User login
Alcohol dependence is not an acute illness. Progression from alcohol use to dependence typically takes years, and alcohol dependence is a chronic illness with symptom severity that increases over time.1,2 As the level of alcohol intake increases, the probability of developing an alcohol use disorder, cirrhosis, seizures, cancer, hypertension, stroke, and injuries significantly increases.3,4 Most alcohol-related harm occurs in high-risk drinkers who do not meet DSM-IV-TR criteria for an alcohol use disorder.5,6
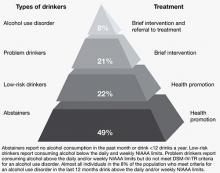
Clinicians therefore have an opportunity to intervene at early stages of alcohol use to help prevent progression to dependence and reduce harm. The concept of a continuum from low-to high-risk alcohol use is replacing the disease-oriented model that focuses on identifying and treating individuals who meet DSM-IV-TR criteria for alcohol use disorders (Figure 1).4,7 Efforts to provide screening and intervention earlier in the disease course have:
- mainly been carried out in the primary care setting
- been aimed at nontreatment-seeking, nondependent individuals
- led to recommendations for safe alcohol consumption limits.8-10
One of the largest outreach efforts is a federally funded screening, brief intervention, referral to treatment (SBIRT) program established in 17 states that targets hospital emergency rooms, community health centers, and trauma centers.11
Although research on the use of brief interventions for problem drinking in psychiatric settings is limited,12-15 psychiatrists can employ these strategies, even during a brief medication management visit.
Figure 1: Recommended treatment based on type of alcohol use
NIAAA: National Institute on Alcohol Abuse and Alcoholism
Source: References 7,16
How much is too much?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommends men age <65 drink no more than 4 drinks/day and no more than 14 drinks/week and women of any age and men age ≥65 drink no more than 3 drinks/day and no more than 7 drinks/week.16 A standard drink is defined as 14 grams of absolute ethanol (12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits). Drinking above these levels is likely to result in harm and is defined as hazardous or at-risk use.10,17,18 Harmful use is alcohol consumption that has resulted in adverse mental or physical effects.10,17,18 We use “problem drinking” to describe both at-risk and harmful use as alcohol intake that exceeds NIAAA-recommended limits but does not meet DSM-IV-TR criteria for an alcohol use disorder.
In the United States, approximately 20% of the population exceeds NIAAA recommended alcohol intake guidelines without meeting criteria for an alcohol use disorder.18 Problem drinkers have an increased risk of developing an alcohol use disorder, nicotine dependence, liver disease, financial problems, marital disruptions, injuries, and driver’s license suspensions.4-6,19
Problem drinking is common in psychiatric populations and may lead to difficulties beyond those experienced in the general population.20,21 For example, problem drinking in individuals with bipolar disorder is associated with reduced medication compliance, greater functional impairment, and possibly more suicide attempts.22,23 Even moderate alcohol use below the NIAAA-recommend levels may increase symptom severity in patients with bipolar disorder.22,23
Interviewing techniques
Interventions to identify and treat problem drinkers have focused on the primary care setting because these physicians often are the only medical professionals problem drinkers encounter.8-10 The style of counseling is based on motivational interviewing. Providers use therapeutic empathy, describe risk, deal with ambivalence and resistance, assess motivation to change, emphasize patient responsibility and self-efficacy, and provide a menu of specific strategies to reduce alcohol use. However, unlike standard motivational interviewing, in brief interventions, providers use clear, directive advice to reduce alcohol consumption in the context of the medical provider role. Brief interventions also draw on cognitive-behavioral therapy and general education strategies utilizing contracting, goal setting, and written materials such as self-help manuals.24
Clinicians’ time demands have driven an effort to make interventions for problem drinkers efficient and time-limited. A single short intervention (5 to 15 minutes) can be effective, but 2 to 4 sessions of 5 to 15 minutes each seems to be more effective.8,10 The emphasis is on increasing a patient’s insight and awareness of risk to prompt him or her to establish and manage a goal to reduce alcohol intake. As opposed to abstinence, which is commonly recommended for patients with alcohol use disorders, reducing intake typically is encouraged for problem drinkers.9,10,16,18 For patients who use alcohol over the recommended limits and also meet criteria for an alcohol use disorder, clinicians can deliver a brief intervention, but should recommend abstinence from drinking and provide referral for further treatment.9,10,16,18
Compared with controls, problem drinkers who receive a brief intervention are twice as likely to moderate their drinking at 6 to 12 months25 and significantly reduce alcohol intake by approximately 4 drinks per week at follow-ups of 12 months or more.8,10,26 In addition, providing brief interventions significantly decreases the proportion of individuals whose alcohol intake exceeds recommended levels.10 A meta-analysis and a systemic review indicate brief interventions for problem drinkers reduce morbidity and mortality resulting from motor vehicle crashes, falls, suicide attempts, domestic violence, assaults, and child abuse.5,27
A brief intervention
Screening and brief intervention guidelines suggest a standard approach for assessing and managing problem drinking and alcohol use disorders.7,16 This approach can be described by the “5 As of intervention” (Table 1),10 which is one way to summarize the different brief intervention strategies described in the literature.7,9,10,16-18,28-30
Ask. Asking a question about any alcohol use is a simple way to initiate a conversation about the topic (“Do you sometimes drink beer, wine, or other alcoholic beverages?”). Incorporating questions about alcohol consumption into inquiries about other health habits (eg, smoking, exercise) may decrease patients’ defensiveness. If your patient reports using alcohol, follow up by screening for ≥5 drinks a day for men or ≥4 drinks a day for women (“In the past year, how many times have you had 5 or more drinks a day?”). Use at this level ≥1 times a year indicates a positive screen that provides good sensitivity and specificity for detecting problem drinking and alcohol use disorders.18 Then ask about weekly alcohol intake (“On average, how many days a week do you have an alcoholic drink?” “On a typical drinking day how many drinks do you have?”). Presenting a chart that describes what constitutes a standard drink—available from the NIAAA (see Related Resources)—may be helpful.
