User login
Percutaneous coronary intervention (PCI) using coronary artery stent implantation is commonly used to treat symptomatic high-risk and unstable coronary artery disease (CAD). The use of stents has improved the safety and efficacy of PCI by reducing the need for repeat revascularization, reducing acute vessel closure requiring emergent coronary artery bypass graft surgery, and expanding the use of PCI to more complex diseases. Nevertheless, stents carry the risk of sudden thrombotic occlusion or stent thrombosis, particularly during the first several days or weeks after implantation. In turn, stent thrombosis can lead to acute myocardial infarction (MI) and a mortality rate > 25%.1,2
This article highlights 2 cases of patients with stent thrombosis and discusses its pathophysiology, clinical features, and risk-avoidance strategies. Given the high prevalence of CAD and ubiquitous PCI procedures in the U.S. health care system, it is essential that not only cardiologists, but all clinicians and health care providers who care for patients with coronary stents understand how to help prevent and manage this life-threatening clinical entity.1
Case 1
A 56-year-old man presented to his primary care physician with exertion-related angina. The patient had a history of type 2 diabetes mellitus, dyslipidemia, systemic hypertension, obesity, and CAD status post MI in 2002 treated with a bare metal stent (BMS) to the left circumflex coronary artery (LCx). A stress myocardial perfusion imaging with 99mTc-sestamibi revealed moderate reversible exercise-induced myocardial ischemia involving the inferior and inferoapical wall segments of the left ventricle with associated hypokinesia.
Coronary angiography revealed nonsignificant disease of the left anterior descending artery (LAD) and LCx, a patent LCx stent, and a 95% mid-right coronary artery (RCA) obstruction with delayed (TIMI grade 2) antegrade flow. The distal right posterior descending artery filled via left to right collaterals from the LAD.
Percutaneous coronary intervention was performed on the RCA lesion 8 days after the patient was started on dual antiplatelet therapy (DAPT) with aspirin 81 mg and clopidogrel 75 mg (including 300 mg loading dose on the day of the diagnostic angiogram). The mid RCA was treated with a drug-eluting stent (DES) and a BMS in a nonoverlapping fashion with an excellent angiographic result. The patient was instructed to continue DAPT with aspirin 325 mg daily and clopidogrel 75 mg daily for 12 months.
Three days post PCI, the patient arrived at the emergency department with angina of 1-hour duration associated with shortness of breath and diaphoresis. He reported strict adherence to DAPT.
Initial vital signs were normal. The electrocardiogram (ECG) showed ST segment elevation (1-2 mm) on leads III, aVF, and V5 to V6, suggestive of an acute inferolateral injury pattern for which emergent coronary angiography was performed. Angiography showed a 100% proximal RCA occlusion at the proximal edge of the most proximal stent with absence of any antegrade flow beyond the occlusion (TIMI grade 0 flow). This finding was diagnostic of definite angiographic subacute stent thrombosis. The patient underwent successful aspiration thrombectomy, balloon angioplasty, and restoration of normal TIMI grade 3 flow with a door-to-balloon time of 86 minutes.
Because stent thrombosis is relatively unexpected after an excellent angiographic result and DAPT adherence, the possibility of clopidogrel resistance was considered as a major contributor for the thrombotic event. Platelet aggregation tests showed adequate prolongation of collagen/epinephrine (COL-EPI) > 300 seconds (normal: 81-153 seconds), but inadequate prolongation of collagen/adenosindiphosphate (COL-ADP) of 109 seconds (normal: 53-105 seconds) while on clopidogrel. Therefore, the patient was switched to prasugrel.
The patient was discharged home after 5 days of observation at the cardiac care unit without any post-MI complications. During a follow-up appointment 1 month after discharge, he was clinically stable and free of cardiovascular symptoms. Workup performed for acquired or inherited thrombophilia was negative. He continued taking DAPT (daily aspirin 325 mg orally and prasugrel 10 mg orally) for 12 months. After completing 12 months of DAPT, he was maintained on aspirin 81 mg daily. At 24 months’ follow-up, he remained free of recurrent angina with no further cardiovascular events.
Case 2
An 84-year-old man with a medical history of dyslipidemia, paroxysmal atrial fibrillation, previous stroke, and peptic ulcer disease was brought to the emergency department following an episode of near syncope in the early morning hours. The patient revealed that he had experienced neck pain since midnight. The 12-lead ECG showed normal sinus rhythm with 2 mm ST segment elevation in leads II, III, aVF, V5-V6, and ST segment depression in V2, and Q waves in inferior leads. A right-sided ECG showed ST segment elevation in V4, suggestive of right ventricle infarction.
The patient remained hypotensive (83/49 mm Hg) despite isotonic fluid administration (about 1.5-2.0 liters of 0.9 normal saline at 999 mL/h). A dopamine drip for persistent hypotension was started, and he was taken emergently to the catheterization laboratory for primary PCI. Coronary angiography showed no significant left CAD and a 100% mid-RCA occlusion with faint left-to-right collaterals. After aspiration thrombectomy, bare metal RCA stenting was performed. Transient no-reflow was treated with intracoronary nicardipine and nitroglycerin. The patient continued to be in shock, and an intra-aortic balloon pump was inserted and 1:1 counterpulsation was initiated.
Following admission to the coronary care unit, the patient’s mean arterial pressure improved. Inotropes were weaned off 2 days after PCI, and the intra-aortic balloon pump was removed. During his stay, the post-MI course was uneventful except for an episode of asymptomatic paroxysmal atrial flutter and nonspecific back dermatitis attributed to a prolonged recumbent position.
The patient was transferred to the internal medicine ward for medical therapy optimization and the initiation of low-intensity cardiac rehabilitation. After 2 days on the ward, discharge planning was initiated. However, he developed an episode of atrial fibrillation with fast ventricular response. Metoprolol 5 mg IV bolus was given, and the ventricular rate was controlled. At that point, the dose of long-acting beta-blocker (metoprolol succinate) was optimized, he was started on full-dose anticoagulation (warfarin), and clopidogrel was discontinued. Two days later, the patient reported back pruritus, and an erythematous raised rash on his back spreading to the torso was noticed. An aspirin allergy was suspected as the trigger for the rash, thus aspirin was also discontinued.
Three days later, the patient developed recurrent neck pain (angina) with radiation to his shoulders and left arm. The ECG revealed re-elevation of the ST segment (inferior, posterior, and lateral leads). He received reloading of clopidogrel 600 mg and aspirin 325 mg. Also, an eptifibatide IV bolus followed by an infusion was given for immediate antiplatelet action. He was transferred for emergent coronary angiography with suspected subacute stent thrombosis.
Upon arrival to the catheterization lab, the patient was awake and alert but in mild respiratory distress. Intravenous dopamine was started due to hypotension (systolic blood pressure was about 85 mm Hg). Limited RCA angiography showed a large clot burden with a partially thrombosed stent and TIMI grade 3 flow. After intracoronary eptifibatide and nicardipine were given, successful aspiration thrombectomy was performed twice with partial removal of thrombus. In-stent high-pressure balloon angioplasty was performed and optimal stenting was confirmed by intravascular ultrasound (IVUS) criteria. However, a residual layered thrombus along the distal stent edge was noticed. The patient tolerated the procedure without complications.
Dual antiplatelet therapy with aspirin and clopidogrel for 12 months was recommended. The eptifibatide infusion was continued for 48 hours. The jaw pain, shortness of breath, and ECG changes disappeared, but the patient remained on vasopressors for the following 7 days.
Around 1 week after the stent thrombosis event, the patient was found pulseless. Advanced cardiopulmonary resuscitation was started. ST segment elevation in lead II was noted on the cardiac monitor. There was no return of spontaneous circulation after 20 minutes, and the patient was pronounced dead. The autopsy revealed a patent RCA stent without evidence of occlusion, a large transmural inferior MI, left ventricular rupture, and hemopericardium.
Discussion
Stent thrombosis is an uncommon complication after coronary stent implantation. Based on the Academic Research Consortium criteria, definite stent thrombosis is defined as a clinical event with symptoms suggestive of an acute coronary syndrome (ACS) with angiography or pathology that confirms the presence of stent thrombosis.2 Probable stent thrombosis is defined as an unexplained death within 30 days or MI involving the territory of the target vessel without angiographic confirmation of stent thrombosis.2 Finally, possible stent thrombosis is any unexplained death after 30 days.2
Based on timing, stent thrombosis is divided by acute (< 24 hours post stent implantation), subacute (24 hours to 30 days post stent implantation), late (> 30 days post stent implantation), and very late (> 12 months post stent implantation).3 However, most cases (up to 60%) occur within the first 30 days after placement, irrespective of stent type.4
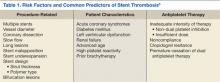
The incidence of subacute stent thrombosis is reported to approach 1% during the first 30 days postprocedure but may be as high as 5% or 10% depending on associated clinical and angiographic variables (Table 1).5 The strongest clinical predictors of stent thrombosis are premature cessation of antiplatelet therapy, renal insufficiency, diabetes mellitus, and ACS.2,6 Lesion and procedural characteristics associated with increased risk of stent thrombosis include bifurcation lesions, longer stent length, multiple implanted stents, stent underexpansion, and/or stent malapposition.6-9 Stent type (drug or non–drug-eluting) has no impact on the risk of stent thrombosis during the first 30 days postprocedure.10,11
The clinical events related to late stent thrombosis, although rare, carry a mortality rate of up to 45%.12 The specific risk factors for late and very late stent thrombosis are less well defined but relate to delayed neointimal coverage, ongoing vessel inflammation, and the development of neoatherosclerosis within stents.13,14
Rationale for the Use of Dual Antiplatelet Regimen
Stent thrombosis is a platelet-mediated process related to a heightened state of systemic and intracoronary thrombogenicity and inflammation.15 Stent under-expansion enhances abnormal shear stress, which explains as many as 80% of these events.13,15,16 Stent thrombosis also has been frequently related to inadequate neointimal coverage.14 Angioscopic studies, especially with DES, suggest that stent endothelialization is delayed or incomplete, observing a correlation between the areas of uncovered stent surface and thrombosis.14,17
In the early days of coronary stenting, during the 1990s, the risk of acute and subacute stent thrombosis approached 20%.18,19 Initial attempts to reduce the risk included combining aspirin and warfarin, but at the expense of a marked increase in bleeding complications and prolonged hospital stays.20,21 In 1995, it became clear through the pivotal observations of Colombo and colleagues that incomplete expansion of the stent (documented by IVUS) was a major contributor to the risk of stent thrombosis.16 By using noncompliant balloons at high pressure (14-20 atmospheres) for stent postdilatation combined with DAPT (aspirin and ticlopidine), the high rates of early stent thrombosis were markedly reduced to the current level of 1% to 2%.16
Colombo and colleagues’ observations were prospectively evaluated in the Stent Anticoagulation Regimen Study (STARS) trial.22 Patients who underwent successful stenting were randomized to aspirin alone, aspirin and warfarin, or aspirin and ticlopidine. The STARS trial showed convincingly that the combination of aspirin and ticlopidine was superior to the other 2 regimens, reducing the stent thrombosis rate to only 0.5% (compared with 2.7% for aspirin and warfarin, and 3.6% for aspirin alone).22 Afterward, DAPT became the standard of care following coronary stenting.23
Although ticlopidine was the first widely used thienopyridine for the prevention of stent thrombosis, hematologic adverse events (AEs) (eg, neutropenia, thrombotic thrombocytopenia purpura) limited its use.24 Consequently, ticlopidine was replaced with clopidogrel, which seemed to offer similar efficacy but significantly fewer AEs.25
The current American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines for the prevention of ST after coronary stent implantation state that after PCI:
- Aspirin use should be continued indefinitely.
