigated in a younger, nonobese cohort of patients.21 Further research is warranted into this specific model of therapeutic intervention and others for service members.
Limitations
Limitations in this study include possible reporting errors due to improper or insufficient medical coding as well as data entry errors at the clinic that may exist within medical billing databases. Therefore, the results of this analysis may be over- or underrepresented. The increase in incidence and prevalence may not necessarily reflect an increasing number of people who have the disease. The increase could be a result of better SDB detection practices or incentives to be diagnosed with SDB (VA disability claims upon retirement). The assumption is made that procedures corresponding with SDB diagnoses are directly related to SDB, and any costs incurred from those procedures are due to SDB.
It is important to note variability between services and institutions within the DoD in the diagnosis and treatment of SDB. Specifically, some institutions use ambulatory polysomnograms, or studies done at home, and autotitration of continuous positive airway pressure, whereas others require more costly hospital-based studies and laboratory titration. Another confounder in the cost data is the number of diagnoses and treatment deferred to the network as a result of the relatively small number of sleep-trained physicians within the military.
Conclusion
As the field of sleep medicine continues to develop its literature, it is becoming clearer that the detrimental sequelae of SDB are varied and pose significant short- and long-term risks. Active-duty service members represent a subset of the population with consequences that are potentially graver than those of civilians, especially when they are expected to operate complicated machinery or to make rapid and critical decisions in battle.
The prevalence and incidence of SDB increased each year during a 5-year review and currently affects 1 in 20 service members. Furthermore, the cost of civilian care for this disease process was nearly $100 million in FY 2012 to FY 2013, suggesting a growing financial burden for taxpayers. Further research is warranted to fully appreciate the impact of SDB on both service members and the U.S. military.
Acknowledgments
The authors thank the U.S. Navy and specifically the support within the Department of Otolaryngology at the Naval Medical Center Portsmouth for the time and effort allotted for completion of this study. This research was supported in part by an appointment to the Postgraduate Research Participation Program at the Navy and Marine Corps Public Health Center (NMCPHC) administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and NMCPHC.
Sleep-disordered breathing (SDB) is a continuum of symptoms that range from primary snoring with upper airway resistance to frank obstruction seen in obstructive sleep apnea (OSA). This disease spectrum has been reported to affect 10% to 17% of men and 3% to 9% of women in the general population.1 The specific incidence of OSA has been estimated to be about 2% to 4% of the general adult population.2,3 Sleep-disordered breathing often leads to poor sleep quality, which has been associated with many medical comorbidities, including vascular disease, hypertension, major cardiac events, cardiomyopathies, impaired concentration, reduced psychomotor vigilance and cognition, and daytime somnolence.1,2,4-6 Furthermore, there is evidence that the prevalence of SDB continues to grow among the general population.1 However, the prevalence of SDB in various populations (eg, pediatric vs adult, varying body mass index, country of origin) varies widely due to the multifactorial nature of the risk factors and the difficulty in diagnosing SDB.
Some of the more intuitive medical sequelae of SDB are daytime somnolence and subsequent impaired concentration for those with disrupted sleep patterns. Medical literature has paid specific attention to cohorts of personnel who may be at heightened risk from impaired concentration or inability to focus. These populations include but are not limited to sleep-deprived resident physicians, firefighters, truck drivers, and heavy-machine operators.7,8
Military service members represent a distinct cohort that often is relied on to maintain vigilance even in austere environments. Concentration is paramount in order to perform combat operations or tasks that involve operating heavy machinery, such as nuclear submarines, aircraft, or tanks. Given the myriad of unique operational demands on service members, SDB can have detrimental consequences on an individual’s health and his or her military readiness and training. Ultimately, SDB may degrade a unit’s effectiveness and perhaps the country’s military capability.
Active-duty military service members seem to be more susceptible to clinically relevant sleep conditions. In the military, causes of disruptions in normal sleep patterns are multifactorial. Medical literature focuses on circadian disruptions due to shift work and frequent travel, frequent alternating use of caffeine and sedatives, exposure to combat/trauma, and chronic sleep deprivation.9-11 Studies have been published that focus on service members who have returned from combat deployment.10,12,13 However, these studies do not explore the overall burden of disease, and there are no specific data to suggest the prevalence, annual incidence, or associated costs.