You also can use additional questions from the CAGE screening test (Table 2).31 In clinics with a more formal screening protocol, patients may be asked to complete a written self-report such as the Alcohol Use Disorders Identification Test (AUDIT). This 10-question survey covers domains of alcohol consumption, drinking behavior, and alcohol-related problems.17,18 If your patient is a problem drinker, further assessment could determine if he or she has an alcohol use disorder.
Advise. Provide feedback about your patient’s drinking and its consequences along with clear recommendations in an empathic, nonconfrontational manner (“You’re drinking more than is medically safe; I strongly recommend you cut down”). Comparing your patient’s drinking pattern to population norms may be helpful (“Less than 20% of people drink a much as you”).7,16 When possible, tie the consequences of the patient’s drinking to his or her current physical, mental, family, social, and legal concerns. Convey your concerns empathically, as a medical provider providing health recommendations (“As your doctor, I am concerned about how much you drink and how it is affecting your health”). However, to respect patient autonomy, give a medical recommendation, rather than a directive (“As your doctor, I feel I should tell you” rather than “You should”). Finally, express a clear message of your willingness to help.
Assess your patient’s readiness to change (“Given what we’ve talked about, are you willing to consider making changes in your drinking?”). Showing the links between alcohol use and personal consequences may improve patient engagement (“If you keep drinking at your current levels, do you think your goal of improving your grades will be easier, harder, or no different?”).28 If your patient is willing to make a change, negotiate a patient-specific goal, such as reducing drinking to within the recommended limits, using alcohol only a few days a week instead of every day, or abstaining for a defined period. If the patient is not willing to change, restate your concern regarding his or her health-related consequences and your willingness to help.
Assist. After you’ve negotiated a goal with your patient, discuss a treatment plan to help the patient achieve the goal. This should include steps the patient will take to reduce or quit drinking. Consider offering handouts on standard drink sizes, alcohol-associated harms, and strategies for cutting down or abstaining (eg, pacing use, spacing drinks by including nonalcoholic beverages, plans to handle urges, using alcohol money for other items), and calendars for tracking drinking (ie, a drinking diary). Help your patient identify situations where he or she is likely to have difficulty achieving the goal and strategies for avoiding or managing such situations. Ask patients to identify a family member or friend who can help them. Refer patients who have an alcohol use disorder to addiction treatment.
For patients who are not willing to change, discuss the perceived benefits of continued drinking vs reducing or stopping drinking to encourage them to reflect on their alcohol use patterns. Discuss any potential barriers to change. Keep in mind ambivalence and reluctance to change drinking patterns are common and many patients are unaware of the risks of their alcohol use. This discussion may lead patients to contemplate change later.
Arrange. Schedule a follow-up appointment to reinforce the treatment plan with further support, feedback, and assistance in setting, achieving, and maintaining realistic goals. Consider a follow-up phone call 2 weeks after the brief intervention to check on progress and a follow-up appointment in 1 month. Clinical staff may have the opportunity to e-mail or text message patients to check on progress between face-to-face visits. At the follow-up appointment, ask if your patient was able to meet and sustain the drinking goal. If so, support continued adherence, renegotiate drinking goals if indicated, and encourage follow-up with at least annual rescreening. When patients are unable to meet their treatment goals, acknowledge that change is difficult, encourage any positive changes, and address barriers to reaching the goal. Reemphasize your willingness to help, reevaluate the diagnosis, treatment plan, and goals, and schedule close follow-up. Consider engaging significant others in the treatment process.
Table 1
Brief interventions: ‘5As’ to address alcohol use
Ask: Screen for use
|
Advise: Provide strong direct personal advice to change
|
Assess: Determine willingness to change
|
Assist: Help the patient make a change if he or she is ready
|
Arrange: Reinforce change effort with follow-up
|
| Source: Reference 10 |
Table 2
CAGE questionnaire to detect alcohol use disorders
| Cut down | ‘Have you ever felt you ought to cut down on your drinking?’ |
| Annoyed | ‘Have people annoyed you by criticizing your drinking?’ |
| Guilt | ‘Have you ever felt bad or guilty about your drinking?’ |
| Eye-opener | ‘Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?’ |
| Source: Reference 31 | |
Use in psychiatric practice
Problem drinking may not be adequately addressed in psychiatric settings. In a survey of problem drinkers identified in the general population, only 64% discussed their drinking during a mental health visit and only 40% received counseling about their alcohol use from their mental health provider.32 In a study of 200 psychiatric inpatients, 49% exhibited problem drinking as measured by AUDIT, but only 27% of patients had alcohol use recorded in their medical record.33 In addition, routine use of screening tools such as CAGE or AUDIT appears to be low in many psychiatric settings even though research has shown that tools such as AUDIT or computerized screening may be effective for identifying problem drinking in psychiatric outpatient settings.20,21,34
Several small studies support the efficacy of brief interventions for problem drinking in psychiatric settings. A study in a psychiatric emergency service found patients with either schizophrenia/bipolar disorder or depression/anxiety decreased their drinking by about 7 drinks a week over 6 months after a brief intervention.15 This study was small and the decrease in alcohol intake was not significant within the 2 population groups (P = .10 for schizophrenia/bipolar disorder, n = 34, P = .05 for depression/anxiety, n = 53); however, there was a significant decrease for all patients with follow-up (P = .0096, N = 55).15 In another study, psychiatric inpatients with problem drinking who received a brief motivational intervention demonstrated a statistically significant reduction in alcohol consumption at 6 months compared with patients who received only an information packet,13 but health-related outcomes at 5 years did not differ between the 2 groups.14 Finally, in a study of 344 nonpsychotic psychiatric outpatients with problem drinking, one-half of those who received a brief telephone intervention reduced their drinking to non-hazardous levels at a 6-month follow-up (intervention 43.8%, control 27.7%).12
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction. 1993;88(6):791-804.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Schuckit MA, Anthenelli RM, Bucholz KK, et al. The time course of development of alcohol-related problems in men and women. J Stud Alcohol. 1995;56(2):218-225.
2. Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana cocaine, and alcohol. Neuropsychopharmacology. 2002;26(4):479-488.
3. Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209-1228.
4. Dawson DA, Li TK, Grant BF. A prospective study of risk drinking: at risk for what? Drug Alcohol Depend. 2008;95(1-2):62-72.
5. Dinh-Zarr T, Goss C, Heitman E, et al. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2004;(3):CD001857.-
6. Bradley KA, Donovan DM, Larson EB. How much is too much? Advising patients about safe levels of alcohol consumption. Arch Intern Med. 1993;153(24):2734-2740.
7. Babor TF, Higgins-Biddle JC. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. World Health Organization. http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6b.pdf. Accessed August 18 2011.
8. Kaner EF, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28(3):301-323.
9. Fleming M, Manwell LB. Brief intervention in primary care settings. A primary treatment method for at-risk problem, and dependent drinkers. Alcohol Res Health. 1999;23(2):128-137.
10. Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-568.
11. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1-3):280-295.
12. Eberhard S, Nordström G, Höglund P, et al. Secondary prevention of hazardous alcohol consumption in psychiatric out-patients: a randomised controlled study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(12):1013-1021.
13. Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev. 2002;21(2):105-112.
14. Hulse GK, Tait RJ. Five-year outcomes of a brief alcohol intervention for adult in-patients with psychiatric disorders. Addiction. 2003;98(8):1061-1068.
15. Milner KK, Barry KL, Blow FC, et al. Brief interventions for patients presenting to the Psychiatric Emergency Service (PES) with major mental illnesses and at-risk drinking. Community Ment Health J. 2010;46(2):149-155.
16. U.S. Department of Health and Human Services. Helping patients who drink too much: a clinician’s guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Updated 2005. Accessed August 18, 2011.
17. Fiellin DA, Reid MC, O’Connor PG. Outpatient management of patients with alcohol problems. Ann Intern Med. 2000;133(10):815-827.
18. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: an evidence-based guide for primary care clinicians. Am Fam Physician. 2009;80(1):44-50.
19. Batty GD, Lewars H, Emslie C, et al. Internationally recognized guidelines for ‘sensible’ alcohol consumption: is exceeding them actually detrimental to health and social circumstances? Evidence from a population-based cohort study. J Public Health (Oxf). 2009;31(3):360-365.
20. Barry KL, Milner K, Blow FC, et al. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatr Serv. 2006;57(7):1039-1042.
21. Satre D, Wolfe W, Eisendrath S, et al. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatr Serv. 2008;59(4):441-444.
22. Goldstein BI, Velyvis VP, Parikh SV. The association between moderate alcohol use and illness severity in bipolar disorder: a preliminary report. J Clin Psychiatry. 2006;67(1):102-106.
23. Lagerberg TV, Andreassen OA, Ringen PA, et al. Excessive substance use in bipolar disorder is associated with impaired functioning rather than clinical characteristics, a descriptive study. BMC Psychiatry. 2010;10:9.-
24. Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. J Stud Alcohol Drugs. 2010;71(1):23-31.
25. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12(5):274-283.
26. Bertholet N, Daeppen JB, Wietlisbach V, et al. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986-995.
27. Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99(7):839-845.
28. Grossberg P, Halperin A, Mackenzie S, et al. Inside the physician’s black bag: critical ingredients of brief alcohol interventions. Subst Abus. 2010;31(4):240-250.
29. D’Onofrio G, Pantalon MV, Degutis LC, et al. Development and implementation of an emergency practitioner-performed brief intervention for hazardous and harmful drinkers in the emergency department. Acad Emerg Med. 2005;12(3):249-256.
30. Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279-292.
31. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905-1907.
32. Weisner C, Matzger H. Missed opportunities in addressing drinking behavior in medical and mental health services. Alcohol Clin Exp Res. 2003;27(7):1132-1141.
33. Barnaby B, Drummond C, McCloud A, et al. Substance misuse in psychiatric inpatients: comparison of a screening questionnaire survey with case notes. BMJ. 2003;327(7418):783-784.
34. Freimuth M. Another missed opportunity? Recognition of alcohol use problems by mental health providers. Psychotherapy: Theory Research, Practice, Training. 2008;45(3):405-409.
Alcohol dependence is not an acute illness. Progression from alcohol use to dependence typically takes years, and alcohol dependence is a chronic illness with symptom severity that increases over time.1,2 As the level of alcohol intake increases, the probability of developing an alcohol use disorder, cirrhosis, seizures, cancer, hypertension, stroke, and injuries significantly increases.3,4 Most alcohol-related harm occurs in high-risk drinkers who do not meet DSM-IV-TR criteria for an alcohol use disorder.5,6
Clinicians therefore have an opportunity to intervene at early stages of alcohol use to help prevent progression to dependence and reduce harm. The concept of a continuum from low-to high-risk alcohol use is replacing the disease-oriented model that focuses on identifying and treating individuals who meet DSM-IV-TR criteria for alcohol use disorders (Figure 1).4,7 Efforts to provide screening and intervention earlier in the disease course have:
- mainly been carried out in the primary care setting
- been aimed at nontreatment-seeking, nondependent individuals
- led to recommendations for safe alcohol consumption limits.8-10
One of the largest outreach efforts is a federally funded screening, brief intervention, referral to treatment (SBIRT) program established in 17 states that targets hospital emergency rooms, community health centers, and trauma centers.11
Although research on the use of brief interventions for problem drinking in psychiatric settings is limited,12-15 psychiatrists can employ these strategies, even during a brief medication management visit.
Figure 1: Recommended treatment based on type of alcohol use
NIAAA: National Institute on Alcohol Abuse and Alcoholism
Source: References 7,16
How much is too much?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommends men age <65 drink no more than 4 drinks/day and no more than 14 drinks/week and women of any age and men age ≥65 drink no more than 3 drinks/day and no more than 7 drinks/week.16 A standard drink is defined as 14 grams of absolute ethanol (12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits). Drinking above these levels is likely to result in harm and is defined as hazardous or at-risk use.10,17,18 Harmful use is alcohol consumption that has resulted in adverse mental or physical effects.10,17,18 We use “problem drinking” to describe both at-risk and harmful use as alcohol intake that exceeds NIAAA-recommended limits but does not meet DSM-IV-TR criteria for an alcohol use disorder.