- The duration of adenosine diphosphate antagonists depends on the stent type (BMS or DES) and the indication for implantation (ACS or non-ACS).
a. Patients receiving a stent (BMS or DES) for ACS therapy should be given 1 of the following for at least 12 months:
i. Clopidogrel 75 mg daily
ii. Prasugrel 10 mg daily
iii. Ticagrelor 90 mg twice daily
b. In patients receiving DES for a non-ACS indication, clopidogrel should be given for at least 12 months if the patient is not at high risk for bleeding.
c. In patients receiving BMS for a non-ACS indication, clopidogrel should be given for a minimum of 1 month and ideally up to 12 months.23
Clopidogrel Hyporesponse
As shown in case 1, stent thrombosis may still occur in a patient on DAPT because of individual variability in platelet response to clopidogrel.5 Clopidogrel hyporesponse, also known as clopidogrel resistance, has been recognized as clinically significant because of its prevalence and association with poor outcomes.5 Its prevalence may range between 4% and 30%, although the definitions of clopidogrel hyporesponse varied between studies.26
Clopidogrel hyporesponse is defined as an inadequate inhibition of platelet function measured by nonspecific ex-vivo laboratory methods.27,28 The relationship between clopidogrel resistance (nonresponders), stent thrombosis, and ischemic events has been clearly established.5,29
Given the devastating consequences of stent thrombosis, efforts were directed to identify those patients at highest risk. One such effort has been focused on the measurement of platelet function, allowing for the identification of patients who do not respond adequately to antiplatelet therapy.15,28,30,31 However, the treatment of high-residual platelet reactivity as confirmed by laboratory assessment has not shown to clinically correlate with any benefit in the prevention of ST.6,15,29-31 Therefore, the current ACC/AHA/SCAI PCI guidelines do not recommend the routine clinical use of platelet function testing to screen patients treated with clopidogrel who are undergoing PCI.23
Clopidogrel is a prodrug, metabolized to its active form via the cytochrome P450 enzyme system before it can inhibit platelet function.32 Accordingly, certain genetic variation in enzyme activity, or polymorphisms, would be expected to influence its clinical effectiveness.33,34 The most common of these polymorphisms, CYP2C19*2, has been associated (in vitro) with reduced concentrations of active clopidogrel metabolites and with diminished platelet inhibition.35,36 As a result, the FDA has added a safety alert to the prescribing information for clopidogrel concerning how genetic differences in the metabolism of this agent can affect its effectiveness, ways to test for these genetic differences, and advice concerning alternative dosing strategies or use of other medications in poor metabolizers of clopidogrel.37 Although the routine clinical use of genetic testing to screen patients treated with clopidogrel who are undergoing PCI is not recommended, it may be considered in patients undergoing elective high-risk PCI procedures (eg, unprotected left main, last patent coronary artery, or bifurcating left main).23
The newer inhibitors of ADP-induced platelet activation, prasugrel and ticagrelor, are not prodrugs, and thus, their action is not affected by this genetic variability. Accordingly, these drugs have shown a more consistent, stronger, and faster inhibition of platelet aggregation compared with clopidogrel.36-39 In the pivotal trials (TRITON-TIMI 38 and PLATO), these agents have also been shown to be more effective in reducing the incidence of stent thrombosis.36,37,40,41 Therefore, in cases where clopidogrel resistance/hyporesponse is suspected in the setting of DAPT, such as stent thrombosis, guidelines recommend the use of 1 of these agents.23
Premature Discontinuation of Antiplatelet Therapy
As illustrated in case 2, premature discontinuation of antiplatelet therapy may be fatal, as it is associated with a marked increase in the risk of stent thrombosis. Indeed, premature discontinuation of DAPT is the leading independent predictor for stent thrombosis.12,42,43 Premature discontinuation of DAPT is defined when one or both agents (aspirin, ADP-antagonists) are suspended within 30 days of BMS placement or within 1 year of DES placement. In the case of DES, the first 6 months after implantation seem to be most critical. In a large observational study of patients treated with DES, stent thrombosis occurred in 29% of those patients in whom antiplatelet therapy was prematurely discontinued.12
In order to minimize the risk of premature DAPT discontinuation, one should address its causes. There are patient- and physician-related factors that may influence an early discontinuation of aspirin, thienopyridine, or both agents. Patient-related factors were identified in the PREMIER registry, including older age, not having completed high school, not being married, and/or not seeking health care because of costs.42 Another important but often overlooked factor that has an impact on adherence with prolonged DAPT post-DES implantation is nuisance or superficial bleeding.44 Physician-related factors include not providing discharge instructions for medication use and ill-advised instructions given by health care providers to discontinue therapy before procedures with a low risk of bleeding (eg, dental cleaning, cataract surgery, colonoscopy, skin biopsy).42
In addition, the perioperative management of DAPT during the first several weeks after coronary stenting has been shown to critically influence outcomes. In a study by Sharma and colleagues, fatal cases of stent thrombosis occurred after the discontinuation of antiplatelet therapy for noncardiac surgery among patients with BMS implantation within the past 90 days.43
In selected cases when a noncardiac procedure cannot be delayed for 1 year, recognizing the impact of the specific timing for the discontinuation of the antiplatelet regimen is essential. Kaluza and colleagues reported on 40 patients treated with BMS who underwent noncardiac surgery within 6 weeks of the stent implantation.45 Seven patients had an MI, of which 6 were fatal. Stent thrombosis was presumed to be the cause of all MIs. In 5 of 7 cases, ticlopidine was withheld before surgery.45
All clinicians should be aware of the following recommendations to avoid catastrophic cardiovascular complications related to premature discontinuation of DAPT during the perioperative setting:
- Elective procedures should be deferred until patients have completed an appropriate course of thienopyridine therapy (12 months after DES and a minimum of 4 weeks for BMS implantation).
- For those patients treated with DES who are to undergo a nonelective procedure that mandates discontinuation of thienopyridine therapy, the possibility of procedure postponement for completion of DAPT for at least 6 months should be judiciously deliberated. If the procedure cannot be postponed, aspirin should be continued if at all possible and the thienopyridine restarted as soon as possible after the procedure.42,46,47
Conclusion
Stent thrombosis is a rare but devastating complication of coronary stent implantation. Although it can occur at any time after stent placement, the majority of events occur within the first month. The use of optimal stenting techniques and adherence to DAPT are required to minimize the risk of stent thrombosis. Several clinical and procedural predictors have been related to an increased risk of stent thrombosis. The premature cessation of DAPT is the most important risk factor for stent thrombosis.
All physicians should ensure patients are properly and thoroughly educated about the reasons they are prescribed DAPT and the significant risks associated with prematurely discontinuing such therapy. All clinicians, especially noncardiologists, should realize the importance of close communication with a cardiologist or interventional cardiologist in situations when premature discontinuation is being considered for a specific reason.
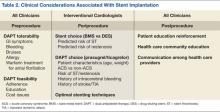
Table 2 summarizes a framework of the most relevant factors that should be taken into account before, during, and after stent implantation, both by interventional cardiologists, as well as by all clinicians involved in the care of the patient. Given current procedural volumes (> 1 million PCI procedures are performed in the U.S. annually) and because the risk of stent thrombosis is both time and treatment dependent, it is of paramount importance that, not only cardiologists, but all physicians know the impact of stent thrombosis in their patients and how to avoid situations that may increase its risk.1 Team-approach decisions about antiplatelet therapy after stent placement, especially within the first 12 months, and a patient-centered mind-set are indispensable to optimize patient outcomes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Ryan J, Cohen DJ. Are drug-eluting stents cost-effective? It depends on whom you ask. Circulation. 2006;114(16):1736-1744.
2. Cutlip DE, Windecker S, Mehran R, et al; Academic Research Consortium. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation. 2007;115(17):2344-2351.
3. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK; Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494-502.
4. Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: Meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012;5(3):357-364.
5. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, et al. Variability in individual responsiveness to clopidogrel: Clinical implications, management, and future perspectives. J Am Coll Cardiol. 2007;49(14):1505-1516.
6. Moussa I, Di Mario C, Reimers B, Akiyama T, Tobis J, Colombo A. Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: Frequency, predictors and clinical outcome. J Am Coll Cardiol. 1997;29(1):6-12.