To quantify this disease burden in the military, this study focused on the subset of sleep disorders that impact respiration during sleep and determined the prevalence and annual incidence for the entire active-duty population. Additionally, the authors fill a void in the literature by determining the financial burden of SDB on civilian care expenditures.
Methods
This study was a retrospective review of administrative military health care data spanning fiscal years (FYs) 2009 to 2013 (October 1, 2008 to September 30, 2013). The study protocol was approved by the Naval Medical Center Portsmouth Institutional Review Board, and approval was given to waive informed consent. The Health Analysis Department at the Navy and Marine Corps Public Health Center (NMCPHC) obtained and analyzed data from the Military Health System (MHS) Management Analysis and Reporting Tool (M2). The M2 system is an ad hoc query tool used for viewing population, clinical, and financial MHS data, including care received within military treatment facilities (MTFs) and care purchased through TRICARE at civilian facilities. Both inpatient and outpatient health care records were included.
The population included all active-duty service members and guard/reserve members on active duty within all military services, including air force, army, coast guard, and navy branches, between FY 2009 and FY 2013. The authors identified service members with SDB as those with at least 1 ICD-9 diagnosis code related to SDB: obstructive sleep apnea (327.23); sleep-related hypoventilation/hypoxemia (327.26); and other organic sleep disorder (327.80).
Due to the transient nature of the military population, a monthly average over the 5 years of the study determined the overall number of service members eligible for care (1,717,227 service members).
Data Analysis
Prevalence of diagnosed SDB per FY was calculated as the number of service members who received at least 1 SDB diagnostic code between October 1, 2008 and September 30, 2013, over the average total active-duty population. Incidence per year was calculated as the number of new cases per FY, using 2009 as the baseline. Data were stratified by demographic and enrollment information for diagnosed service members and analyzed using SAS 9.4 (Cary, NC) software.
Direct costs associated with SDB treatment fall into 2 categories for service members: (1) care delivered by civilian providers, calculated based on the amount TRICARE paid for the service, using insurance claim data; and (2) care received at MTFs by military providers. Costs for care at MTFs cannot be calculated, as the total cost amount for a single record is not directly attributed to SDB diagnosis.
Results
A total of 197,183 service members were diagnosed with SDB from FY 2009 to FY 2013. Both the annual incidence and prevalence of SDB for the active-duty military population showed upward trends for each of the years evaluated (Figure 1).
Notably, 72% of service members seen for SDB ranged in age from 25 to 44 years (Table).
Discussion
This study shows that the prevalence and incidence of SDB in the active-duty population are less than those reported for the civilian populace as a whole but are still greater than expected for an otherwise healthy and young population. Furthermore, the burden of disease and the cost to diagnose and treat have steadily increased for each of the past 5 fiscal years that were assessed.
The data show an upward trend in the incidence and prevalence of SDB in the military from FY 2009 to FY 2013 for reasons that are not clear but likely with many confounding contributions. As the spectrum of SDB has become better defined and the detrimental sequelae are better understood, it is likely that both service members and health care providers are more aware of the symptoms and more importantly, the potential for interventions that improve quality of life. It is also important to note that the U.S. military is a very transient organization with a nearly constant turnover between new enlistees/officers and those leaving the service or retiring after 20 years of service. Thus, despite an annual incidence of nearly 3% throughout the years evaluated, the annual increase in prevalence is not necessarily commensurate.
The FY 2013 prevalence (4.2%) and civilian care costs ($98,259,519) present traditional indications of the disease burden. Both metrics represent a sizable and increasing disease burden for the military. It is also important to note that these costs reflect only the short-term expenses for initial diagnosis and therapy. These costs in no way reflect the care for the long-term medical sequelae that have been recently linked to uncontrolled SDB/OSA, such as heart and vascular diseases, hypertension, and increased stroke risk. Additional costs will continue to grow.