In the United States, approximately 20% of the population exceeds NIAAA recommended alcohol intake guidelines without meeting criteria for an alcohol use disorder.18 Problem drinkers have an increased risk of developing an alcohol use disorder, nicotine dependence, liver disease, financial problems, marital disruptions, injuries, and driver’s license suspensions.4-6,19
Problem drinking is common in psychiatric populations and may lead to difficulties beyond those experienced in the general population.20,21 For example, problem drinking in individuals with bipolar disorder is associated with reduced medication compliance, greater functional impairment, and possibly more suicide attempts.22,23 Even moderate alcohol use below the NIAAA-recommend levels may increase symptom severity in patients with bipolar disorder.22,23
Interviewing techniques
Interventions to identify and treat problem drinkers have focused on the primary care setting because these physicians often are the only medical professionals problem drinkers encounter.8-10 The style of counseling is based on motivational interviewing. Providers use therapeutic empathy, describe risk, deal with ambivalence and resistance, assess motivation to change, emphasize patient responsibility and self-efficacy, and provide a menu of specific strategies to reduce alcohol use. However, unlike standard motivational interviewing, in brief interventions, providers use clear, directive advice to reduce alcohol consumption in the context of the medical provider role. Brief interventions also draw on cognitive-behavioral therapy and general education strategies utilizing contracting, goal setting, and written materials such as self-help manuals.24
Clinicians’ time demands have driven an effort to make interventions for problem drinkers efficient and time-limited. A single short intervention (5 to 15 minutes) can be effective, but 2 to 4 sessions of 5 to 15 minutes each seems to be more effective.8,10 The emphasis is on increasing a patient’s insight and awareness of risk to prompt him or her to establish and manage a goal to reduce alcohol intake. As opposed to abstinence, which is commonly recommended for patients with alcohol use disorders, reducing intake typically is encouraged for problem drinkers.9,10,16,18 For patients who use alcohol over the recommended limits and also meet criteria for an alcohol use disorder, clinicians can deliver a brief intervention, but should recommend abstinence from drinking and provide referral for further treatment.9,10,16,18
Compared with controls, problem drinkers who receive a brief intervention are twice as likely to moderate their drinking at 6 to 12 months25 and significantly reduce alcohol intake by approximately 4 drinks per week at follow-ups of 12 months or more.8,10,26 In addition, providing brief interventions significantly decreases the proportion of individuals whose alcohol intake exceeds recommended levels.10 A meta-analysis and a systemic review indicate brief interventions for problem drinkers reduce morbidity and mortality resulting from motor vehicle crashes, falls, suicide attempts, domestic violence, assaults, and child abuse.5,27
A brief intervention
Screening and brief intervention guidelines suggest a standard approach for assessing and managing problem drinking and alcohol use disorders.7,16 This approach can be described by the “5 As of intervention” (Table 1),10 which is one way to summarize the different brief intervention strategies described in the literature.7,9,10,16-18,28-30
Ask. Asking a question about any alcohol use is a simple way to initiate a conversation about the topic (“Do you sometimes drink beer, wine, or other alcoholic beverages?”). Incorporating questions about alcohol consumption into inquiries about other health habits (eg, smoking, exercise) may decrease patients’ defensiveness. If your patient reports using alcohol, follow up by screening for ≥5 drinks a day for men or ≥4 drinks a day for women (“In the past year, how many times have you had 5 or more drinks a day?”). Use at this level ≥1 times a year indicates a positive screen that provides good sensitivity and specificity for detecting problem drinking and alcohol use disorders.18 Then ask about weekly alcohol intake (“On average, how many days a week do you have an alcoholic drink?” “On a typical drinking day how many drinks do you have?”). Presenting a chart that describes what constitutes a standard drink—available from the NIAAA (see Related Resources)—may be helpful.
You also can use additional questions from the CAGE screening test (Table 2).31 In clinics with a more formal screening protocol, patients may be asked to complete a written self-report such as the Alcohol Use Disorders Identification Test (AUDIT). This 10-question survey covers domains of alcohol consumption, drinking behavior, and alcohol-related problems.17,18 If your patient is a problem drinker, further assessment could determine if he or she has an alcohol use disorder.
Advise. Provide feedback about your patient’s drinking and its consequences along with clear recommendations in an empathic, nonconfrontational manner (“You’re drinking more than is medically safe; I strongly recommend you cut down”). Comparing your patient’s drinking pattern to population norms may be helpful (“Less than 20% of people drink a much as you”).7,16 When possible, tie the consequences of the patient’s drinking to his or her current physical, mental, family, social, and legal concerns. Convey your concerns empathically, as a medical provider providing health recommendations (“As your doctor, I am concerned about how much you drink and how it is affecting your health”). However, to respect patient autonomy, give a medical recommendation, rather than a directive (“As your doctor, I feel I should tell you” rather than “You should”). Finally, express a clear message of your willingness to help.
Assess your patient’s readiness to change (“Given what we’ve talked about, are you willing to consider making changes in your drinking?”). Showing the links between alcohol use and personal consequences may improve patient engagement (“If you keep drinking at your current levels, do you think your goal of improving your grades will be easier, harder, or no different?”).28 If your patient is willing to make a change, negotiate a patient-specific goal, such as reducing drinking to within the recommended limits, using alcohol only a few days a week instead of every day, or abstaining for a defined period. If the patient is not willing to change, restate your concern regarding his or her health-related consequences and your willingness to help.
Assist. After you’ve negotiated a goal with your patient, discuss a treatment plan to help the patient achieve the goal. This should include steps the patient will take to reduce or quit drinking. Consider offering handouts on standard drink sizes, alcohol-associated harms, and strategies for cutting down or abstaining (eg, pacing use, spacing drinks by including nonalcoholic beverages, plans to handle urges, using alcohol money for other items), and calendars for tracking drinking (ie, a drinking diary). Help your patient identify situations where he or she is likely to have difficulty achieving the goal and strategies for avoiding or managing such situations. Ask patients to identify a family member or friend who can help them. Refer patients who have an alcohol use disorder to addiction treatment.