7. Fujii K, Carlier SG, Mintz GS, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: An intravascular ultrasound study. J Am Coll Cardiol. 2005;45(7):995-998.
8. Uren NG, Schwarzacher SP, Metz JA, et al; POST Registry Investigators. Predictors and outcomes of stent thrombosis: An intravascular ultrasound registry. Eur Heart J. 2002;23(2):124-132.
9. Cook S, Wenaweser P, Togni M, et al. Intravascular ultrasound in very late DES-stent thrombosis (abstr). J Am Coll Cardiol. 2006;47(suppl B):9B.
10. Moreno R, Fernández C, Hernández R, et al. Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies. J Am Coll Cardiol. 2005;45(6):954-959.
11. Ellis SG, Colombo A, Grube E, et al. Incidence, timing, and correlates of stent thrombosis with the polymeric paclitaxel drug-eluting stent: A TAXUS II, IV, V, and VI meta-analysis of 3,445 patients followed for up to 3 years. J Am Coll Cardiol. 2007;49(10):1043-1051.
12. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126-2130.
13. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: A pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001;103(15):1967-1971.
14. Kotani J, Awata M, Nanto S, et al. Incomplete neointimal coverage of sirolimus-eluting stents: Angioscopic findings. J Am Coll Cardiol. 2006;47(10):2108–2111.
15. Cheneau E, Leborgne L, Mintz GS, et al. Predictors of subacute stent thrombosis: Results of a systematic intravascular ultrasound study. Circulation. 2003;108(1):43-47.
16. Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation achieved with intravascular ultrasound guidance. Circulation. 1995;91(6):1676-1688.
17. Oyabu J, Ueda Y, Ogasawara N, Okada K, Hirayama A, Kodama K. Angioscopic evaluation of neointima coverage: Sirolimus-drug eluting stent versus bare metal stent. Am Heart J. 2006;152(6):1168-1174.
18. Serruys PW, Strauss BH, Beatt KJ, et al. Angiographic follow-up after placement of a self-expanding coronary-artery stent. N Engl J Med. 1991;324(1):13-17.
19. Schatz RA, Baim DS, Leon M, et al. Clinical experience with the Palmaz-Schatz coronary stent. Initial results of a multicenter study. Circulation. 1991:83(1):148-161.
20. Fischman DL, Leon MB, Baim DS, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331(8):496-501.
21. Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331(8):489-495.
22. Leon MD, Baim DS, Gordon P, et al. Clinical and angiographic results from the STent Anticoagulation Regimen Study (STARS) (abstr). Circulation. 1996;94(suppl I):I-685.
23. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: A report of the American College of Cardiology Foundation/American Heart Association Task Force of Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44-e122.
24. Bennett CL, Davidson CJ, Raisch DW, Weinberg PD, Bennett RH, Feldman MD. Thrombotic thrombocytopenic purpura associated with ticlopidine in the setting of coronary artery stents and stroke prevention. Arch Intern Med. 1999;159(21):2524-2528.
25. Bertrand ME, Rupprecht HJ, Urban P, Gershlick AH; CLASSICS Investigators. Double-blind study of the safety of clopidogrel with and without a loading dose in combination with aspirin compared with ticlopidine in combination with aspirin after coronary stenting: The clopidogrel aspirin stent international cooperative study (CLASSICS). Circulation. 2000;102(6):624-629.
26. Wang, TH, Bhatt DL, Topol EJ. Aspirin and clopidogrel resistance: An emerging clinical entity. Eur Heart J. 2006;27(6):647-654.
27. Vats HS, Hocking WG, Rezkalla SH. Suspected clopidogrel resistance in a patient with acute stent thrombosis. Nat Clin Pract Cardiovasc Med. 2006;3(4):226-230.
28. Gurbel PA, Becker RC, Mann KG, Steinhubl SR, Michelson AD. Platelet function monitoring in patients with coronary artery disease. J Am Coll Cardiol. 2007;50(19):1822-1834.
29. Fitzgerald DJ, Maree A. Aspirin and clopidogrel resistance. Hematology Am Soc Hematol Educ Program. 2007;2007(1):114-120.
30. Cattaneo M. Resistance to antiplatelet drugs: Molecular mechanisms and laboratory detection. J Thromb Haemost. 2007;5(suppl 1):230-237.
31. Trenk D, Hochholzer W, Fromm MF, et al. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008;51(20):1925-1934.
32. Kazui M, Nishiya Y, Ishizuka T, et al. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos. 2010;38(1):92-99.
33. Hulot JS, Bura A, Villard E, et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood. 2006;108(7):2244-2247.
34. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360(4):354-362.
35. U.S. Food and Drug Administration. Plavix (clopidogrel): Reduced effectiveness in patients who are poor metabolizers of the drug. U.S. Food and Drug Administration Website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm204256.htm. Updated September 6, 2013. Accessed September 4, 2014.
36. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Intensive oral antiplatelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary syndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: A subanalysis of a randomised trial. Lancet. 2008;371(9621):1353-1363.
37. Wallentin L, Becker RC, Budaj A, et al; PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
38. Wallentin L, Varenhorst C, James S, et al. Prasugrel achieves greater and faster P2Y12 receptor-mediated platelet inhibition than clopidogrel due to more efficient generation of its active metabolite in aspirin-treated patients with coronary artery disease. Eur Heart J. 2008;29(1):21-30.
39. Gurbel PA, Bliden KP, Butler K, et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: The ONSET/OFFSET study. Circulation. 2009;120(25):2577-2585.
40. Wiviott SD, Trenk D, Frelinger AL, et al; PRINCIPLE-TIMI 44 Investigators. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: The Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007;116(25):2923-2932.
41. Gurbel PA, Bliden KP, Butler K, et al. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: The RESPOND study. Circulation. 2010;121(10):1188-1199.
42. Spertus, JA, Kettelkamp R, Vance C, et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: Results from the PREMIER registry. Circulation. 2006;113(24):2803-2809.
43. Sharma AK, Ajani AE, Hamwi SM, et al. Major noncardiac surgery following coronary stenting: When is it safe to operate? Catheter Cardiovasc Interv. 2004;63(2):141-145.
44. Ben-Dor I, Torguson R, Scheinowitz M, et al. Incidence, correlates, and clinical impact of nuisance bleeding after antiplatelet therapy for patients with drug-eluting stents. Am Heart J. 2010;159(5):871-875.
45. Kaluza GL, Joseph J, Lee JR, Raizner ME, Raizner AE. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000;35(5):1288-1294.
46. Airoldi F, Colombo A, Morici N, et al. Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation. 2007;116(7):745-754.
47. Grines CL, Bonow RO, Casey DE Jr, et al; American Heart Association; American College of Cardiology; Society for Cardiovascular Angiography and Interventions; American College of Surgeons; American Dental Association; American College of Physicians. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: A science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49(6):734-739.
Percutaneous coronary intervention (PCI) using coronary artery stent implantation is commonly used to treat symptomatic high-risk and unstable coronary artery disease (CAD). The use of stents has improved the safety and efficacy of PCI by reducing the need for repeat revascularization, reducing acute vessel closure requiring emergent coronary artery bypass graft surgery, and expanding the use of PCI to more complex diseases. Nevertheless, stents carry the risk of sudden thrombotic occlusion or stent thrombosis, particularly during the first several days or weeks after implantation. In turn, stent thrombosis can lead to acute myocardial infarction (MI) and a mortality rate > 25%.1,2
This article highlights 2 cases of patients with stent thrombosis and discusses its pathophysiology, clinical features, and risk-avoidance strategies. Given the high prevalence of CAD and ubiquitous PCI procedures in the U.S. health care system, it is essential that not only cardiologists, but all clinicians and health care providers who care for patients with coronary stents understand how to help prevent and manage this life-threatening clinical entity.1
Case 1
A 56-year-old man presented to his primary care physician with exertion-related angina. The patient had a history of type 2 diabetes mellitus, dyslipidemia, systemic hypertension, obesity, and CAD status post MI in 2002 treated with a bare metal stent (BMS) to the left circumflex coronary artery (LCx). A stress myocardial perfusion imaging with 99mTc-sestamibi revealed moderate reversible exercise-induced myocardial ischemia involving the inferior and inferoapical wall segments of the left ventricle with associated hypokinesia.
Coronary angiography revealed nonsignificant disease of the left anterior descending artery (LAD) and LCx, a patent LCx stent, and a 95% mid-right coronary artery (RCA) obstruction with delayed (TIMI grade 2) antegrade flow. The distal right posterior descending artery filled via left to right collaterals from the LAD.
Percutaneous coronary intervention was performed on the RCA lesion 8 days after the patient was started on dual antiplatelet therapy (DAPT) with aspirin 81 mg and clopidogrel 75 mg (including 300 mg loading dose on the day of the diagnostic angiogram). The mid RCA was treated with a drug-eluting stent (DES) and a BMS in a nonoverlapping fashion with an excellent angiographic result. The patient was instructed to continue DAPT with aspirin 325 mg daily and clopidogrel 75 mg daily for 12 months.
Three days post PCI, the patient arrived at the emergency department with angina of 1-hour duration associated with shortness of breath and diaphoresis. He reported strict adherence to DAPT.
Initial vital signs were normal. The electrocardiogram (ECG) showed ST segment elevation (1-2 mm) on leads III, aVF, and V5 to V6, suggestive of an acute inferolateral injury pattern for which emergent coronary angiography was performed. Angiography showed a 100% proximal RCA occlusion at the proximal edge of the most proximal stent with absence of any antegrade flow beyond the occlusion (TIMI grade 0 flow). This finding was diagnostic of definite angiographic subacute stent thrombosis. The patient underwent successful aspiration thrombectomy, balloon angioplasty, and restoration of normal TIMI grade 3 flow with a door-to-balloon time of 86 minutes.