Perhaps the most validated predictive factor for diagnosis of SDB or OSA is body habitus as measured by body mass index (BMI). In particular, nearly 60% to 90% of patients with OSA are obese.2 Weight gain seems to increase the OSA severity, whereas losing weight decreases it.14-16 Although the U.S. military employs height and weight standards that preclude those with persistently overweight or obese BMIs from continued service, these standards often are not rigid, and there are overweight or even obese active-duty members. Interestingly, despite a population that essentially controls for the most predictive risk factor, the prevalence of SDB is still approximately 1 in 20 (4.9%) in FY 2013.
Given the significant burden of disease represented by the incidence, prevalence, and cost data determined in this study and the growing recognition of long-term complications from poorly controlled SDB, it has become evident that more efficacious interventions are needed. Modern treatments for SDB can be classified as surgical or nonsurgical but with no single modality fitting the need for all patients secondary to poor adherence and/or limited efficacy.17-20 However, to mitigate the impact on military readiness and taxpayer-funded health care costs, it may be appropriate to begin exploring therapeutic options beyond the current standard of care. For example, an invasive and costly onetime surgical intervention using an implantable device to stimulate the hypoglossal nerve to open a person’s airway during inspiration is being investigated in a younger, nonobese cohort of patients.21 Further research is warranted into this specific model of therapeutic intervention and others for service members.
Limitations
Limitations in this study include possible reporting errors due to improper or insufficient medical coding as well as data entry errors at the clinic that may exist within medical billing databases. Therefore, the results of this analysis may be over- or underrepresented. The increase in incidence and prevalence may not necessarily reflect an increasing number of people who have the disease. The increase could be a result of better SDB detection practices or incentives to be diagnosed with SDB (VA disability claims upon retirement). The assumption is made that procedures corresponding with SDB diagnoses are directly related to SDB, and any costs incurred from those procedures are due to SDB.
It is important to note variability between services and institutions within the DoD in the diagnosis and treatment of SDB. Specifically, some institutions use ambulatory polysomnograms, or studies done at home, and autotitration of continuous positive airway pressure, whereas others require more costly hospital-based studies and laboratory titration. Another confounder in the cost data is the number of diagnoses and treatment deferred to the network as a result of the relatively small number of sleep-trained physicians within the military.
Conclusion
As the field of sleep medicine continues to develop its literature, it is becoming clearer that the detrimental sequelae of SDB are varied and pose significant short- and long-term risks. Active-duty service members represent a subset of the population with consequences that are potentially graver than those of civilians, especially when they are expected to operate complicated machinery or to make rapid and critical decisions in battle.
The prevalence and incidence of SDB increased each year during a 5-year review and currently affects 1 in 20 service members. Furthermore, the cost of civilian care for this disease process was nearly $100 million in FY 2012 to FY 2013, suggesting a growing financial burden for taxpayers. Further research is warranted to fully appreciate the impact of SDB on both service members and the U.S. military.
Acknowledgments
The authors thank the U.S. Navy and specifically the support within the Department of Otolaryngology at the Naval Medical Center Portsmouth for the time and effort allotted for completion of this study. This research was supported in part by an appointment to the Postgraduate Research Participation Program at the Navy and Marine Corps Public Health Center (NMCPHC) administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and NMCPHC.
1. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014.
2. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-1239.
3. Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14(1):63-70.
4. Kim H, Dinges DF, Young T. Sleep-disordered breathing and psychomotor vigilance in a community-based sample. Sleep. 2007;30(10):1309-1316.
5. Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017-1028.
6. Gilat H, Vinker S, Buda I, Soudry E, Shani M, Bachar G. Obstructive sleep apnea and cardiovascular comorbidities: a large epidemiologic study. Medicine (Baltimore). 2014;93(9):e45.
7. Li X, Sundquist K, Sundquist J. Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med. 2008;9(2):129-136.
8. Barger LK, Rajaratnam SM, Wang W, et al. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J Clin Sleep Med. 2015;11(3):233-240.
9. Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549-557.
10. Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167-174.