For patients who are not willing to change, discuss the perceived benefits of continued drinking vs reducing or stopping drinking to encourage them to reflect on their alcohol use patterns. Discuss any potential barriers to change. Keep in mind ambivalence and reluctance to change drinking patterns are common and many patients are unaware of the risks of their alcohol use. This discussion may lead patients to contemplate change later.
Arrange. Schedule a follow-up appointment to reinforce the treatment plan with further support, feedback, and assistance in setting, achieving, and maintaining realistic goals. Consider a follow-up phone call 2 weeks after the brief intervention to check on progress and a follow-up appointment in 1 month. Clinical staff may have the opportunity to e-mail or text message patients to check on progress between face-to-face visits. At the follow-up appointment, ask if your patient was able to meet and sustain the drinking goal. If so, support continued adherence, renegotiate drinking goals if indicated, and encourage follow-up with at least annual rescreening. When patients are unable to meet their treatment goals, acknowledge that change is difficult, encourage any positive changes, and address barriers to reaching the goal. Reemphasize your willingness to help, reevaluate the diagnosis, treatment plan, and goals, and schedule close follow-up. Consider engaging significant others in the treatment process.
Table 1
Brief interventions: ‘5As’ to address alcohol use
Ask: Screen for use
|
Advise: Provide strong direct personal advice to change
|
Assess: Determine willingness to change
|
Assist: Help the patient make a change if he or she is ready
|
Arrange: Reinforce change effort with follow-up
|
| Source: Reference 10 |
Table 2
CAGE questionnaire to detect alcohol use disorders
| Cut down | ‘Have you ever felt you ought to cut down on your drinking?’ |
| Annoyed | ‘Have people annoyed you by criticizing your drinking?’ |
| Guilt | ‘Have you ever felt bad or guilty about your drinking?’ |
| Eye-opener | ‘Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?’ |
| Source: Reference 31 | |
Use in psychiatric practice
Problem drinking may not be adequately addressed in psychiatric settings. In a survey of problem drinkers identified in the general population, only 64% discussed their drinking during a mental health visit and only 40% received counseling about their alcohol use from their mental health provider.32 In a study of 200 psychiatric inpatients, 49% exhibited problem drinking as measured by AUDIT, but only 27% of patients had alcohol use recorded in their medical record.33 In addition, routine use of screening tools such as CAGE or AUDIT appears to be low in many psychiatric settings even though research has shown that tools such as AUDIT or computerized screening may be effective for identifying problem drinking in psychiatric outpatient settings.20,21,34
Several small studies support the efficacy of brief interventions for problem drinking in psychiatric settings. A study in a psychiatric emergency service found patients with either schizophrenia/bipolar disorder or depression/anxiety decreased their drinking by about 7 drinks a week over 6 months after a brief intervention.15 This study was small and the decrease in alcohol intake was not significant within the 2 population groups (P = .10 for schizophrenia/bipolar disorder, n = 34, P = .05 for depression/anxiety, n = 53); however, there was a significant decrease for all patients with follow-up (P = .0096, N = 55).15 In another study, psychiatric inpatients with problem drinking who received a brief motivational intervention demonstrated a statistically significant reduction in alcohol consumption at 6 months compared with patients who received only an information packet,13 but health-related outcomes at 5 years did not differ between the 2 groups.14 Finally, in a study of 344 nonpsychotic psychiatric outpatients with problem drinking, one-half of those who received a brief telephone intervention reduced their drinking to non-hazardous levels at a 6-month follow-up (intervention 43.8%, control 27.7%).12
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction. 1993;88(6):791-804.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Alcohol dependence is not an acute illness. Progression from alcohol use to dependence typically takes years, and alcohol dependence is a chronic illness with symptom severity that increases over time.1,2 As the level of alcohol intake increases, the probability of developing an alcohol use disorder, cirrhosis, seizures, cancer, hypertension, stroke, and injuries significantly increases.3,4 Most alcohol-related harm occurs in high-risk drinkers who do not meet DSM-IV-TR criteria for an alcohol use disorder.5,6
Clinicians therefore have an opportunity to intervene at early stages of alcohol use to help prevent progression to dependence and reduce harm. The concept of a continuum from low-to high-risk alcohol use is replacing the disease-oriented model that focuses on identifying and treating individuals who meet DSM-IV-TR criteria for alcohol use disorders (Figure 1).4,7 Efforts to provide screening and intervention earlier in the disease course have:
- mainly been carried out in the primary care setting
- been aimed at nontreatment-seeking, nondependent individuals
- led to recommendations for safe alcohol consumption limits.8-10
One of the largest outreach efforts is a federally funded screening, brief intervention, referral to treatment (SBIRT) program established in 17 states that targets hospital emergency rooms, community health centers, and trauma centers.11
Although research on the use of brief interventions for problem drinking in psychiatric settings is limited,12-15 psychiatrists can employ these strategies, even during a brief medication management visit.
Figure 1: Recommended treatment based on type of alcohol use
NIAAA: National Institute on Alcohol Abuse and Alcoholism
Source: References 7,16
How much is too much?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommends men age <65 drink no more than 4 drinks/day and no more than 14 drinks/week and women of any age and men age ≥65 drink no more than 3 drinks/day and no more than 7 drinks/week.16 A standard drink is defined as 14 grams of absolute ethanol (12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits). Drinking above these levels is likely to result in harm and is defined as hazardous or at-risk use.10,17,18 Harmful use is alcohol consumption that has resulted in adverse mental or physical effects.10,17,18 We use “problem drinking” to describe both at-risk and harmful use as alcohol intake that exceeds NIAAA-recommended limits but does not meet DSM-IV-TR criteria for an alcohol use disorder.