Because stent thrombosis is relatively unexpected after an excellent angiographic result and DAPT adherence, the possibility of clopidogrel resistance was considered as a major contributor for the thrombotic event. Platelet aggregation tests showed adequate prolongation of collagen/epinephrine (COL-EPI) > 300 seconds (normal: 81-153 seconds), but inadequate prolongation of collagen/adenosindiphosphate (COL-ADP) of 109 seconds (normal: 53-105 seconds) while on clopidogrel. Therefore, the patient was switched to prasugrel.
The patient was discharged home after 5 days of observation at the cardiac care unit without any post-MI complications. During a follow-up appointment 1 month after discharge, he was clinically stable and free of cardiovascular symptoms. Workup performed for acquired or inherited thrombophilia was negative. He continued taking DAPT (daily aspirin 325 mg orally and prasugrel 10 mg orally) for 12 months. After completing 12 months of DAPT, he was maintained on aspirin 81 mg daily. At 24 months’ follow-up, he remained free of recurrent angina with no further cardiovascular events.
Case 2
An 84-year-old man with a medical history of dyslipidemia, paroxysmal atrial fibrillation, previous stroke, and peptic ulcer disease was brought to the emergency department following an episode of near syncope in the early morning hours. The patient revealed that he had experienced neck pain since midnight. The 12-lead ECG showed normal sinus rhythm with 2 mm ST segment elevation in leads II, III, aVF, V5-V6, and ST segment depression in V2, and Q waves in inferior leads. A right-sided ECG showed ST segment elevation in V4, suggestive of right ventricle infarction.
The patient remained hypotensive (83/49 mm Hg) despite isotonic fluid administration (about 1.5-2.0 liters of 0.9 normal saline at 999 mL/h). A dopamine drip for persistent hypotension was started, and he was taken emergently to the catheterization laboratory for primary PCI. Coronary angiography showed no significant left CAD and a 100% mid-RCA occlusion with faint left-to-right collaterals. After aspiration thrombectomy, bare metal RCA stenting was performed. Transient no-reflow was treated with intracoronary nicardipine and nitroglycerin. The patient continued to be in shock, and an intra-aortic balloon pump was inserted and 1:1 counterpulsation was initiated.
Following admission to the coronary care unit, the patient’s mean arterial pressure improved. Inotropes were weaned off 2 days after PCI, and the intra-aortic balloon pump was removed. During his stay, the post-MI course was uneventful except for an episode of asymptomatic paroxysmal atrial flutter and nonspecific back dermatitis attributed to a prolonged recumbent position.
The patient was transferred to the internal medicine ward for medical therapy optimization and the initiation of low-intensity cardiac rehabilitation. After 2 days on the ward, discharge planning was initiated. However, he developed an episode of atrial fibrillation with fast ventricular response. Metoprolol 5 mg IV bolus was given, and the ventricular rate was controlled. At that point, the dose of long-acting beta-blocker (metoprolol succinate) was optimized, he was started on full-dose anticoagulation (warfarin), and clopidogrel was discontinued. Two days later, the patient reported back pruritus, and an erythematous raised rash on his back spreading to the torso was noticed. An aspirin allergy was suspected as the trigger for the rash, thus aspirin was also discontinued.
Three days later, the patient developed recurrent neck pain (angina) with radiation to his shoulders and left arm. The ECG revealed re-elevation of the ST segment (inferior, posterior, and lateral leads). He received reloading of clopidogrel 600 mg and aspirin 325 mg. Also, an eptifibatide IV bolus followed by an infusion was given for immediate antiplatelet action. He was transferred for emergent coronary angiography with suspected subacute stent thrombosis.
Upon arrival to the catheterization lab, the patient was awake and alert but in mild respiratory distress. Intravenous dopamine was started due to hypotension (systolic blood pressure was about 85 mm Hg). Limited RCA angiography showed a large clot burden with a partially thrombosed stent and TIMI grade 3 flow. After intracoronary eptifibatide and nicardipine were given, successful aspiration thrombectomy was performed twice with partial removal of thrombus. In-stent high-pressure balloon angioplasty was performed and optimal stenting was confirmed by intravascular ultrasound (IVUS) criteria. However, a residual layered thrombus along the distal stent edge was noticed. The patient tolerated the procedure without complications.
Dual antiplatelet therapy with aspirin and clopidogrel for 12 months was recommended. The eptifibatide infusion was continued for 48 hours. The jaw pain, shortness of breath, and ECG changes disappeared, but the patient remained on vasopressors for the following 7 days.
Around 1 week after the stent thrombosis event, the patient was found pulseless. Advanced cardiopulmonary resuscitation was started. ST segment elevation in lead II was noted on the cardiac monitor. There was no return of spontaneous circulation after 20 minutes, and the patient was pronounced dead. The autopsy revealed a patent RCA stent without evidence of occlusion, a large transmural inferior MI, left ventricular rupture, and hemopericardium.
Discussion
Stent thrombosis is an uncommon complication after coronary stent implantation. Based on the Academic Research Consortium criteria, definite stent thrombosis is defined as a clinical event with symptoms suggestive of an acute coronary syndrome (ACS) with angiography or pathology that confirms the presence of stent thrombosis.2 Probable stent thrombosis is defined as an unexplained death within 30 days or MI involving the territory of the target vessel without angiographic confirmation of stent thrombosis.2 Finally, possible stent thrombosis is any unexplained death after 30 days.2
Based on timing, stent thrombosis is divided by acute (< 24 hours post stent implantation), subacute (24 hours to 30 days post stent implantation), late (> 30 days post stent implantation), and very late (> 12 months post stent implantation).3 However, most cases (up to 60%) occur within the first 30 days after placement, irrespective of stent type.4
The incidence of subacute stent thrombosis is reported to approach 1% during the first 30 days postprocedure but may be as high as 5% or 10% depending on associated clinical and angiographic variables (Table 1).5 The strongest clinical predictors of stent thrombosis are premature cessation of antiplatelet therapy, renal insufficiency, diabetes mellitus, and ACS.2,6 Lesion and procedural characteristics associated with increased risk of stent thrombosis include bifurcation lesions, longer stent length, multiple implanted stents, stent underexpansion, and/or stent malapposition.6-9 Stent type (drug or non–drug-eluting) has no impact on the risk of stent thrombosis during the first 30 days postprocedure.10,11
The clinical events related to late stent thrombosis, although rare, carry a mortality rate of up to 45%.12 The specific risk factors for late and very late stent thrombosis are less well defined but relate to delayed neointimal coverage, ongoing vessel inflammation, and the development of neoatherosclerosis within stents.13,14
Rationale for the Use of Dual Antiplatelet Regimen
Stent thrombosis is a platelet-mediated process related to a heightened state of systemic and intracoronary thrombogenicity and inflammation.15 Stent under-expansion enhances abnormal shear stress, which explains as many as 80% of these events.13,15,16 Stent thrombosis also has been frequently related to inadequate neointimal coverage.14 Angioscopic studies, especially with DES, suggest that stent endothelialization is delayed or incomplete, observing a correlation between the areas of uncovered stent surface and thrombosis.14,17
In the early days of coronary stenting, during the 1990s, the risk of acute and subacute stent thrombosis approached 20%.18,19 Initial attempts to reduce the risk included combining aspirin and warfarin, but at the expense of a marked increase in bleeding complications and prolonged hospital stays.20,21 In 1995, it became clear through the pivotal observations of Colombo and colleagues that incomplete expansion of the stent (documented by IVUS) was a major contributor to the risk of stent thrombosis.16 By using noncompliant balloons at high pressure (14-20 atmospheres) for stent postdilatation combined with DAPT (aspirin and ticlopidine), the high rates of early stent thrombosis were markedly reduced to the current level of 1% to 2%.16
Colombo and colleagues’ observations were prospectively evaluated in the Stent Anticoagulation Regimen Study (STARS) trial.22 Patients who underwent successful stenting were randomized to aspirin alone, aspirin and warfarin, or aspirin and ticlopidine. The STARS trial showed convincingly that the combination of aspirin and ticlopidine was superior to the other 2 regimens, reducing the stent thrombosis rate to only 0.5% (compared with 2.7% for aspirin and warfarin, and 3.6% for aspirin alone).22 Afterward, DAPT became the standard of care following coronary stenting.23
Although ticlopidine was the first widely used thienopyridine for the prevention of stent thrombosis, hematologic adverse events (AEs) (eg, neutropenia, thrombotic thrombocytopenia purpura) limited its use.24 Consequently, ticlopidine was replaced with clopidogrel, which seemed to offer similar efficacy but significantly fewer AEs.25
The current American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines for the prevention of ST after coronary stent implantation state that after PCI:
- Aspirin use should be continued indefinitely.
- The duration of adenosine diphosphate antagonists depends on the stent type (BMS or DES) and the indication for implantation (ACS or non-ACS).
a. Patients receiving a stent (BMS or DES) for ACS therapy should be given 1 of the following for at least 12 months:
i. Clopidogrel 75 mg daily
ii. Prasugrel 10 mg daily
iii. Ticagrelor 90 mg twice daily
b. In patients receiving DES for a non-ACS indication, clopidogrel should be given for at least 12 months if the patient is not at high risk for bleeding.