11. Capaldi VF 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med. 2011;176(8):879-888.
12. Collen J, Orr N, Lettieri CJ, Carter K, Holley AB. Sleep disturbances among soldiers with combat-related traumatic brain injury. Chest. 2012;142(3):622-630.
13. Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173(3):230-235.
14. Dixon JB, Schachter LM, O’Brien PE. Polysomnography before and after weight loss in obese patients with severe sleep apnea. Int J Obes (Lond). 2005;29(9):1048-1054.
15. Loube DI, Loube AA, Erman MK. Continuous positive airway pressure treatment results in weight less in obese and overweight patients with obstructive sleep apnea. J Am Diet Assoc. 1997;97(8):896-897.
16. Loube DI, Loube AA, Mitler MM. Weight loss for obstructive sleep apnea: the optimal therapy for obese patients. J Am Diet Assoc. 1994;94(11):1291-1295.
17. Malhotra A, Orr JE, Owens RL. On the cutting edge of obstructive sleep apnoea: where next? Lancet Respir Med. 2015;3(5):397-403.
18. Mysliwiec V, Capaldi VF, 2nd, Gill J, et al. Adherence to positive airway pressure therapy in U.S. military personnel with sleep apnea improves sleepiness, sleep quality, and depressive symptoms. Mil Med. 2015;180(4):475-482.
19. Salepci B, Caglayan B, Kiral N, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58(9):1467-1473.
20. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178.
21. Pietzsch JB, Liu S, Garner AM, Kezirian EJ, Strollo PJ. Long-term cost-effectiveness of upper airway stimulation for the treatment of obstructive sleep apnea: a model-based projection based on the STAR trial. Sleep. 2015;38(5):735-744.
1. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014.
2. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-1239.
3. Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14(1):63-70.
4. Kim H, Dinges DF, Young T. Sleep-disordered breathing and psychomotor vigilance in a community-based sample. Sleep. 2007;30(10):1309-1316.
5. Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017-1028.
6. Gilat H, Vinker S, Buda I, Soudry E, Shani M, Bachar G. Obstructive sleep apnea and cardiovascular comorbidities: a large epidemiologic study. Medicine (Baltimore). 2014;93(9):e45.
7. Li X, Sundquist K, Sundquist J. Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med. 2008;9(2):129-136.
8. Barger LK, Rajaratnam SM, Wang W, et al. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J Clin Sleep Med. 2015;11(3):233-240.
9. Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549-557.
10. Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167-174.
11. Capaldi VF 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med. 2011;176(8):879-888.
12. Collen J, Orr N, Lettieri CJ, Carter K, Holley AB. Sleep disturbances among soldiers with combat-related traumatic brain injury. Chest. 2012;142(3):622-630.
13. Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173(3):230-235.
14. Dixon JB, Schachter LM, O’Brien PE. Polysomnography before and after weight loss in obese patients with severe sleep apnea. Int J Obes (Lond). 2005;29(9):1048-1054.
15. Loube DI, Loube AA, Erman MK. Continuous positive airway pressure treatment results in weight less in obese and overweight patients with obstructive sleep apnea. J Am Diet Assoc. 1997;97(8):896-897.
16. Loube DI, Loube AA, Mitler MM. Weight loss for obstructive sleep apnea: the optimal therapy for obese patients. J Am Diet Assoc. 1994;94(11):1291-1295.
17. Malhotra A, Orr JE, Owens RL. On the cutting edge of obstructive sleep apnoea: where next? Lancet Respir Med. 2015;3(5):397-403.
18. Mysliwiec V, Capaldi VF, 2nd, Gill J, et al. Adherence to positive airway pressure therapy in U.S. military personnel with sleep apnea improves sleepiness, sleep quality, and depressive symptoms. Mil Med. 2015;180(4):475-482.
19. Salepci B, Caglayan B, Kiral N, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58(9):1467-1473.
20. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178.
21. Pietzsch JB, Liu S, Garner AM, Kezirian EJ, Strollo PJ. Long-term cost-effectiveness of upper airway stimulation for the treatment of obstructive sleep apnea: a model-based projection based on the STAR trial. Sleep. 2015;38(5):735-744.