In the United States, approximately 20% of the population exceeds NIAAA recommended alcohol intake guidelines without meeting criteria for an alcohol use disorder.18 Problem drinkers have an increased risk of developing an alcohol use disorder, nicotine dependence, liver disease, financial problems, marital disruptions, injuries, and driver’s license suspensions.4-6,19
Problem drinking is common in psychiatric populations and may lead to difficulties beyond those experienced in the general population.20,21 For example, problem drinking in individuals with bipolar disorder is associated with reduced medication compliance, greater functional impairment, and possibly more suicide attempts.22,23 Even moderate alcohol use below the NIAAA-recommend levels may increase symptom severity in patients with bipolar disorder.22,23
Interviewing techniques
Interventions to identify and treat problem drinkers have focused on the primary care setting because these physicians often are the only medical professionals problem drinkers encounter.8-10 The style of counseling is based on motivational interviewing. Providers use therapeutic empathy, describe risk, deal with ambivalence and resistance, assess motivation to change, emphasize patient responsibility and self-efficacy, and provide a menu of specific strategies to reduce alcohol use. However, unlike standard motivational interviewing, in brief interventions, providers use clear, directive advice to reduce alcohol consumption in the context of the medical provider role. Brief interventions also draw on cognitive-behavioral therapy and general education strategies utilizing contracting, goal setting, and written materials such as self-help manuals.24
Clinicians’ time demands have driven an effort to make interventions for problem drinkers efficient and time-limited. A single short intervention (5 to 15 minutes) can be effective, but 2 to 4 sessions of 5 to 15 minutes each seems to be more effective.8,10 The emphasis is on increasing a patient’s insight and awareness of risk to prompt him or her to establish and manage a goal to reduce alcohol intake. As opposed to abstinence, which is commonly recommended for patients with alcohol use disorders, reducing intake typically is encouraged for problem drinkers.9,10,16,18 For patients who use alcohol over the recommended limits and also meet criteria for an alcohol use disorder, clinicians can deliver a brief intervention, but should recommend abstinence from drinking and provide referral for further treatment.9,10,16,18
Compared with controls, problem drinkers who receive a brief intervention are twice as likely to moderate their drinking at 6 to 12 months25 and significantly reduce alcohol intake by approximately 4 drinks per week at follow-ups of 12 months or more.8,10,26 In addition, providing brief interventions significantly decreases the proportion of individuals whose alcohol intake exceeds recommended levels.10 A meta-analysis and a systemic review indicate brief interventions for problem drinkers reduce morbidity and mortality resulting from motor vehicle crashes, falls, suicide attempts, domestic violence, assaults, and child abuse.5,27
A brief intervention
Screening and brief intervention guidelines suggest a standard approach for assessing and managing problem drinking and alcohol use disorders.7,16 This approach can be described by the “5 As of intervention” (Table 1),10 which is one way to summarize the different brief intervention strategies described in the literature.7,9,10,16-18,28-30
Ask. Asking a question about any alcohol use is a simple way to initiate a conversation about the topic (“Do you sometimes drink beer, wine, or other alcoholic beverages?”). Incorporating questions about alcohol consumption into inquiries about other health habits (eg, smoking, exercise) may decrease patients’ defensiveness. If your patient reports using alcohol, follow up by screening for ≥5 drinks a day for men or ≥4 drinks a day for women (“In the past year, how many times have you had 5 or more drinks a day?”). Use at this level ≥1 times a year indicates a positive screen that provides good sensitivity and specificity for detecting problem drinking and alcohol use disorders.18 Then ask about weekly alcohol intake (“On average, how many days a week do you have an alcoholic drink?” “On a typical drinking day how many drinks do you have?”). Presenting a chart that describes what constitutes a standard drink—available from the NIAAA (see Related Resources)—may be helpful.
You also can use additional questions from the CAGE screening test (Table 2).31 In clinics with a more formal screening protocol, patients may be asked to complete a written self-report such as the Alcohol Use Disorders Identification Test (AUDIT). This 10-question survey covers domains of alcohol consumption, drinking behavior, and alcohol-related problems.17,18 If your patient is a problem drinker, further assessment could determine if he or she has an alcohol use disorder.
Advise. Provide feedback about your patient’s drinking and its consequences along with clear recommendations in an empathic, nonconfrontational manner (“You’re drinking more than is medically safe; I strongly recommend you cut down”). Comparing your patient’s drinking pattern to population norms may be helpful (“Less than 20% of people drink a much as you”).7,16 When possible, tie the consequences of the patient’s drinking to his or her current physical, mental, family, social, and legal concerns. Convey your concerns empathically, as a medical provider providing health recommendations (“As your doctor, I am concerned about how much you drink and how it is affecting your health”). However, to respect patient autonomy, give a medical recommendation, rather than a directive (“As your doctor, I feel I should tell you” rather than “You should”). Finally, express a clear message of your willingness to help.
Assess your patient’s readiness to change (“Given what we’ve talked about, are you willing to consider making changes in your drinking?”). Showing the links between alcohol use and personal consequences may improve patient engagement (“If you keep drinking at your current levels, do you think your goal of improving your grades will be easier, harder, or no different?”).28 If your patient is willing to make a change, negotiate a patient-specific goal, such as reducing drinking to within the recommended limits, using alcohol only a few days a week instead of every day, or abstaining for a defined period. If the patient is not willing to change, restate your concern regarding his or her health-related consequences and your willingness to help.
Assist. After you’ve negotiated a goal with your patient, discuss a treatment plan to help the patient achieve the goal. This should include steps the patient will take to reduce or quit drinking. Consider offering handouts on standard drink sizes, alcohol-associated harms, and strategies for cutting down or abstaining (eg, pacing use, spacing drinks by including nonalcoholic beverages, plans to handle urges, using alcohol money for other items), and calendars for tracking drinking (ie, a drinking diary). Help your patient identify situations where he or she is likely to have difficulty achieving the goal and strategies for avoiding or managing such situations. Ask patients to identify a family member or friend who can help them. Refer patients who have an alcohol use disorder to addiction treatment.