c. In patients receiving BMS for a non-ACS indication, clopidogrel should be given for a minimum of 1 month and ideally up to 12 months.23
Clopidogrel Hyporesponse
As shown in case 1, stent thrombosis may still occur in a patient on DAPT because of individual variability in platelet response to clopidogrel.5 Clopidogrel hyporesponse, also known as clopidogrel resistance, has been recognized as clinically significant because of its prevalence and association with poor outcomes.5 Its prevalence may range between 4% and 30%, although the definitions of clopidogrel hyporesponse varied between studies.26
Clopidogrel hyporesponse is defined as an inadequate inhibition of platelet function measured by nonspecific ex-vivo laboratory methods.27,28 The relationship between clopidogrel resistance (nonresponders), stent thrombosis, and ischemic events has been clearly established.5,29
Given the devastating consequences of stent thrombosis, efforts were directed to identify those patients at highest risk. One such effort has been focused on the measurement of platelet function, allowing for the identification of patients who do not respond adequately to antiplatelet therapy.15,28,30,31 However, the treatment of high-residual platelet reactivity as confirmed by laboratory assessment has not shown to clinically correlate with any benefit in the prevention of ST.6,15,29-31 Therefore, the current ACC/AHA/SCAI PCI guidelines do not recommend the routine clinical use of platelet function testing to screen patients treated with clopidogrel who are undergoing PCI.23
Clopidogrel is a prodrug, metabolized to its active form via the cytochrome P450 enzyme system before it can inhibit platelet function.32 Accordingly, certain genetic variation in enzyme activity, or polymorphisms, would be expected to influence its clinical effectiveness.33,34 The most common of these polymorphisms, CYP2C19*2, has been associated (in vitro) with reduced concentrations of active clopidogrel metabolites and with diminished platelet inhibition.35,36 As a result, the FDA has added a safety alert to the prescribing information for clopidogrel concerning how genetic differences in the metabolism of this agent can affect its effectiveness, ways to test for these genetic differences, and advice concerning alternative dosing strategies or use of other medications in poor metabolizers of clopidogrel.37 Although the routine clinical use of genetic testing to screen patients treated with clopidogrel who are undergoing PCI is not recommended, it may be considered in patients undergoing elective high-risk PCI procedures (eg, unprotected left main, last patent coronary artery, or bifurcating left main).23
The newer inhibitors of ADP-induced platelet activation, prasugrel and ticagrelor, are not prodrugs, and thus, their action is not affected by this genetic variability. Accordingly, these drugs have shown a more consistent, stronger, and faster inhibition of platelet aggregation compared with clopidogrel.36-39 In the pivotal trials (TRITON-TIMI 38 and PLATO), these agents have also been shown to be more effective in reducing the incidence of stent thrombosis.36,37,40,41 Therefore, in cases where clopidogrel resistance/hyporesponse is suspected in the setting of DAPT, such as stent thrombosis, guidelines recommend the use of 1 of these agents.23
Premature Discontinuation of Antiplatelet Therapy
As illustrated in case 2, premature discontinuation of antiplatelet therapy may be fatal, as it is associated with a marked increase in the risk of stent thrombosis. Indeed, premature discontinuation of DAPT is the leading independent predictor for stent thrombosis.12,42,43 Premature discontinuation of DAPT is defined when one or both agents (aspirin, ADP-antagonists) are suspended within 30 days of BMS placement or within 1 year of DES placement. In the case of DES, the first 6 months after implantation seem to be most critical. In a large observational study of patients treated with DES, stent thrombosis occurred in 29% of those patients in whom antiplatelet therapy was prematurely discontinued.12
In order to minimize the risk of premature DAPT discontinuation, one should address its causes. There are patient- and physician-related factors that may influence an early discontinuation of aspirin, thienopyridine, or both agents. Patient-related factors were identified in the PREMIER registry, including older age, not having completed high school, not being married, and/or not seeking health care because of costs.42 Another important but often overlooked factor that has an impact on adherence with prolonged DAPT post-DES implantation is nuisance or superficial bleeding.44 Physician-related factors include not providing discharge instructions for medication use and ill-advised instructions given by health care providers to discontinue therapy before procedures with a low risk of bleeding (eg, dental cleaning, cataract surgery, colonoscopy, skin biopsy).42
In addition, the perioperative management of DAPT during the first several weeks after coronary stenting has been shown to critically influence outcomes. In a study by Sharma and colleagues, fatal cases of stent thrombosis occurred after the discontinuation of antiplatelet therapy for noncardiac surgery among patients with BMS implantation within the past 90 days.43
In selected cases when a noncardiac procedure cannot be delayed for 1 year, recognizing the impact of the specific timing for the discontinuation of the antiplatelet regimen is essential. Kaluza and colleagues reported on 40 patients treated with BMS who underwent noncardiac surgery within 6 weeks of the stent implantation.45 Seven patients had an MI, of which 6 were fatal. Stent thrombosis was presumed to be the cause of all MIs. In 5 of 7 cases, ticlopidine was withheld before surgery.45
All clinicians should be aware of the following recommendations to avoid catastrophic cardiovascular complications related to premature discontinuation of DAPT during the perioperative setting:
- Elective procedures should be deferred until patients have completed an appropriate course of thienopyridine therapy (12 months after DES and a minimum of 4 weeks for BMS implantation).
- For those patients treated with DES who are to undergo a nonelective procedure that mandates discontinuation of thienopyridine therapy, the possibility of procedure postponement for completion of DAPT for at least 6 months should be judiciously deliberated. If the procedure cannot be postponed, aspirin should be continued if at all possible and the thienopyridine restarted as soon as possible after the procedure.42,46,47
Conclusion
Stent thrombosis is a rare but devastating complication of coronary stent implantation. Although it can occur at any time after stent placement, the majority of events occur within the first month. The use of optimal stenting techniques and adherence to DAPT are required to minimize the risk of stent thrombosis. Several clinical and procedural predictors have been related to an increased risk of stent thrombosis. The premature cessation of DAPT is the most important risk factor for stent thrombosis.
All physicians should ensure patients are properly and thoroughly educated about the reasons they are prescribed DAPT and the significant risks associated with prematurely discontinuing such therapy. All clinicians, especially noncardiologists, should realize the importance of close communication with a cardiologist or interventional cardiologist in situations when premature discontinuation is being considered for a specific reason.
Table 2 summarizes a framework of the most relevant factors that should be taken into account before, during, and after stent implantation, both by interventional cardiologists, as well as by all clinicians involved in the care of the patient. Given current procedural volumes (> 1 million PCI procedures are performed in the U.S. annually) and because the risk of stent thrombosis is both time and treatment dependent, it is of paramount importance that, not only cardiologists, but all physicians know the impact of stent thrombosis in their patients and how to avoid situations that may increase its risk.1 Team-approach decisions about antiplatelet therapy after stent placement, especially within the first 12 months, and a patient-centered mind-set are indispensable to optimize patient outcomes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Percutaneous coronary intervention (PCI) using coronary artery stent implantation is commonly used to treat symptomatic high-risk and unstable coronary artery disease (CAD). The use of stents has improved the safety and efficacy of PCI by reducing the need for repeat revascularization, reducing acute vessel closure requiring emergent coronary artery bypass graft surgery, and expanding the use of PCI to more complex diseases. Nevertheless, stents carry the risk of sudden thrombotic occlusion or stent thrombosis, particularly during the first several days or weeks after implantation. In turn, stent thrombosis can lead to acute myocardial infarction (MI) and a mortality rate > 25%.1,2
This article highlights 2 cases of patients with stent thrombosis and discusses its pathophysiology, clinical features, and risk-avoidance strategies. Given the high prevalence of CAD and ubiquitous PCI procedures in the U.S. health care system, it is essential that not only cardiologists, but all clinicians and health care providers who care for patients with coronary stents understand how to help prevent and manage this life-threatening clinical entity.1
Case 1
A 56-year-old man presented to his primary care physician with exertion-related angina. The patient had a history of type 2 diabetes mellitus, dyslipidemia, systemic hypertension, obesity, and CAD status post MI in 2002 treated with a bare metal stent (BMS) to the left circumflex coronary artery (LCx). A stress myocardial perfusion imaging with 99mTc-sestamibi revealed moderate reversible exercise-induced myocardial ischemia involving the inferior and inferoapical wall segments of the left ventricle with associated hypokinesia.
Coronary angiography revealed nonsignificant disease of the left anterior descending artery (LAD) and LCx, a patent LCx stent, and a 95% mid-right coronary artery (RCA) obstruction with delayed (TIMI grade 2) antegrade flow. The distal right posterior descending artery filled via left to right collaterals from the LAD.
Percutaneous coronary intervention was performed on the RCA lesion 8 days after the patient was started on dual antiplatelet therapy (DAPT) with aspirin 81 mg and clopidogrel 75 mg (including 300 mg loading dose on the day of the diagnostic angiogram). The mid RCA was treated with a drug-eluting stent (DES) and a BMS in a nonoverlapping fashion with an excellent angiographic result. The patient was instructed to continue DAPT with aspirin 325 mg daily and clopidogrel 75 mg daily for 12 months.
Three days post PCI, the patient arrived at the emergency department with angina of 1-hour duration associated with shortness of breath and diaphoresis. He reported strict adherence to DAPT.
Initial vital signs were normal. The electrocardiogram (ECG) showed ST segment elevation (1-2 mm) on leads III, aVF, and V5 to V6, suggestive of an acute inferolateral injury pattern for which emergent coronary angiography was performed. Angiography showed a 100% proximal RCA occlusion at the proximal edge of the most proximal stent with absence of any antegrade flow beyond the occlusion (TIMI grade 0 flow). This finding was diagnostic of definite angiographic subacute stent thrombosis. The patient underwent successful aspiration thrombectomy, balloon angioplasty, and restoration of normal TIMI grade 3 flow with a door-to-balloon time of 86 minutes.
Because stent thrombosis is relatively unexpected after an excellent angiographic result and DAPT adherence, the possibility of clopidogrel resistance was considered as a major contributor for the thrombotic event. Platelet aggregation tests showed adequate prolongation of collagen/epinephrine (COL-EPI) > 300 seconds (normal: 81-153 seconds), but inadequate prolongation of collagen/adenosindiphosphate (COL-ADP) of 109 seconds (normal: 53-105 seconds) while on clopidogrel. Therefore, the patient was switched to prasugrel.
The patient was discharged home after 5 days of observation at the cardiac care unit without any post-MI complications. During a follow-up appointment 1 month after discharge, he was clinically stable and free of cardiovascular symptoms. Workup performed for acquired or inherited thrombophilia was negative. He continued taking DAPT (daily aspirin 325 mg orally and prasugrel 10 mg orally) for 12 months. After completing 12 months of DAPT, he was maintained on aspirin 81 mg daily. At 24 months’ follow-up, he remained free of recurrent angina with no further cardiovascular events.
Case 2
An 84-year-old man with a medical history of dyslipidemia, paroxysmal atrial fibrillation, previous stroke, and peptic ulcer disease was brought to the emergency department following an episode of near syncope in the early morning hours. The patient revealed that he had experienced neck pain since midnight. The 12-lead ECG showed normal sinus rhythm with 2 mm ST segment elevation in leads II, III, aVF, V5-V6, and ST segment depression in V2, and Q waves in inferior leads. A right-sided ECG showed ST segment elevation in V4, suggestive of right ventricle infarction.
The patient remained hypotensive (83/49 mm Hg) despite isotonic fluid administration (about 1.5-2.0 liters of 0.9 normal saline at 999 mL/h). A dopamine drip for persistent hypotension was started, and he was taken emergently to the catheterization laboratory for primary PCI. Coronary angiography showed no significant left CAD and a 100% mid-RCA occlusion with faint left-to-right collaterals. After aspiration thrombectomy, bare metal RCA stenting was performed. Transient no-reflow was treated with intracoronary nicardipine and nitroglycerin. The patient continued to be in shock, and an intra-aortic balloon pump was inserted and 1:1 counterpulsation was initiated.
Following admission to the coronary care unit, the patient’s mean arterial pressure improved. Inotropes were weaned off 2 days after PCI, and the intra-aortic balloon pump was removed. During his stay, the post-MI course was uneventful except for an episode of asymptomatic paroxysmal atrial flutter and nonspecific back dermatitis attributed to a prolonged recumbent position.
The patient was transferred to the internal medicine ward for medical therapy optimization and the initiation of low-intensity cardiac rehabilitation. After 2 days on the ward, discharge planning was initiated. However, he developed an episode of atrial fibrillation with fast ventricular response. Metoprolol 5 mg IV bolus was given, and the ventricular rate was controlled. At that point, the dose of long-acting beta-blocker (metoprolol succinate) was optimized, he was started on full-dose anticoagulation (warfarin), and clopidogrel was discontinued. Two days later, the patient reported back pruritus, and an erythematous raised rash on his back spreading to the torso was noticed. An aspirin allergy was suspected as the trigger for the rash, thus aspirin was also discontinued.
Three days later, the patient developed recurrent neck pain (angina) with radiation to his shoulders and left arm. The ECG revealed re-elevation of the ST segment (inferior, posterior, and lateral leads). He received reloading of clopidogrel 600 mg and aspirin 325 mg. Also, an eptifibatide IV bolus followed by an infusion was given for immediate antiplatelet action. He was transferred for emergent coronary angiography with suspected subacute stent thrombosis.
Upon arrival to the catheterization lab, the patient was awake and alert but in mild respiratory distress. Intravenous dopamine was started due to hypotension (systolic blood pressure was about 85 mm Hg). Limited RCA angiography showed a large clot burden with a partially thrombosed stent and TIMI grade 3 flow. After intracoronary eptifibatide and nicardipine were given, successful aspiration thrombectomy was performed twice with partial removal of thrombus. In-stent high-pressure balloon angioplasty was performed and optimal stenting was confirmed by intravascular ultrasound (IVUS) criteria. However, a residual layered thrombus along the distal stent edge was noticed. The patient tolerated the procedure without complications.
Dual antiplatelet therapy with aspirin and clopidogrel for 12 months was recommended. The eptifibatide infusion was continued for 48 hours. The jaw pain, shortness of breath, and ECG changes disappeared, but the patient remained on vasopressors for the following 7 days.
Around 1 week after the stent thrombosis event, the patient was found pulseless. Advanced cardiopulmonary resuscitation was started. ST segment elevation in lead II was noted on the cardiac monitor. There was no return of spontaneous circulation after 20 minutes, and the patient was pronounced dead. The autopsy revealed a patent RCA stent without evidence of occlusion, a large transmural inferior MI, left ventricular rupture, and hemopericardium.
Discussion
Stent thrombosis is an uncommon complication after coronary stent implantation. Based on the Academic Research Consortium criteria, definite stent thrombosis is defined as a clinical event with symptoms suggestive of an acute coronary syndrome (ACS) with angiography or pathology that confirms the presence of stent thrombosis.2 Probable stent thrombosis is defined as an unexplained death within 30 days or MI involving the territory of the target vessel without angiographic confirmation of stent thrombosis.2 Finally, possible stent thrombosis is any unexplained death after 30 days.2
Based on timing, stent thrombosis is divided by acute (< 24 hours post stent implantation), subacute (24 hours to 30 days post stent implantation), late (> 30 days post stent implantation), and very late (> 12 months post stent implantation).3 However, most cases (up to 60%) occur within the first 30 days after placement, irrespective of stent type.4
The incidence of subacute stent thrombosis is reported to approach 1% during the first 30 days postprocedure but may be as high as 5% or 10% depending on associated clinical and angiographic variables (Table 1).5 The strongest clinical predictors of stent thrombosis are premature cessation of antiplatelet therapy, renal insufficiency, diabetes mellitus, and ACS.2,6 Lesion and procedural characteristics associated with increased risk of stent thrombosis include bifurcation lesions, longer stent length, multiple implanted stents, stent underexpansion, and/or stent malapposition.6-9 Stent type (drug or non–drug-eluting) has no impact on the risk of stent thrombosis during the first 30 days postprocedure.10,11
The clinical events related to late stent thrombosis, although rare, carry a mortality rate of up to 45%.12 The specific risk factors for late and very late stent thrombosis are less well defined but relate to delayed neointimal coverage, ongoing vessel inflammation, and the development of neoatherosclerosis within stents.13,14
Rationale for the Use of Dual Antiplatelet Regimen
Stent thrombosis is a platelet-mediated process related to a heightened state of systemic and intracoronary thrombogenicity and inflammation.15 Stent under-expansion enhances abnormal shear stress, which explains as many as 80% of these events.13,15,16 Stent thrombosis also has been frequently related to inadequate neointimal coverage.14 Angioscopic studies, especially with DES, suggest that stent endothelialization is delayed or incomplete, observing a correlation between the areas of uncovered stent surface and thrombosis.14,17
In the early days of coronary stenting, during the 1990s, the risk of acute and subacute stent thrombosis approached 20%.18,19 Initial attempts to reduce the risk included combining aspirin and warfarin, but at the expense of a marked increase in bleeding complications and prolonged hospital stays.20,21 In 1995, it became clear through the pivotal observations of Colombo and colleagues that incomplete expansion of the stent (documented by IVUS) was a major contributor to the risk of stent thrombosis.16 By using noncompliant balloons at high pressure (14-20 atmospheres) for stent postdilatation combined with DAPT (aspirin and ticlopidine), the high rates of early stent thrombosis were markedly reduced to the current level of 1% to 2%.16
Colombo and colleagues’ observations were prospectively evaluated in the Stent Anticoagulation Regimen Study (STARS) trial.22 Patients who underwent successful stenting were randomized to aspirin alone, aspirin and warfarin, or aspirin and ticlopidine. The STARS trial showed convincingly that the combination of aspirin and ticlopidine was superior to the other 2 regimens, reducing the stent thrombosis rate to only 0.5% (compared with 2.7% for aspirin and warfarin, and 3.6% for aspirin alone).22 Afterward, DAPT became the standard of care following coronary stenting.23
Although ticlopidine was the first widely used thienopyridine for the prevention of stent thrombosis, hematologic adverse events (AEs) (eg, neutropenia, thrombotic thrombocytopenia purpura) limited its use.24 Consequently, ticlopidine was replaced with clopidogrel, which seemed to offer similar efficacy but significantly fewer AEs.25
The current American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines for the prevention of ST after coronary stent implantation state that after PCI:
- Aspirin use should be continued indefinitely.
- The duration of adenosine diphosphate antagonists depends on the stent type (BMS or DES) and the indication for implantation (ACS or non-ACS).
a. Patients receiving a stent (BMS or DES) for ACS therapy should be given 1 of the following for at least 12 months:
i. Clopidogrel 75 mg daily
ii. Prasugrel 10 mg daily
iii. Ticagrelor 90 mg twice daily
b. In patients receiving DES for a non-ACS indication, clopidogrel should be given for at least 12 months if the patient is not at high risk for bleeding.