For patients who are not willing to change, discuss the perceived benefits of continued drinking vs reducing or stopping drinking to encourage them to reflect on their alcohol use patterns. Discuss any potential barriers to change. Keep in mind ambivalence and reluctance to change drinking patterns are common and many patients are unaware of the risks of their alcohol use. This discussion may lead patients to contemplate change later.
Arrange. Schedule a follow-up appointment to reinforce the treatment plan with further support, feedback, and assistance in setting, achieving, and maintaining realistic goals. Consider a follow-up phone call 2 weeks after the brief intervention to check on progress and a follow-up appointment in 1 month. Clinical staff may have the opportunity to e-mail or text message patients to check on progress between face-to-face visits. At the follow-up appointment, ask if your patient was able to meet and sustain the drinking goal. If so, support continued adherence, renegotiate drinking goals if indicated, and encourage follow-up with at least annual rescreening. When patients are unable to meet their treatment goals, acknowledge that change is difficult, encourage any positive changes, and address barriers to reaching the goal. Reemphasize your willingness to help, reevaluate the diagnosis, treatment plan, and goals, and schedule close follow-up. Consider engaging significant others in the treatment process.
Table 1
Brief interventions: ‘5As’ to address alcohol use
Ask: Screen for use
|
Advise: Provide strong direct personal advice to change
|
Assess: Determine willingness to change
|
Assist: Help the patient make a change if he or she is ready
|
Arrange: Reinforce change effort with follow-up
|
| Source: Reference 10 |
Table 2
CAGE questionnaire to detect alcohol use disorders
| Cut down | ‘Have you ever felt you ought to cut down on your drinking?’ |
| Annoyed | ‘Have people annoyed you by criticizing your drinking?’ |
| Guilt | ‘Have you ever felt bad or guilty about your drinking?’ |
| Eye-opener | ‘Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?’ |
| Source: Reference 31 | |
Use in psychiatric practice
Problem drinking may not be adequately addressed in psychiatric settings. In a survey of problem drinkers identified in the general population, only 64% discussed their drinking during a mental health visit and only 40% received counseling about their alcohol use from their mental health provider.32 In a study of 200 psychiatric inpatients, 49% exhibited problem drinking as measured by AUDIT, but only 27% of patients had alcohol use recorded in their medical record.33 In addition, routine use of screening tools such as CAGE or AUDIT appears to be low in many psychiatric settings even though research has shown that tools such as AUDIT or computerized screening may be effective for identifying problem drinking in psychiatric outpatient settings.20,21,34
Several small studies support the efficacy of brief interventions for problem drinking in psychiatric settings. A study in a psychiatric emergency service found patients with either schizophrenia/bipolar disorder or depression/anxiety decreased their drinking by about 7 drinks a week over 6 months after a brief intervention.15 This study was small and the decrease in alcohol intake was not significant within the 2 population groups (P = .10 for schizophrenia/bipolar disorder, n = 34, P = .05 for depression/anxiety, n = 53); however, there was a significant decrease for all patients with follow-up (P = .0096, N = 55).15 In another study, psychiatric inpatients with problem drinking who received a brief motivational intervention demonstrated a statistically significant reduction in alcohol consumption at 6 months compared with patients who received only an information packet,13 but health-related outcomes at 5 years did not differ between the 2 groups.14 Finally, in a study of 344 nonpsychotic psychiatric outpatients with problem drinking, one-half of those who received a brief telephone intervention reduced their drinking to non-hazardous levels at a 6-month follow-up (intervention 43.8%, control 27.7%).12
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction. 1993;88(6):791-804.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Schuckit MA, Anthenelli RM, Bucholz KK, et al. The time course of development of alcohol-related problems in men and women. J Stud Alcohol. 1995;56(2):218-225.
2. Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana cocaine, and alcohol. Neuropsychopharmacology. 2002;26(4):479-488.
3. Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209-1228.
4. Dawson DA, Li TK, Grant BF. A prospective study of risk drinking: at risk for what? Drug Alcohol Depend. 2008;95(1-2):62-72.
5. Dinh-Zarr T, Goss C, Heitman E, et al. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2004;(3):CD001857.-
6. Bradley KA, Donovan DM, Larson EB. How much is too much? Advising patients about safe levels of alcohol consumption. Arch Intern Med. 1993;153(24):2734-2740.
7. Babor TF, Higgins-Biddle JC. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. World Health Organization. http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6b.pdf. Accessed August 18 2011.
8. Kaner EF, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28(3):301-323.
9. Fleming M, Manwell LB. Brief intervention in primary care settings. A primary treatment method for at-risk problem, and dependent drinkers. Alcohol Res Health. 1999;23(2):128-137.
10. Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-568.
11. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1-3):280-295.
12. Eberhard S, Nordström G, Höglund P, et al. Secondary prevention of hazardous alcohol consumption in psychiatric out-patients: a randomised controlled study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(12):1013-1021.
13. Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev. 2002;21(2):105-112.
14. Hulse GK, Tait RJ. Five-year outcomes of a brief alcohol intervention for adult in-patients with psychiatric disorders. Addiction. 2003;98(8):1061-1068.
15. Milner KK, Barry KL, Blow FC, et al. Brief interventions for patients presenting to the Psychiatric Emergency Service (PES) with major mental illnesses and at-risk drinking. Community Ment Health J. 2010;46(2):149-155.
16. U.S. Department of Health and Human Services. Helping patients who drink too much: a clinician’s guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Updated 2005. Accessed August 18, 2011.
17. Fiellin DA, Reid MC, O’Connor PG. Outpatient management of patients with alcohol problems. Ann Intern Med. 2000;133(10):815-827.
18. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: an evidence-based guide for primary care clinicians. Am Fam Physician. 2009;80(1):44-50.
19. Batty GD, Lewars H, Emslie C, et al. Internationally recognized guidelines for ‘sensible’ alcohol consumption: is exceeding them actually detrimental to health and social circumstances? Evidence from a population-based cohort study. J Public Health (Oxf). 2009;31(3):360-365.
20. Barry KL, Milner K, Blow FC, et al. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatr Serv. 2006;57(7):1039-1042.
21. Satre D, Wolfe W, Eisendrath S, et al. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatr Serv. 2008;59(4):441-444.