c. In patients receiving BMS for a non-ACS indication, clopidogrel should be given for a minimum of 1 month and ideally up to 12 months.23
Clopidogrel Hyporesponse
As shown in case 1, stent thrombosis may still occur in a patient on DAPT because of individual variability in platelet response to clopidogrel.5 Clopidogrel hyporesponse, also known as clopidogrel resistance, has been recognized as clinically significant because of its prevalence and association with poor outcomes.5 Its prevalence may range between 4% and 30%, although the definitions of clopidogrel hyporesponse varied between studies.26
Clopidogrel hyporesponse is defined as an inadequate inhibition of platelet function measured by nonspecific ex-vivo laboratory methods.27,28 The relationship between clopidogrel resistance (nonresponders), stent thrombosis, and ischemic events has been clearly established.5,29
Given the devastating consequences of stent thrombosis, efforts were directed to identify those patients at highest risk. One such effort has been focused on the measurement of platelet function, allowing for the identification of patients who do not respond adequately to antiplatelet therapy.15,28,30,31 However, the treatment of high-residual platelet reactivity as confirmed by laboratory assessment has not shown to clinically correlate with any benefit in the prevention of ST.6,15,29-31 Therefore, the current ACC/AHA/SCAI PCI guidelines do not recommend the routine clinical use of platelet function testing to screen patients treated with clopidogrel who are undergoing PCI.23
Clopidogrel is a prodrug, metabolized to its active form via the cytochrome P450 enzyme system before it can inhibit platelet function.32 Accordingly, certain genetic variation in enzyme activity, or polymorphisms, would be expected to influence its clinical effectiveness.33,34 The most common of these polymorphisms, CYP2C19*2, has been associated (in vitro) with reduced concentrations of active clopidogrel metabolites and with diminished platelet inhibition.35,36 As a result, the FDA has added a safety alert to the prescribing information for clopidogrel concerning how genetic differences in the metabolism of this agent can affect its effectiveness, ways to test for these genetic differences, and advice concerning alternative dosing strategies or use of other medications in poor metabolizers of clopidogrel.37 Although the routine clinical use of genetic testing to screen patients treated with clopidogrel who are undergoing PCI is not recommended, it may be considered in patients undergoing elective high-risk PCI procedures (eg, unprotected left main, last patent coronary artery, or bifurcating left main).23
The newer inhibitors of ADP-induced platelet activation, prasugrel and ticagrelor, are not prodrugs, and thus, their action is not affected by this genetic variability. Accordingly, these drugs have shown a more consistent, stronger, and faster inhibition of platelet aggregation compared with clopidogrel.36-39 In the pivotal trials (TRITON-TIMI 38 and PLATO), these agents have also been shown to be more effective in reducing the incidence of stent thrombosis.36,37,40,41 Therefore, in cases where clopidogrel resistance/hyporesponse is suspected in the setting of DAPT, such as stent thrombosis, guidelines recommend the use of 1 of these agents.23
Premature Discontinuation of Antiplatelet Therapy
As illustrated in case 2, premature discontinuation of antiplatelet therapy may be fatal, as it is associated with a marked increase in the risk of stent thrombosis. Indeed, premature discontinuation of DAPT is the leading independent predictor for stent thrombosis.12,42,43 Premature discontinuation of DAPT is defined when one or both agents (aspirin, ADP-antagonists) are suspended within 30 days of BMS placement or within 1 year of DES placement. In the case of DES, the first 6 months after implantation seem to be most critical. In a large observational study of patients treated with DES, stent thrombosis occurred in 29% of those patients in whom antiplatelet therapy was prematurely discontinued.12
In order to minimize the risk of premature DAPT discontinuation, one should address its causes. There are patient- and physician-related factors that may influence an early discontinuation of aspirin, thienopyridine, or both agents. Patient-related factors were identified in the PREMIER registry, including older age, not having completed high school, not being married, and/or not seeking health care because of costs.42 Another important but often overlooked factor that has an impact on adherence with prolonged DAPT post-DES implantation is nuisance or superficial bleeding.44 Physician-related factors include not providing discharge instructions for medication use and ill-advised instructions given by health care providers to discontinue therapy before procedures with a low risk of bleeding (eg, dental cleaning, cataract surgery, colonoscopy, skin biopsy).42
In addition, the perioperative management of DAPT during the first several weeks after coronary stenting has been shown to critically influence outcomes. In a study by Sharma and colleagues, fatal cases of stent thrombosis occurred after the discontinuation of antiplatelet therapy for noncardiac surgery among patients with BMS implantation within the past 90 days.43
In selected cases when a noncardiac procedure cannot be delayed for 1 year, recognizing the impact of the specific timing for the discontinuation of the antiplatelet regimen is essential. Kaluza and colleagues reported on 40 patients treated with BMS who underwent noncardiac surgery within 6 weeks of the stent implantation.45 Seven patients had an MI, of which 6 were fatal. Stent thrombosis was presumed to be the cause of all MIs. In 5 of 7 cases, ticlopidine was withheld before surgery.45
All clinicians should be aware of the following recommendations to avoid catastrophic cardiovascular complications related to premature discontinuation of DAPT during the perioperative setting:
- Elective procedures should be deferred until patients have completed an appropriate course of thienopyridine therapy (12 months after DES and a minimum of 4 weeks for BMS implantation).
- For those patients treated with DES who are to undergo a nonelective procedure that mandates discontinuation of thienopyridine therapy, the possibility of procedure postponement for completion of DAPT for at least 6 months should be judiciously deliberated. If the procedure cannot be postponed, aspirin should be continued if at all possible and the thienopyridine restarted as soon as possible after the procedure.42,46,47
Conclusion
Stent thrombosis is a rare but devastating complication of coronary stent implantation. Although it can occur at any time after stent placement, the majority of events occur within the first month. The use of optimal stenting techniques and adherence to DAPT are required to minimize the risk of stent thrombosis. Several clinical and procedural predictors have been related to an increased risk of stent thrombosis. The premature cessation of DAPT is the most important risk factor for stent thrombosis.
All physicians should ensure patients are properly and thoroughly educated about the reasons they are prescribed DAPT and the significant risks associated with prematurely discontinuing such therapy. All clinicians, especially noncardiologists, should realize the importance of close communication with a cardiologist or interventional cardiologist in situations when premature discontinuation is being considered for a specific reason.
Table 2 summarizes a framework of the most relevant factors that should be taken into account before, during, and after stent implantation, both by interventional cardiologists, as well as by all clinicians involved in the care of the patient. Given current procedural volumes (> 1 million PCI procedures are performed in the U.S. annually) and because the risk of stent thrombosis is both time and treatment dependent, it is of paramount importance that, not only cardiologists, but all physicians know the impact of stent thrombosis in their patients and how to avoid situations that may increase its risk.1 Team-approach decisions about antiplatelet therapy after stent placement, especially within the first 12 months, and a patient-centered mind-set are indispensable to optimize patient outcomes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Ryan J, Cohen DJ. Are drug-eluting stents cost-effective? It depends on whom you ask. Circulation. 2006;114(16):1736-1744.
2. Cutlip DE, Windecker S, Mehran R, et al; Academic Research Consortium. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation. 2007;115(17):2344-2351.
3. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK; Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494-502.
4. Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: Meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012;5(3):357-364.
5. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, et al. Variability in individual responsiveness to clopidogrel: Clinical implications, management, and future perspectives. J Am Coll Cardiol. 2007;49(14):1505-1516.
6. Moussa I, Di Mario C, Reimers B, Akiyama T, Tobis J, Colombo A. Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: Frequency, predictors and clinical outcome. J Am Coll Cardiol. 1997;29(1):6-12.
7. Fujii K, Carlier SG, Mintz GS, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: An intravascular ultrasound study. J Am Coll Cardiol. 2005;45(7):995-998.
8. Uren NG, Schwarzacher SP, Metz JA, et al; POST Registry Investigators. Predictors and outcomes of stent thrombosis: An intravascular ultrasound registry. Eur Heart J. 2002;23(2):124-132.
9. Cook S, Wenaweser P, Togni M, et al. Intravascular ultrasound in very late DES-stent thrombosis (abstr). J Am Coll Cardiol. 2006;47(suppl B):9B.
10. Moreno R, Fernández C, Hernández R, et al. Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies. J Am Coll Cardiol. 2005;45(6):954-959.
11. Ellis SG, Colombo A, Grube E, et al. Incidence, timing, and correlates of stent thrombosis with the polymeric paclitaxel drug-eluting stent: A TAXUS II, IV, V, and VI meta-analysis of 3,445 patients followed for up to 3 years. J Am Coll Cardiol. 2007;49(10):1043-1051.
12. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126-2130.
13. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: A pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001;103(15):1967-1971.
14. Kotani J, Awata M, Nanto S, et al. Incomplete neointimal coverage of sirolimus-eluting stents: Angioscopic findings. J Am Coll Cardiol. 2006;47(10):2108–2111.
15. Cheneau E, Leborgne L, Mintz GS, et al. Predictors of subacute stent thrombosis: Results of a systematic intravascular ultrasound study. Circulation. 2003;108(1):43-47.
16. Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation achieved with intravascular ultrasound guidance. Circulation. 1995;91(6):1676-1688.
17. Oyabu J, Ueda Y, Ogasawara N, Okada K, Hirayama A, Kodama K. Angioscopic evaluation of neointima coverage: Sirolimus-drug eluting stent versus bare metal stent. Am Heart J. 2006;152(6):1168-1174.
18. Serruys PW, Strauss BH, Beatt KJ, et al. Angiographic follow-up after placement of a self-expanding coronary-artery stent. N Engl J Med. 1991;324(1):13-17.
19. Schatz RA, Baim DS, Leon M, et al. Clinical experience with the Palmaz-Schatz coronary stent. Initial results of a multicenter study. Circulation. 1991:83(1):148-161.
20. Fischman DL, Leon MB, Baim DS, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331(8):496-501.
21. Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331(8):489-495.
22. Leon MD, Baim DS, Gordon P, et al. Clinical and angiographic results from the STent Anticoagulation Regimen Study (STARS) (abstr). Circulation. 1996;94(suppl I):I-685.
23. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: A report of the American College of Cardiology Foundation/American Heart Association Task Force of Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44-e122.
24. Bennett CL, Davidson CJ, Raisch DW, Weinberg PD, Bennett RH, Feldman MD. Thrombotic thrombocytopenic purpura associated with ticlopidine in the setting of coronary artery stents and stroke prevention. Arch Intern Med. 1999;159(21):2524-2528.
25. Bertrand ME, Rupprecht HJ, Urban P, Gershlick AH; CLASSICS Investigators. Double-blind study of the safety of clopidogrel with and without a loading dose in combination with aspirin compared with ticlopidine in combination with aspirin after coronary stenting: The clopidogrel aspirin stent international cooperative study (CLASSICS). Circulation. 2000;102(6):624-629.
26. Wang, TH, Bhatt DL, Topol EJ. Aspirin and clopidogrel resistance: An emerging clinical entity. Eur Heart J. 2006;27(6):647-654.
27. Vats HS, Hocking WG, Rezkalla SH. Suspected clopidogrel resistance in a patient with acute stent thrombosis. Nat Clin Pract Cardiovasc Med. 2006;3(4):226-230.
28. Gurbel PA, Becker RC, Mann KG, Steinhubl SR, Michelson AD. Platelet function monitoring in patients with coronary artery disease. J Am Coll Cardiol. 2007;50(19):1822-1834.
29. Fitzgerald DJ, Maree A. Aspirin and clopidogrel resistance. Hematology Am Soc Hematol Educ Program. 2007;2007(1):114-120.
30. Cattaneo M. Resistance to antiplatelet drugs: Molecular mechanisms and laboratory detection. J Thromb Haemost. 2007;5(suppl 1):230-237.
31. Trenk D, Hochholzer W, Fromm MF, et al. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008;51(20):1925-1934.
32. Kazui M, Nishiya Y, Ishizuka T, et al. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos. 2010;38(1):92-99.
33. Hulot JS, Bura A, Villard E, et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood. 2006;108(7):2244-2247.
34. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360(4):354-362.
35. U.S. Food and Drug Administration. Plavix (clopidogrel): Reduced effectiveness in patients who are poor metabolizers of the drug. U.S. Food and Drug Administration Website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm204256.htm. Updated September 6, 2013. Accessed September 4, 2014.
36. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Intensive oral antiplatelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary syndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: A subanalysis of a randomised trial. Lancet. 2008;371(9621):1353-1363.
37. Wallentin L, Becker RC, Budaj A, et al; PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
38. Wallentin L, Varenhorst C, James S, et al. Prasugrel achieves greater and faster P2Y12 receptor-mediated platelet inhibition than clopidogrel due to more efficient generation of its active metabolite in aspirin-treated patients with coronary artery disease. Eur Heart J. 2008;29(1):21-30.
39. Gurbel PA, Bliden KP, Butler K, et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: The ONSET/OFFSET study. Circulation. 2009;120(25):2577-2585.
40. Wiviott SD, Trenk D, Frelinger AL, et al; PRINCIPLE-TIMI 44 Investigators. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: The Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007;116(25):2923-2932.
41. Gurbel PA, Bliden KP, Butler K, et al. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: The RESPOND study. Circulation. 2010;121(10):1188-1199.
42. Spertus, JA, Kettelkamp R, Vance C, et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: Results from the PREMIER registry. Circulation. 2006;113(24):2803-2809.
43. Sharma AK, Ajani AE, Hamwi SM, et al. Major noncardiac surgery following coronary stenting: When is it safe to operate? Catheter Cardiovasc Interv. 2004;63(2):141-145.
44. Ben-Dor I, Torguson R, Scheinowitz M, et al. Incidence, correlates, and clinical impact of nuisance bleeding after antiplatelet therapy for patients with drug-eluting stents. Am Heart J. 2010;159(5):871-875.
45. Kaluza GL, Joseph J, Lee JR, Raizner ME, Raizner AE. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000;35(5):1288-1294.
46. Airoldi F, Colombo A, Morici N, et al. Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation. 2007;116(7):745-754.
47. Grines CL, Bonow RO, Casey DE Jr, et al; American Heart Association; American College of Cardiology; Society for Cardiovascular Angiography and Interventions; American College of Surgeons; American Dental Association; American College of Physicians. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: A science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49(6):734-739.
1. Ryan J, Cohen DJ. Are drug-eluting stents cost-effective? It depends on whom you ask. Circulation. 2006;114(16):1736-1744.
2. Cutlip DE, Windecker S, Mehran R, et al; Academic Research Consortium. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation. 2007;115(17):2344-2351.
3. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK; Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494-502.
4. Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: Meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012;5(3):357-364.
5. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, et al. Variability in individual responsiveness to clopidogrel: Clinical implications, management, and future perspectives. J Am Coll Cardiol. 2007;49(14):1505-1516.
6. Moussa I, Di Mario C, Reimers B, Akiyama T, Tobis J, Colombo A. Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: Frequency, predictors and clinical outcome. J Am Coll Cardiol. 1997;29(1):6-12.
7. Fujii K, Carlier SG, Mintz GS, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: An intravascular ultrasound study. J Am Coll Cardiol. 2005;45(7):995-998.
8. Uren NG, Schwarzacher SP, Metz JA, et al; POST Registry Investigators. Predictors and outcomes of stent thrombosis: An intravascular ultrasound registry. Eur Heart J. 2002;23(2):124-132.
9. Cook S, Wenaweser P, Togni M, et al. Intravascular ultrasound in very late DES-stent thrombosis (abstr). J Am Coll Cardiol. 2006;47(suppl B):9B.
10. Moreno R, Fernández C, Hernández R, et al. Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies. J Am Coll Cardiol. 2005;45(6):954-959.
11. Ellis SG, Colombo A, Grube E, et al. Incidence, timing, and correlates of stent thrombosis with the polymeric paclitaxel drug-eluting stent: A TAXUS II, IV, V, and VI meta-analysis of 3,445 patients followed for up to 3 years. J Am Coll Cardiol. 2007;49(10):1043-1051.
12. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126-2130.
13. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: A pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001;103(15):1967-1971.
14. Kotani J, Awata M, Nanto S, et al. Incomplete neointimal coverage of sirolimus-eluting stents: Angioscopic findings. J Am Coll Cardiol. 2006;47(10):2108–2111.
15. Cheneau E, Leborgne L, Mintz GS, et al. Predictors of subacute stent thrombosis: Results of a systematic intravascular ultrasound study. Circulation. 2003;108(1):43-47.
16. Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation achieved with intravascular ultrasound guidance. Circulation. 1995;91(6):1676-1688.
17. Oyabu J, Ueda Y, Ogasawara N, Okada K, Hirayama A, Kodama K. Angioscopic evaluation of neointima coverage: Sirolimus-drug eluting stent versus bare metal stent. Am Heart J. 2006;152(6):1168-1174.
18. Serruys PW, Strauss BH, Beatt KJ, et al. Angiographic follow-up after placement of a self-expanding coronary-artery stent. N Engl J Med. 1991;324(1):13-17.
19. Schatz RA, Baim DS, Leon M, et al. Clinical experience with the Palmaz-Schatz coronary stent. Initial results of a multicenter study. Circulation. 1991:83(1):148-161.
20. Fischman DL, Leon MB, Baim DS, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331(8):496-501.
21. Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331(8):489-495.
22. Leon MD, Baim DS, Gordon P, et al. Clinical and angiographic results from the STent Anticoagulation Regimen Study (STARS) (abstr). Circulation. 1996;94(suppl I):I-685.
23. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: A report of the American College of Cardiology Foundation/American Heart Association Task Force of Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44-e122.
24. Bennett CL, Davidson CJ, Raisch DW, Weinberg PD, Bennett RH, Feldman MD. Thrombotic thrombocytopenic purpura associated with ticlopidine in the setting of coronary artery stents and stroke prevention. Arch Intern Med. 1999;159(21):2524-2528.
25. Bertrand ME, Rupprecht HJ, Urban P, Gershlick AH; CLASSICS Investigators. Double-blind study of the safety of clopidogrel with and without a loading dose in combination with aspirin compared with ticlopidine in combination with aspirin after coronary stenting: The clopidogrel aspirin stent international cooperative study (CLASSICS). Circulation. 2000;102(6):624-629.
26. Wang, TH, Bhatt DL, Topol EJ. Aspirin and clopidogrel resistance: An emerging clinical entity. Eur Heart J. 2006;27(6):647-654.
27. Vats HS, Hocking WG, Rezkalla SH. Suspected clopidogrel resistance in a patient with acute stent thrombosis. Nat Clin Pract Cardiovasc Med. 2006;3(4):226-230.
28. Gurbel PA, Becker RC, Mann KG, Steinhubl SR, Michelson AD. Platelet function monitoring in patients with coronary artery disease. J Am Coll Cardiol. 2007;50(19):1822-1834.
29. Fitzgerald DJ, Maree A. Aspirin and clopidogrel resistance. Hematology Am Soc Hematol Educ Program. 2007;2007(1):114-120.
30. Cattaneo M. Resistance to antiplatelet drugs: Molecular mechanisms and laboratory detection. J Thromb Haemost. 2007;5(suppl 1):230-237.
31. Trenk D, Hochholzer W, Fromm MF, et al. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008;51(20):1925-1934.
32. Kazui M, Nishiya Y, Ishizuka T, et al. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos. 2010;38(1):92-99.
33. Hulot JS, Bura A, Villard E, et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood. 2006;108(7):2244-2247.
34. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360(4):354-362.
35. U.S. Food and Drug Administration. Plavix (clopidogrel): Reduced effectiveness in patients who are poor metabolizers of the drug. U.S. Food and Drug Administration Website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm204256.htm. Updated September 6, 2013. Accessed September 4, 2014.
36. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Intensive oral antiplatelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary syndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: A subanalysis of a randomised trial. Lancet. 2008;371(9621):1353-1363.
37. Wallentin L, Becker RC, Budaj A, et al; PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
38. Wallentin L, Varenhorst C, James S, et al. Prasugrel achieves greater and faster P2Y12 receptor-mediated platelet inhibition than clopidogrel due to more efficient generation of its active metabolite in aspirin-treated patients with coronary artery disease. Eur Heart J. 2008;29(1):21-30.
39. Gurbel PA, Bliden KP, Butler K, et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: The ONSET/OFFSET study. Circulation. 2009;120(25):2577-2585.
40. Wiviott SD, Trenk D, Frelinger AL, et al; PRINCIPLE-TIMI 44 Investigators. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: The Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007;116(25):2923-2932.
41. Gurbel PA, Bliden KP, Butler K, et al. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: The RESPOND study. Circulation. 2010;121(10):1188-1199.
42. Spertus, JA, Kettelkamp R, Vance C, et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: Results from the PREMIER registry. Circulation. 2006;113(24):2803-2809.
43. Sharma AK, Ajani AE, Hamwi SM, et al. Major noncardiac surgery following coronary stenting: When is it safe to operate? Catheter Cardiovasc Interv. 2004;63(2):141-145.
44. Ben-Dor I, Torguson R, Scheinowitz M, et al. Incidence, correlates, and clinical impact of nuisance bleeding after antiplatelet therapy for patients with drug-eluting stents. Am Heart J. 2010;159(5):871-875.
45. Kaluza GL, Joseph J, Lee JR, Raizner ME, Raizner AE. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000;35(5):1288-1294.
46. Airoldi F, Colombo A, Morici N, et al. Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation. 2007;116(7):745-754.
47. Grines CL, Bonow RO, Casey DE Jr, et al; American Heart Association; American College of Cardiology; Society for Cardiovascular Angiography and Interventions; American College of Surgeons; American Dental Association; American College of Physicians. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: A science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49(6):734-739.