22. Goldstein BI, Velyvis VP, Parikh SV. The association between moderate alcohol use and illness severity in bipolar disorder: a preliminary report. J Clin Psychiatry. 2006;67(1):102-106.
23. Lagerberg TV, Andreassen OA, Ringen PA, et al. Excessive substance use in bipolar disorder is associated with impaired functioning rather than clinical characteristics, a descriptive study. BMC Psychiatry. 2010;10:9.-
24. Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. J Stud Alcohol Drugs. 2010;71(1):23-31.
25. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12(5):274-283.
26. Bertholet N, Daeppen JB, Wietlisbach V, et al. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986-995.
27. Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99(7):839-845.
28. Grossberg P, Halperin A, Mackenzie S, et al. Inside the physician’s black bag: critical ingredients of brief alcohol interventions. Subst Abus. 2010;31(4):240-250.
29. D’Onofrio G, Pantalon MV, Degutis LC, et al. Development and implementation of an emergency practitioner-performed brief intervention for hazardous and harmful drinkers in the emergency department. Acad Emerg Med. 2005;12(3):249-256.
30. Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279-292.
31. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905-1907.
32. Weisner C, Matzger H. Missed opportunities in addressing drinking behavior in medical and mental health services. Alcohol Clin Exp Res. 2003;27(7):1132-1141.
33. Barnaby B, Drummond C, McCloud A, et al. Substance misuse in psychiatric inpatients: comparison of a screening questionnaire survey with case notes. BMJ. 2003;327(7418):783-784.
34. Freimuth M. Another missed opportunity? Recognition of alcohol use problems by mental health providers. Psychotherapy: Theory Research, Practice, Training. 2008;45(3):405-409.
1. Schuckit MA, Anthenelli RM, Bucholz KK, et al. The time course of development of alcohol-related problems in men and women. J Stud Alcohol. 1995;56(2):218-225.
2. Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana cocaine, and alcohol. Neuropsychopharmacology. 2002;26(4):479-488.
3. Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209-1228.
4. Dawson DA, Li TK, Grant BF. A prospective study of risk drinking: at risk for what? Drug Alcohol Depend. 2008;95(1-2):62-72.
5. Dinh-Zarr T, Goss C, Heitman E, et al. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2004;(3):CD001857.-
6. Bradley KA, Donovan DM, Larson EB. How much is too much? Advising patients about safe levels of alcohol consumption. Arch Intern Med. 1993;153(24):2734-2740.
7. Babor TF, Higgins-Biddle JC. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. World Health Organization. http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6b.pdf. Accessed August 18 2011.
8. Kaner EF, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28(3):301-323.
9. Fleming M, Manwell LB. Brief intervention in primary care settings. A primary treatment method for at-risk problem, and dependent drinkers. Alcohol Res Health. 1999;23(2):128-137.
10. Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-568.
11. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1-3):280-295.
12. Eberhard S, Nordström G, Höglund P, et al. Secondary prevention of hazardous alcohol consumption in psychiatric out-patients: a randomised controlled study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(12):1013-1021.
13. Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev. 2002;21(2):105-112.
14. Hulse GK, Tait RJ. Five-year outcomes of a brief alcohol intervention for adult in-patients with psychiatric disorders. Addiction. 2003;98(8):1061-1068.
15. Milner KK, Barry KL, Blow FC, et al. Brief interventions for patients presenting to the Psychiatric Emergency Service (PES) with major mental illnesses and at-risk drinking. Community Ment Health J. 2010;46(2):149-155.
16. U.S. Department of Health and Human Services. Helping patients who drink too much: a clinician’s guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Updated 2005. Accessed August 18, 2011.
17. Fiellin DA, Reid MC, O’Connor PG. Outpatient management of patients with alcohol problems. Ann Intern Med. 2000;133(10):815-827.
18. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: an evidence-based guide for primary care clinicians. Am Fam Physician. 2009;80(1):44-50.
19. Batty GD, Lewars H, Emslie C, et al. Internationally recognized guidelines for ‘sensible’ alcohol consumption: is exceeding them actually detrimental to health and social circumstances? Evidence from a population-based cohort study. J Public Health (Oxf). 2009;31(3):360-365.
20. Barry KL, Milner K, Blow FC, et al. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatr Serv. 2006;57(7):1039-1042.
21. Satre D, Wolfe W, Eisendrath S, et al. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatr Serv. 2008;59(4):441-444.
22. Goldstein BI, Velyvis VP, Parikh SV. The association between moderate alcohol use and illness severity in bipolar disorder: a preliminary report. J Clin Psychiatry. 2006;67(1):102-106.
23. Lagerberg TV, Andreassen OA, Ringen PA, et al. Excessive substance use in bipolar disorder is associated with impaired functioning rather than clinical characteristics, a descriptive study. BMC Psychiatry. 2010;10:9.-
24. Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. J Stud Alcohol Drugs. 2010;71(1):23-31.
25. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12(5):274-283.
26. Bertholet N, Daeppen JB, Wietlisbach V, et al. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986-995.
27. Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99(7):839-845.
28. Grossberg P, Halperin A, Mackenzie S, et al. Inside the physician’s black bag: critical ingredients of brief alcohol interventions. Subst Abus. 2010;31(4):240-250.
29. D’Onofrio G, Pantalon MV, Degutis LC, et al. Development and implementation of an emergency practitioner-performed brief intervention for hazardous and harmful drinkers in the emergency department. Acad Emerg Med. 2005;12(3):249-256.
30. Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279-292.
31. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905-1907.
32. Weisner C, Matzger H. Missed opportunities in addressing drinking behavior in medical and mental health services. Alcohol Clin Exp Res. 2003;27(7):1132-1141.
33. Barnaby B, Drummond C, McCloud A, et al. Substance misuse in psychiatric inpatients: comparison of a screening questionnaire survey with case notes. BMJ. 2003;327(7418):783-784.
34. Freimuth M. Another missed opportunity? Recognition of alcohol use problems by mental health providers. Psychotherapy: Theory Research, Practice, Training. 2008;45(3):405-409.